The patient presenting with non-dental orofacial pain can be one of the most challenging aspects of primary dental care and appears to be more prevalent than previously thought. Although a small part of everyday dentistry, dentists are often the first point of call for patients with orofacial pain, usually before the GP, and pain consultations can be among the most difficult to manage.
Time constraints and lack of experience in managing non-dental pain disorders are just some of the challenges faced, but a good history, along with a few simple investigations, can improve the consultation outcome, therapeutic options and, where needed, the quality of pain referrals. This article aims to help clarify some of the most common orofacial pain disorders and, where appropriate, give guidance on investigations and treatment that may be carried on in a primary care setting.
Before considering the following diagnoses, other dental and pathological sources of pain must be excluded through appropriate clinical examination and imaging. The more common non-dental orofacial pain conditions that may present to the dentist include:
- TMD
- Burning Mouth Syndrome
- Sinusitis
- Trigeminal neuralgia.
The acronym SOCRATES (Site, Onset, Character, Radiation, Associated Factors, Timing, Exacerbating/Relieving Factors and Severity) is a standardised tool for pain history and assessment endorsed by many medical and dental schools across the UK and provides a thorough and logical approach to history taking. This is as applicable to the dental practice setting as to the specialist pain clinic. Each of these features should be asked about and the response noted. Remember that the ‘absence’ of a finding can be as important as a ‘positive’ response where pain and its associated
features are concerned – both must be recorded in the notes.
Temporomandibular joint dysfunction (TMD)
Background
This is the most frequently seen non-dental pain condition presenting to the dentist. It is also one of the most varied orofacial pain disorders as it can appear in many different ways. Always consider TMD in the differential diagnosis of orofacial pain, even if the symptoms do not seem exactly to fit. This is particularly the case where the pain reported is bilateral. It is easy for the practitioner to treat in primary care and will respond promptly to the correct treatments.
Remember that for TMD:
- Clicking of the jaw in the absence of pain and locking does not require referral or treatment
- Bite splints DO work and should be tried where TMD cannot be excluded. These are now available on the NHS without prior approval. They are not effective alone for every patient, but are used together with other medical and physical therapies to good effect.
Where locking of the TMJ is the main problem, the issue is usually related to the joint itself and these patients should be referred to the local maxillofacial surgery service for assessment.
Aetiology
Parafunctional habits, such as clenching and grinding, are frequently seen in patients with TMD, although many patients also have similar habits without problems. Where pain is present, habits such as chewing gum seem to be an important trigger of pain. Unilateral chewing especially appears to be a risk factor.
Evidence of clenching can be seen from the oral soft tissues with crenulation of the tongue edge and a buccal mucosa occlusal line being common findings. Stress and emotional burden are very often cited, but will not always feature in the history unless specifically asked about by the dentist.
Figure 1
| SOCRATES in TMD | |
|---|---|
| SITE | TMJ, ears, cheeks, temple, teeth, sublingual region Unilateral or Bilateral |
| ONSET | Acute: This is less common. May be following trauma to joint/face, joint dislocation, or muscle spasm.. Chronic: Gradual onset- weeks/ months |
| CHARACTER | Dull ache Throbbing Sharp (with wide opening/ muscle spasm). Less common N.B. Pain is not pulsatile |
| RADIATION | Neck, head (headache), face, upper and lower jaws |
| ASSOCIATED FACTORS | Trismus Clicking or crepitus in TMJ (more common in older age group) Mandibular fatigue and stiffness of the jaw Extra-oral swelling caused by muscle hypertrophy Soft tissue features: linea alba and tongue scalloping |
| TIMING | Morning, during night, during stressful activities e.g. driving |
| EXACERBATING/ RELIEVING FACTORS | Chewing Yawning Playing a wind musical instrument |
| SEVERITY | Range: mild to severe |
Occlusal factors themselves seem to play a very small role in chronic TMD, although
acute changes may be found after placement of a restoration that disrupts the normal intercuspal position. However, looking at the occlusion for triggers in chronic TMD is rarely helpful and often results in destruction of dental hard tissue unnecessarily. TMD itself may in fact cause occlusal changes, as pain-induced muscle dysfunction around the joint results in altered closing patterns of the mandible and a secondary occlusal change.
There is certainly no link with orthodontics in either the origin or resolution of TMJ dysfunctions. Hypermobility of the joints, however, does show an increased probability of developing problems. This is demonstrated in studies on patients with Ehlers-Danlos syndrome, where all patients in the study experienced TMD and multiple joint dislocations.
Who is affected?
As a condition which affects 5-12 per cent of the population, these patients frequently present in dental practice. More women than men are affected by the disorder (quoted up to 4:15) and unlike other types of orofacial pain, its prevalence is higher in a younger age group, with up to 7 per cent of 12-18 year olds diagnosed with mandibular pain dysfunction. However, children and older adults are also affected, commonly with stressful life events being key precipitators.
Interestingly, women taking oral contraceptives or on supplemental oestrogen are also more likely to both suffer from TMD and to seek treatment for the condition. This is thought to be due to the presence of oestrogen receptors in the TM joints, which modify metabolic activity, affecting ligament laxity and also due to the effects of oestrogen on pain experience. There appears to be no genetic predisposition and no influence from the family environment, although many patients citing ‘stress’ as a trigger have home issues!
Examination
Palpate the muscles of mastication for evidence of pain or hypertrophy. Use forced movements of the mandible against pressure to look for pain in the medial and lateral pterygoid muscles. Palpate the TMJs in static and dynamic movements – this may elicit pain, clicking and crepitus, all of which should be noted. Measure mouth opening inter-incisally – as a single measure, this does not contribute much, but can be measured serially to look for improvements as treatment progresses.
Soft tissue features, including evidence of parafunctional clenching and tooth wear, should also be noted. If neck or shoulder pain is also present, palpate the trapezius and sterno-mastoid muscles, looking for areas of focal tenderness which might indicate referred pain from the neck to the face.
Treatment
Conservative management remains the most successful treatment for TMD and should always be tried in primary care before considering a referral. Patients must be aware of the self-limiting nature of the condition and they must understand that their role in the treatment is paramount. The success of treatment will depend upon the patient following a standardised regime:
- Medications: NSAIDs (TDS for first two weeks and as needed thereafter)
- Soft diet (liquid for first two weeks and avoidance of hard/chewy foods after)
- Localised heat (apply to affected side for five minutes TDS in evening with five minute breaks intermittent between for two weeks and as needed thereafter)
- Yawning support/avoid wide opening
- Avoidance of chewing gum/habits (e.g. nail/pen biting) and playing wind instruments.
If these simple measures fail to produce an improvement within a month, a Bite Raising Appliance (BRA) should be made and fitted. There is evidence to support the use of both soft and hard BRAs, but neither is clearly better. A soft appliance may be useful in the first instance, as is more comfortable to wear and easier to construct and fit. Some patients will find these encourage clenching; however, this does not seem to affect the success. The patient should be advised to expect this at the beginning of treatment and even some initial increase in discomfort.
Most patients will have seen a good improvement in two months of night use of a splint. In acute cases, a small dose of diazepam (2-5mg up to TDS) can be useful in conjunction with the treatments suggested above remembering to assess the impact this may have on the patient’s life and warning the patient about drowsiness and sedation from the treatment.
If there is no good improvement in this time, a referral for specialist assessment should be arranged.
Specialist referral
Onward referral to oral medicine should be made if symptoms are not improving or the symptoms are increasing despite conservative management AND provision of a BRA.
Investigations and treatment that can be carried out in specialist centre, include ultrasounds and MRI scanning to give evidence of disc displacement and Cone Beam CT to demonstrate joint degeneration. Medication, commonly a tricyclic antidepressant such as Nortriptyline, can be used at night to help with sleep, relaxation and improve pain in conjunction with conservative measures. SSRIs often exacerbate TMD pain and where patients present taking these, discussion with the GP with a view to changing the SSRI to an alternative antidepressant therapy can help treatment.
Burning Mouth Syndrome (BMS)
Background
This name encompasses a number of disorders, which include burning/pain (often of the tongue, lips and buccal mucosa) in the absence of soft tissue abnormalities, as well as a bad taste (dysgeusia), perceived dry mouth (xerostomia) with plenty of saliva present, or a feeling of paraesthesia. For this reason, the term oral dysaesthesia is often preferred. Glossodynia is another term for the same condition.
BMS is a diagnosis of exclusion and true BMS has no identifiable cause. It is a neuropathic pain in which there is either a disturbance in the way in which information is passed from the oropharynx to the brain, or the understanding of that information by the brain.
Aetiology
This is unknown. In some cases it behaves like a neuropathic pain and in others as an abnormal perception. In some patients, testing of vitamin B12, folate or iron reveals deficiencies; others have diabetes as an undiagnosed cause of dryness or neuropathy and in a few candida has been shown to be responsible for the burning. The most common finding in patients with BMS or other forms of dysaesthesia is a generalised tendency to anxiety.
Who is affected?
It is a condition which affects between 1-15 per cent of the population at some point and occurs more commonly in females particularly of peri-menopausal (as high as 40 per cent of this group), but these figures seem higher than seen in clinical practice in Scotland. Although any age can be affected, it occurs rarely in women below 30 years and men below 40 years.
Investigations
It is important to exclude lichen planus, haematinic deficiencies, diabetes and invasive candidiasis before concluding that there is an oral dysaesthesia. Gastro-oesophageal Reflux Disease (GORD) has been suggested as a trigger where taste is involved and a trial of a proton pump inhibitor is often given. Referral to the GP for exclusion of nutritional deficiencies and diabetes is sensible and, where oral dryness is the main complaint, a review of the patient’s medication to see if any medicines with antimuscarinic side effects can be eliminated.
Treatment
A lower soft acrylic bite splint can be helpful to avoid irritation from teeth if a parafuctional habit is present. This is particularly the case where the symptoms are predominantly present around the edge of the tongue. Chewing gum is a useful distraction from symptoms and Gelclair or similar products can be helpful to soothe and distract from the sensation. Alphalipoic acid has shown to be helpful to some patients- this can be purchased at health food shops.
Relaxation/stress reduction exercises and hypnotherapy can be useful where patients are not keen for medication but the use of a tricyclic antidepressant such as Nortriptyline for up to six months can give a good reduction in symptoms. Sometimes patients seek reassurance of the absence of pathology and have comfort in knowing their diagnosis and require no further treatment. Many have suspected that they have cancer and the dentist should always make clear to the patient that this is not the case.
Specialist referral
In many circumstances the patient can be managed in primary care by the dentist and the doctor, but where there is doubt as to the diagnosis or the patient’s symptoms fail to respond to the treatments outlined above, referral to an oral medicine specialist is needed.
Figure 2
| SOCRATES in BMS | |
|---|---|
| SITE | Anterior 2/3 tongue, anterior hard palate and lower lip most common sites |
| ONSET | Often spontaneous onset – patients often attribute to recent dental treatment, illness or medication persisting for months or years In many cases, symptoms will eventually resolve – patients are reassured by this |
| CHARACTER | Burning, scalding, tingling, metallic or foul taste Present each day, but can become intermittent as it resolves |
| ASSOCIATED FACTORS | Anxiety a very common finding Poorly fitting dentures ACE inhibitors may be linked to cause and cessation may resolve In men, adultery is an associated factor that has been seen due to guilt and associated stress |
| TIMING | Not present on waking Symptoms often become more severe as day progresses – most severe in evening Does not affect sleep |
| EXACERBATING/ RELIEVING FACTORS | Talking, eating spicy food, stressful events all make worse Relieved by eating, chewing gum and ‘being busy’ |
| SEVERITY | Varies: mild to severe |
Maxillary sinusitis
Background
Acute maxillary sinusitis produces unilateral midface pain which can be very similar in character to pulpal or periapical pain in the upper molar teeth. It should be suspected where a dental cause does not seem likely after clinical and radiographic examination of the teeth and sensibility testing. It can also be confused with TMD pain.
Who is affected?
Sinusitis rarely affects children below the age of nine years as the maxillary sinuses do not develop properly until puberty. Elderly people are at higher risk due to both a more compromised immune system and also a combination of anatomical and physiological factors such as dry nasal mucosa, weaker cartilage causing airflow changes and a diminished cough/weakened gag reflex.
Atopic individuals show a particular high risk for developing chronic sinusitis.
Aetiology
Most are viral infections. Chronic sinusitis is not painful, only acute exacerbations. There may be local nasal and sinus abnormalities contributing to the aetiology, such as polyps in the nose or sinus, septal deviation or obstruction to the meatus of the sinus in the nose. There may have been a precipitating event such as an upper molar extraction where the roots have been close to the sinus floor.
Character
Constant throbbing pain which may vary in intensity.
Associated features
There will often be a history of sinusitis and frequently an awareness of a bad taste or halitosis. This is often worse in the morning and due to pus running into the oropharynx from the nasal floor (post nasal drip). Many patients get tenderness to pressure of the cheek over the affected sinus and discomfort on pressure on the alveolar ridge between the roots of the first and second premolar teeth. The patient may report the pain as being more severe on bending forward or
lying down.
Management
If maxillary sinusitis is suspected, the patient should be referred to their GP for appropriate treatment. If the dentist wishes to give temporary supportive therapy, this can be with spray or drop nasal decongestants and not antibiotics, which are ineffective in viral infections.
Trigeminal neuralgia (TN)
Background
TN is usually a straightforward diagnosis due to the character of the pain experienced. The sudden intense and short duration of the pain means that the dental pains which can be confused with TN are acute dentine sensitivity and cracked cusp syndrome. Both of these can give similar histories in some patients where the trigger for trigeminal neuralgia is intraoral. The dentist should look carefully for evidence of these, trying agents to reduce sensitivity, testing the cusps of the premolar and molar teeth in the area of the pain.
Aetiology
The cause of TN is often unknown. Demyelination of the trigeminal nerve is a common factor, however, and this may be due to pressure from an adjacent blood vessel, or, less commonly, a tumour or other intracranial mass (2 per cent of patients) or multiple sclerosis. Diagnosis is by clinical assessment and exclusion of other causes of pain.
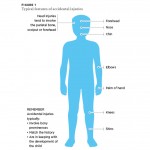
Who is affected?
Trigeminal neuralgia is a rare condition traditionally affecting an older age group, typically individuals over 50. However, many more patients now are seen in a younger age group and the diagnosis should be considered in any patient
with the characteristic pain history. More women are affected than men and the overall prevalence varies in the literature, but has been quoted at between 0.16 per cent and 0.3 per cent.
Character
The key feature of trigeminal neuralgia is the short intense pain experienced on one branch of the trigeminal nerve. This may be triggered by touch, washing, eating or a change in ambient temperature. The patient often describes the pain as being “like an electric shock” and stops them in their tracks.
However, between these, the patient is pain free, although some describe a burning feeling in the trigger area. Trigeminal neuralgia often first presents in the autumn and is frequently worse over the winter months.
Associated features
Rarely, patients will report swelling and redness in the area of their trigger.
Management
Trigeminal neuralgia requires specialist assessment and management at the beginning. Once the treatment is stabilised, the care can be continued in primary care. Primarily, this should be through the GP. A dentist suspecting TN should liaise with the patient’s GP for a referral to oral medicine or neurology and to start the patient on an appropriate medicine, usually carbamazepine whist the referral process progresses.
Although this drug is in the dental formulary, it should only be started by a dentist on the instruction of a specialist, particularly because the patient needs to have blood tests before and during treatment with this drug.
Conclusions
Although many of the pain conditions covered in this article would traditionally be referred to a specialist unit, a good history, careful examination and appropriate investigation can help establish an accurate diagnosis, which can facilitate initial management in a practice setting. This can be much more convenient for the patient and allow a much quicker start to treatment and relief of symptoms.
The simple strategies outlined above are frequently effective, making for a happy
patient and dentist. They are often the first things tried by a specialist and having this initiated in primary care means that patients subsequently passed to a specialist get quickly on to the more complex treatments where needed. Patients often have to travel significant distances for specialist care, especially in oral medicine and are often grateful for management locally. Additionally, limiting the pressures on tertiary care centres allows the patients needing this level of care to be seen more promptly.
Always try to have the same methodical process for pain history taking using SOCRATES – this will help form a logical thought process for forming a diagnosis. Employ all means of investigation prior to referral. Radiographs in particular are critical to eliminating dental sources of pain. Liaison between dentists and general medical practitioners is underutilised and is of immense benefit for complete patient care, from simple investigations to appropriate prescribing or onward referral to specialist medical services.
About the authors
Emma Finnegan graduated in Dentistry from the University of Glasgow and has a special interest in oral medicine. She currently working as a core trainee in Glasgow Dental Hospital and School.
Dr Alexander Crighton is a consultant in oral medicine and honorary senior lecturer in medicine in relation to dentistry at Glasgow Dental Hospital and School.
In children, the goal is to restore the tooth once for the lifetime of that tooth, yet full coverage restorations for primary teeth are underutilised in general practice.
The function of a crown is to protect existing tooth structure and to retain the tooth in function. Numerous clinical situations require full coverage restorations in primary molars in order to provide the most durable restoration (Table 1). Primary teeth with extensive caries can be restored most successfully with crowns. Enamel hypoplasia of the primary molars may require replacement of cusp anatomy which is also best achieved by full
coverage restoration.
Crowns also provide an optimal coronal seal for pulpally treated primary molars; research shows that indirect pulp therapy, pulpotomy and pulpectomy procedures have better outcomes as clinical success depends on protecting the tooth from the oral environment. Protection of the dentinal-pulpal complex from contamination of the oral environment also promotes healing and protects the vitality of reversibly inflamed pulp, eliminating the need for pulp therapy.
Crowns are also indicated for developmental defects of the tooth structure; teeth with extensive tooth surface loss due to attrition, abrasion, or erosion; fractured primary molars; and infra-occluded primary molars to maintain mesio-distal space (Seale and Randall 2015).
Classification of prefabricated crowns for primary molars
All prefabricated crowns for primary molars are available in varying sizes for each primary tooth type. The manufacturers seeks to replicate the height, mesio-distal width, contour and anatomy of the natural primary teeth, specifically to accommodate the convexity of the cervical margins and the exaggerated mesio-buccal bulge on primary first molars.
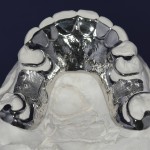
Stainless steel crowns (SSCs) or preformed metal crowns (PMCs) are widely recognised for their strength and longevity; however, due to the metallic colour, they lack aesthetics (Fig 1) (Seale and Randall 2015). Chair-side techniques for direct veneering and open-facing have been used to mask the metal colour. Over the years, alternative tooth coloured full coverage restorations have been tested using different types of dental materials and techniques with varied levels of success. Commercially fabricated preveneered SSCs combine durability and aesthetics (Leith and O’Connell, 2011; Kratunova and O’Connell, 2014; O’Connell et al. 2013). Prefabricated crowns made from composite resin, high density polymers, polycarbonate and zirconia offer a tooth coloured alternatives (Fig 2).
| INDICATIONS FOR FULL COVERAGE RESTORATIONS |
|---|
| Extensive tooth destruction – caries, erosion, developmental defects |
| Caries with > two surface involvement |
| Post pulp therapy |
| Fractured molars |
| Infra-occluding molars: to maintain mesio-distal space |
| Patients with high caries susceptibility/OH impairment /special needs |
| Caries lesions restored under general anaesthesia |
Conventional stainless steel crowns
Stainless steel crowns (SSCs) are prefabricated extra-coronal restorations which can be adapted to individual teeth and cemented in place to provide a definitive restoration (Kindelan et. al. 2008). The SSC is a durable, cost effective, minimally technique sensitive restorative option that offers the advantage of full coverage and accommodates the majority of treatment indications for primary posterior teeth (Seale and Randall 2015).
SSCs were popularised as a restorative method for primary molars in the 1950s (Humphrey 1950; Engel 1950). Over time, SSCs have been modified to improve the anatomical form and the alloy composition (9-12 per cent nickel; chromium 12-30 percent) (Randall 2002). The conventional SSCs are pre-trimmed, pre-contoured and crimped and usually need no or minimal adjustment by the operator. The conventional tooth preparation requires local anaesthesia and the tooth is prepared with 1-1.5mm occlusal reduction and minimal proximal reduction of the primary molar to allow for the crown thickness (0.2mm). The armamentarium required for placement of a SSC is outlined in Table 2.
| TABLE 2 | ||
|---|---|---|
| Armamentarium required for placement of conventional stainless steel |
||
| BURS | Occlusal reduction - Football Proximal reduction - Flame |  |
| SSC INSTRUMENTS | Crimping Pliers Gordon Contouring Pliers Johnsons contouring Pliers Howe Pliers Bee Bee Curved Crown scissors Band seater |  |
| SSC KITS | Available from the major manufacturers either retrimmed, crimped and contoured, or pretrimmed with paralled walls |  |
The finish line should be a smooth feather edge at or below the gingival margin with no step or shoulder. A snap fit is achieved when the flexible metal margin passes over the buccal bulbous area and fits into the cervical constriction of the molar. SSC margins can be well adapted into the undercut areas with the help of contouring and crimping pliers (Randall 2002). SSCs cannot be used in children with nickel sensitivity. Any self-curing luting cement can be used to secure these crowns, with glass ionomer being the most popular material.
Stainless steel crowns using Hall technique
There is growing evidence that a biological approach to management of caries is effective (Kidd 2004; Ricketts et al. 2006; Thompson et al. 2008) and the technique is now gaining popularity worldwide. Isolating the caries in the tooth using a crown (sealing in caries) isolates the microflora from their nutrients reducing/eliminating their ability to cause demineralisation. The dentinal-pulpal complex is also protected from the oral environment arresting the caries process, and maintaining of the vitality of reversibly inflamed pulp.
Placement of a SSC on carious primary molars without any prior tooth preparation, decay removal, or local anaesthesia is known as the ‘Hall Technique’, named after Dr Norna Hall who had used this novel method in her clinical practice since the 1980s. The indications for Hall crowns are the same as those of conventional SSCs but cannot be used where there is a diagnosis of irreversible pulpitis or dental sepsis (Innes et al. 2009, 2011).
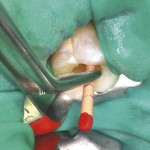
Success of the Hall technique relies on correct pulpal diagnosis. There is no need for local anaesthesia as there is no reduction of tooth structure and no caries is removed. The crown is filled with a glass ionomer cement and pushed onto the tooth thereby sealing the caries lesion from the oral environment. Sometimes, it is necessary to use orthodontic separators and a band seater to allow easier seating (Fig 3). Evidence of the clinical success of this technique after five years is very promising (Innes et al. 2011).
The crown is cemented onto an unprepared tooth causing a premature contact on that tooth. This increase in the vertical dimension of occlusion seems to be of little consequence in children, as occlusal equilibrium is re-established within two to four weeks, without any symptoms (Gallagher et al. 2014).
Preveneered stainless steel crowns
The increasing demand for a more natural appearance of primary tooth restorations led to the introduction of the commercially produced aesthetic preveneered stainless steel crowns (VSSCs) for paediatric dental patients. Recent developments in dental materials result in thermoplastic, composite or epoxy resin veneers to be bonded successfully to base metal using mechanical retention and/or chemical bonding (Hosoya et al. 2002).
The VSSCs were developed to combine the strength and durability of the conventional SSCs with the aesthetically pleasing appearance of the white veneer facing (Figure 4a, 4b). The exact specifications of the attachment, thickness and pattern of the veneer remains proprietary to the individual manufacturer. However, the makers of the current leading brands VSSCs (Nusmile, www.nusmilecrowns.com – and Kinderkrowns – www.kinderkrowns.com) have disclosed that the veneer is a composite resin material which is attached either through an intermediate bonding agent to the pre-prepared (e.g. alumina blasted) metal surface or is bonded and additionally mechanically retained to a fenestrated stainless steel core in different patterns (Fig 5).
The composite facing material requires adequate thickness for mechanical strength and ability to withstand occlusal masticatory forces. Therefore, the tooth preparation for a VSSC has to be modified to allow for this increased bulk in the occlusal and buccal surface. Greater buccal reduction is required. Local anaesthesia is required for tooth preparation with 1.5mm occlusal reduction.
Circumferential reduction is required to remove any cervical undercuts as the crown must fit passively onto the tooth. The finish line is 1mm below the gingival margin. This reduction of tooth structure is much greater than conventional SSC crown preparation but does not result in exposure of the pulp. Pulp therapy will be dictated by the extent of caries. VSSCs cannot be crimped in the areas of the facing so that limited crimping is advised only on the metal margins.
Manufacturers also warn that the metal substructure flexes from pressure during crimping, fitting or seating and this could introduce micro-fractures to the facing which subsequently can progress to veneer loss. Veneer wear or fracture may occur but the restoration will not need to be replaced as the tooth remains protected by the metal substructure (O’Connell and Kratunova 2014). Heat sterilisation may cause discolouration of the facing material and the manufacturers advise chemical sterilisation for colour stability.
- FIGURE 1 Restored primary molars showing the poor aesthetics of the stainless steel crowns in the smile.
- FIGURE 2 Prefabricated full coverage restorations currently available for primary molars in order: stainless steel crown, crown former for composite posterior strip crown, Nusmile veneered SSC, KinderKrown VSSC and a zirconia crown.
- FIGURE 3 Provision of a full coverage restoration using the Hall technique. No local anaesthesia or tooth preparation. A. placement of orthodontic separators B. space provided after 1 week C. Cementation of SSC
- FIGURE 3
- FIGURE 3
- FIGURE 4 Life-like aesthetics of pre-veneered SSC (VSSC) placed on the lower first primary molars A. the smile line and B. intraorally
- FIGURE 4
- FIGURE 5 A. The internal surface and B. external surface demonstrating differences between the various commercial brands of VSSC
- FIGURE 5
- FIGURE 6 Primary molar zirconia crowns A. Excellent aesthetics in the smile B. Intra-oral view of same child
- FIGURE 6
- FIGURE 7 Variations in the size, contour and anatomy of the various manufacturers of prefabricated zirconia crowns currently available requiring modifications in tooth preparation.
Prefabricated paediatric zirconia crowns
Zirconia has become increasingly popular as a restorative material due to its exceptional properties combining high aesthetic value and excellent mechanical characteristics (Zarone et al. 2010). Prefabricated paediatric zirconia crowns were first manufactured for clinical use in 2007. The solid zirconia construction offers high strength and durability along with superior aesthetics due to realistic anatomy and shade of the crowns (Fig 6a, 6b). It has been demonstrated that zirconia does not enhance bacterial adhesion and growth (Scarano et al. 2004) so that the surface biocompatibility and thin gingival margins of the crowns do not compromise gingival health. The colour of zirconia crowns is stable and fracture of the ceramic is unlikely given the high flexural strength and fracture toughness of the material. These crowns can be used in nickel-sensitive patients.
Zirconia is rigid and must fit passively on the tooth, therefore clinical skill is required to allow for appropriate (but not excessive) tooth preparation. The tooth preparation is critical as no crimping is possible in the zirconia crowns and adjustment of zirconia is not advised. In addition, each manufacturer of zirconia crowns emphasises different anatomical features that will necessitate alteration of the tooth preparation for maximum success (Fig 7).
Local anaesthesia is required for the tooth preparation with occlusal reduction of 1.5 – 2mm. Circumferentially, the primary tooth is reduced uniformly 1.5mm with a subgingival margin extension of 1-2mm. The zirconia crown should have a passive fit without any friction on tooth structure and no bulging of the gingival tissue. Paediatric zirconia crown kits are now commercially available in the EU and are very attractive for patients/parents and clinicians.
There are no published prospective clinical trials published so far reporting on the performance of zirconia posterior crowns, but data on anterior primary teeth shows that they perform well over time.
The general dental practitioner should use full coverage restorations routinely, especially for children with cavitated proximal lesions and in children assessed as high risk for caries. There have been significant advances in restorative paediatric dentistry and the newer options exist to provide aesthetic restorations for children.
The use of Class 2 restorations using composite, compomer, or glass ionomer should be restricted to small proximal lesions in children at low caries risk, or as a temporary solution. Selection of the most appropriate restoration must be based on the individual case and additional training will be required for clinicians to become competent in these techniques.
All these options however are valuable as part of the clinicians’ armamentarium providing restorative choice in the contemporary paediatric dental practice.
About the authors
Anne C. O’Connell, BA, BDentSc, MS, FIDT
Evelina Kratunova, BDentSc, MFD(RCSI), DCh Dent, FFD(RCSI)
References
Engel RJ. Chrome steel as used in children’s dentistry. Chron Omaha Dist Dent Soc. 1950; 13:255-258. Epidemiol. 1998; 26(1 Suppl): 8-27.
Gallagher S, O’Connell BC, O’Connell AC. Assessment of occlusion after placement of stainless steel crowns in children – a pilot study. J Oral Rehabil. 2014 Oct;41(10):730-6. 10.
Guess PC, Att W, Strub JR. Zirconia in Fixed Implant Prosthodontics. Clin Implant Dent Relat Res. 2010 Dec 22.
Hickel R, Kaaden C, Paschos E, Buerkle V, García-Godoy F, Manhart J. Longevity of occlusally-stressed restorations in posterior primary teeth. Am J Dent. 2005 Jun; 18(3): 198-211.
Hosoya Y, Omachi K, Staninec M. Colorimetric values of esthetic stainless steel crowns. Quintessence Int. 2002 Jul-Aug; 33(7): 537-41.
Humphrey WP. Use of chrome steel in children’s dentistry. Dental Survey. 1950; 26: 945-949.
Innes N, Evans D, Hall N. The Hall Technique for managing carious primary molars. Dent Update. 2009 Oct; 36(8): 472-4, 477-8.
Innes NP, Evans DJ, Stirrups DR. Sealing caries in primary molars: randomized control trial, 5-year results. J Dent Res. 2011 Dec;90(12):1405-10.
Kidd EA. How ‘clean’ must a cavity be before restoration? Caries Res. 2004 May-Jun; 38(3): 305-13.
Kindelan SA, Day P, Nichol R, Willmott N, Fayle SA; British Society of Paediatric Dentistry. UK National Clinical Guidelines in Paediatric Dentistry stainless steel preformed crowns for primary molars. Int J Paediatr Dent. 2008 Nov; 18 Suppl 1: 20-8.
Kratunova E, O’Connell AC. A randomized clinical trial investigating the performance of two commercially available posterior pediatric preveneered stainless steel crowns: a continuation study. Pediatr Dent. 2014; 36(7):494-8.
Leith R, O’Connell AC. A clinical study evaluating success of 2 commercially available preveneered primary molar stainless steel crowns. Pediatr Dent 2011; 33:300-6.
O’Connell AC, Kratunova E, Leith R.Posterior preveneered stainless steel crowns: clinical performance after three years. Pediatr Dent. 2014 May-Jun;36(3):254-8
Ricketts DN, Kidd EA, Innes N, Clarkson J. Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database Syst Rev. 2006 Jul 19; (3): CD003808.
Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and anatase-coatedtitanium healing screws: an invivo human study. J Periodontol. 2010 Oct; 81(10): 1466-71.
Seale NS, Randall R The use of stainless steel crowns: a systematic literature review. Pediatr Dent. 2015 Mar-Apr;37(2):145-60
Thompson V, Craig RG, Curro FA, Green WS, Ship JA. Treatment of deep carious lesions by complete excavation or partial removal: a critical review. J Am Dent Assoc. 2008 Jun; 139(6): 705-12.
Like most topics, decontamination has gone through phases of being high profile and then seemingly disappears off the radar. Recently, when decontamination does re-emerge, it is often when errors or omissions have been identified. It is still undoubtedly an extremely emotive issue, particularly when things go wrong. It is also a critical element as far as patient safety is concerned.
Dental practices and their teams have come a long way in the last five years as far as decontamination is concerned. We have been in a period of consolidation as far as guidance and requirements are concerned but, in my experience, we occasionally slip back into old habits. Reviewing and refreshing our knowledge and skills is essential to ensure we are following the requirements and able to show we are doing the right things to the best of our ability.

Figure 1
The decontamination cycle (Fig 1)
Decontamination is the process by which reusable items are rendered safe for further use on patients and safe for staff to handle. The process is complex and involves several stages, with potential for error throughout.
The decontamination cycle begins in the surgery with segregation of reusable items and disposal of single-use items and other materials in appropriate waste containers. Items to be processed for reuse must be transported safely to the Local
Decontamination Unit (LDU) as soon as possible. The transport boxes should be rigid, lidded, and easy to clean. These transport boxes must be easily identifiable as containing either ‘dirty’ or ‘clean’ items to avoid any potential confusion. Colour coded boxes are often the simplest way to ensure this. Using marker pens or labelling only the lids still leaves potential for error.
The next stages of the cycle are cleaning, inspection, sterilisation packing and storage.
Local Decontamination Units (LDU)
Dental practices today – space, the first frontier
Today, those considering setting up new dental practices need to make sure they have enough space to meet current requirements and ensure they are future proofing their setting. Recently, the number of dental professionals looking to set up new practices has been increasing. The settings of choice tend to be small commercial units in shopping areas where there is potential for patient footfall. I do have some concerns that, in the drive for financial viability, they are starting out with a limited area and will find they run out of space in a short time.
Despite advances in new technology, implying that practices should become more streamlined, the reality is we have many more items to house. In my experience, our need for storage capacity has not decreased despite the drive towards paperless systems and digital advances. Lack of space can result in cluttered, chaotic and disorganised settings with less potential to create a good impression and more potential for error, particularly in relation to good infection control and decontamination.
LDU compliance
Current guidance states an LDU compliant with SHPN13 is essential for primary care dental practices (Compliant Dental Local Decontamination Units in Scotland (Primary Care) (2013)).
Key points
General requirements for LDUs:
- Away from the clinical area and no activity other than decontamination undertaken
- Dirty and clean areas clearly demarcated
- Instrument flow from dirty to clean
- Smooth cleanable surfaces
- Well lit with ventilation
- Enough space for equipment and set-down areas.
Essential components
- Hand wash sink and Personal Protective Equipment (PPE)
- Set-down areas
- Washing sink and rinsing sink
- Washer disinfector
- Inspection areas
- Sterilisers
- Packing area.
Every dental practice in Scotland now has a room dedicated to the decontamination of dental instruments. Having an LDU is the accepted norm and is an essential requirement for the Combined Practice Inspection. These LDUs can undoubtedly vary in shape and size, but the general lay out should be in line with the single room model as stipulated in Scottish Health Planning Note 13 (SHPN13). There are sometimes some minor variations in the configuration and they may not all follow the exact requirements of SHPN13.
The design differences often relate to limited space available or build decisions determined by a contractor. Limitations such as plumbing, or other seemingly insurmountable building difficulties, have often been identified as the cause. In some cases, health boards may have agreed to minor deviations from the guidance to ensure continuance of a service when there appeared to be no other option available.
Some LDUs are undoubtedly smaller than the preferred option and space constraints are not ideal. In these circumstances, it is essential that the correct process is applied to the letter every time to avoid errors. These errors are often due to insufficient set-down space. All staff must be trained accordingly to ensure everyone knows and follows the exact procedures in place for that setting.
Other difficulties relate to using the dedicated LDU for other purposes. Again, this usually comes about due to overall space limitations in the practice. These other activities have ranged from housing X-ray developers to tea and even food preparation, neither of which is acceptable either for staff or patients. Hopefully, that message has been heard loud and clear and common sense now dictates that this is not acceptable.
LDUs are now in use across Scotland. Staff have accommodated remarkably well. I don’t believe many would wish to go back to carrying out decontamination in the clinical area. The constant background activity of washing up, while an ultrasonic rattled incessantly and autoclaves generated sauna-like conditions, was not exactly conducive to the provision of good quality patient care.
- FIGURE 2A SHPN 13 part 2 Dedicated separate Room/rooms
- FIGURE 2B Washer disinfector in LDU
- FIGURE 3 single-use symbol
- FIGURE 4 clip trays
- Tray of instruments loaded correctly for optimal processing in a non-vacuum steriliser
- Print-out showing the parameters reached during the sterilisation cycle
Single-use items
The guidance stipulates that the use of single-use items should be the option of choice where possible as long they are viable and work effectively for the purpose required. All items carrying the single-use symbol (Fig 3) should not be re-used or reprocessed. If this symbol appears on an item this is part of the manufacturer’s instructions. Compliance with manufacturer’s instructions is accepted as the legal requirement for all equipment.
Specific single-use items that have presented difficulties include:
- Three-in-one tips. Reusable metal tips are unacceptable as they are extremely difficult to clean and there are good disposable alternatives. The requirement for single use three-in-one tips is part of the practice inspection.
- Endodontic files. This has been a requirement in Scotland since 2004 and has not changed. (The situation in England is different in that they allow for re-use on the same patient. The issue with this is the exacting requirement for reprocessing and the potential for error as far as identification and storage are concerned.)
- Plastic impression trays are single-use despite the fact labs return them to practices for disposal. The effort required to clean and re-use most certainly outstrips any benefit gained considering the time and energy expended on trying to clean and prepare these for re-use.
- Matrix bands. There is evidence to show that these items, which are often heavily
contaminated with blood, cannot be cleaned effectively and present a risk to staff and patients. These must be dismantled with care and disposed of in appropriate waste containers for sharps. The holder must then be cleaned and sterilised. There are single-use alternatives.
The decontamination process
The decontamination process is about the application of knowledge and skills and is dependent on what individuals do in their own settings. The decontamination process in the LDU includes cleaning, inspection, sterilisation and packing for storage.
The general principles of the process are:
- All items should be processed according to manufacturer’s instructions. The problem with this can be that the instruction provided may not be clear or explicit. In that case, you are entitled to request information from the manufacturer or via the supplier.
- The flow of the instruments in the decontamination process is always from the dirty to clean area and never goes back in the process. The only exception would be if visible soil is picked up through inspection and the item is returned to the start of the cycle to repeat the full process.
- Using an automated cleaning process is required and washer disinfectors are essential for cleaning dental instruments.
- All re-usable items must be at least sterilised if not sterile at the point of use.
- Policies and procedures must be in place for all aspects of decontamination. All staff must have read these and can access them for easy reference.
Cleaning
Washer disinfectors – the final hurdle for compliance?
“Use of a washer disinfector (WD) is a requirement for compliant reprocessing of dental instruments” (Compliant Dental Local Decontamination Units in Scotland (Primary Care) (2013)). Using a washer disinfector is the preferred method for cleaning dental instruments because it offers the best option for the control and reproducibility of cleaning. This means the cleaning process can be validated. WDs are used to carry out the processes of cleaning and disinfection consecutively.
A typical WD cycle for instruments includes the following five stages:
- Flush – Removes gross contamination. Latest standards indicate that a water temperature of <45°C is used to prevent protein coagulation and fixing of soil
to the instrument - Wash – Removes any remaining soil. Detergents used in this process must be specified by the manufacturer as suitable for use in a WD
- Rinse – Removes detergent used during the cleaning process.
- Thermal disinfection – The temperature of the load is raised and held at the pre-set disinfection temperature for the required disinfection holding time: for example, 80˚C for 10 minutes, or 90˚C for one minute
- Drying – heated air removes residual moisture. Some manufacturers have worked on this in an effort to reduce cycle times as this was a significant barrier to their use. They have endeavoured to reduce the cycle times to improve efficiency for use in practice and while still demonstrating effective cleaning efficacy as per testing requirements.
What have the problems been?
It is safe to say that the dental profession in Scotland has been slow to adopt this piece of equipment as a ‘must have’ as they strive towards best practice in decontamination.
The reasons for this are varied and complex. The reputation of these items have been somewhat tarnished often through anecdote and bad press. Admittedly, this was not helped by some genuine technical problems related to specific machines resulting in some practitioners experiencing difficulties despite their best efforts. Negotiations with suppliers and manufacturers have been ongoing in an effort to resolve specific cases. From the outset, some practitioners heard about these problems and simply decided not to try for themselves.
Another difficulty with washer disinfectors was that they didn’t fit naturally and seamlessly into our existing processes. We had to change aspects of what we did to make them work efficiently and effectively for us. Change is difficult and it takes time. The early abandoners ran out of patience and gave up quite quickly. Some of the more tenacious teams persevered and have become converts. Recently, I have had some surprisingly positive feedback from some of the more strident early objectors.
The fact is, these machines are an essential requirement in Scotland to ensure our reusable instruments are clean and able to be sterilised effectively.
To utilise a washer disinfector efficiently and effectively, in my opinion, we need several things. First of all, you need have done a capacity calculation to work out which washer disinfector suits the needs of your practice. The overarching aim is ultimately to run the washer disinfector a minimum number of times a day and only put it on when it’s at or close to its full capacity. To work that out, you need to look at:
- How many items are used in the practice in an average session?
- What does the WD hold?
- Could the internal set-up be improved to hold more?
- How long will it usually take to get the WD to capacity?
- How long does the full decontamination cycle take?
- Do you have enough stock of instruments to avoid shortages at busy times?
In my opinion, using clip trays (Fig 4) for cons kits are essential to allow the WD to work efficiently for you. The initial capital outlay will save running cost in the longer term. It also reduces risks for staff having to spend time dismantling open trays, which need to cleaned separately and then reassembled before storage.
Members of the dental team who work in the LDU are best placed to work this out and establish a routine that suits the way the practice works and use the WD efficiently and effectively.
Ultrasonic cleaners
Compliant ultrasonic cleaners are also an automated cleaning method. They are useful as a back-up cleaning method. They are no longer an essential requirement as far as the practice inspection is concerned as washer disinfectors are the first line cleaning method and an essential requirement.
Ultrasonic cleaners can be utilised to pre-clean particularly heavily soiled instruments before processing in the washer disinfector. This is useful if there is a delay before the washer disinfector is at capacity and heavily contaminated surgical kits would become difficult to clean if left to dry out. Pre-cleaning is advisable in that situation.
Using an ultrasonic cleaner if the washer disinfector is down for short periods is acceptable. The ultrasonic cleaner will have to be validated and tested as per manufacturers’ instructions to ensure it is functioning effectively if it has to be brought back into use. In a busy practice, an ultrasonic alone may not provide the capacity required to ensure throughput and it may be necessary to revert to full manual cleaning as well.
Reverting to full manual cleaning utilises significant volumes of hot water,
detergent and staff time. It also puts your staff at risk of injury. Using manual cleaning should only be adopted as a last resort for cleaning dental instruments. When service and maintenance contracts for washer disinfectors are being arranged some assurance from the supplier as to their response time and contingency plans, if the washer disinfector fails, should be sought. Details of full manual cleaning process can be found in The SCDCEP guidance document – Cleaning Dental Instruments, can be accessed at www.sdcep.org.uk/published-guidance/decontamination/
Handpieces and washer disinfectors
Cleaning handpieces effectively due to the extremely narrow lumens is a difficulty. As far as I am aware, there has been little progress on effective handpiece cleaning in washer disinfectors. Some practices are processing handpieces in their washer disinfectors without detriment to their equipment. Most practices are understandably tentative about putting these delicate, expensive items in their washer disinfector. There is no specific guidance that stipulates this is a requirement. If you plan to process handpieces in a washer disinfector, make sure you have written instructions and an assurance of compatibility from both the handpiece and the washer disinfector manufacturer.
Decontamination process – sterilisation
All reusable items must be sterilised. From time to time we come across situations where there is some confusion as to what type of autoclave is in use or which cycle is being used. It is imperative that the whole dental team understands the difference between vacuum and non-vacuum cycles in benchtop sterilisers to ensure these are used safely and effectively.
- A non-vacuum cycle can only be used for unwrapped items. When the cycle is complete, the items will have been sterilised.
- It is essential that any steam steriliser is not overloaded.
- If a vacuum cycle is used, items can be wrapped or bagged before sterilisation. When this cycle is complete, the items will be sterile as long as the packaging is intact.
Please note, if items are wrapped before being placed in a non-vacuum cycle. they will not have been sterilised. If these items were subsequently used. this presents a significant risk to patient safety. This is a serious event and must be reported.
Maintenance, testing and validation of all decontamination equipment
There tends to be some confusion as to what is required as far as testing and validation of equipment is concerned and what your engineer, supplier or manufacturer provides as part of contractual arrangements.
Maintenance contracts for your decontamination equipment are required to make sure the equipment is in good mechanical working order. You may have options as far as the cover you choose. Make sure you are certain which cover you are paying for and exactly what it includes. Testing and validation are not the same as general maintenance. Your engineer may do this at the same visit as part of the contract. Always make sure you know exactly what they have carried out and retain all paperwork as evidence.
Validation is a documented procedure used to show that the decontamination process will repeatedly and consistently take place to a satisfactory standard when defined operating conditions are used. Validation checks and tests are carried out at least annually, which is referred to as revalidation. Some manufacturers may refer to this as annual testing rather than revalidation.
Periodic testing is required to ensure that WDs perform consistently as specified at validation.
Tests and testing intervals will be stipulated in manufacturer’s instructions. Some of these tests will be carried out by practice personnel and provide regular checks to evidence that equipment is operating as per the parameters determined at validation.
A test person (engineer) will carry out periodic testing/revalidation as specified in the manufacturer’s instructions. This will be required at least annually. Always check with your engineer and make sure you know what is being carried out at each visit.
Testing carried out by practice teams include:
- Automatic control tests. These are required for washer disinfectors, ultrasonic baths and autoclaves. Details on how to perform automatic control tests can be found in the SDCEP decontamination guidance: www.sdcep.org.uk/published-guidance/decontamination/
- Cleaning efficacy tests are used to demonstrate the ability of washer disinfectors and ultrasonic baths to remove soil and contamination. Consult your manufacturer to see which tests are recommended and how often these should be done.
Storage
As far as storage of dental instruments after sterilisation is concerned, the general principle for all reusable items is to ensure that the potential for re-contamination through direct contact or aerosol production is eliminated.
Aerosol production during clinical procedures presents a risk of contamination of surfaces and items within the area. Aerosols contain blood, saliva and significant levels of associated micro-organisms. This can constitute a risk of transmission of infection as many of these micro-organisms can survive on surfaces for variable periods of time. Thorough environmental cleaning and closed storage must be applied to avoid potential risk of transmission of infection.
The practice of bulk storage of items for intraoral use should be discontinued. Using drawer inserts to store loose mirrors and probes is not acceptable as far as avoiding possible contamination is concerned. Storage options include the bagging of examination and other kits. Bagging of forceps and other items for oral surgery has been accepted as the norm for some time. Conservation kits in clip trays should be stored covered with a lid or bagged and can be placed in cupboards in racks or drawers either in the clinical area or in a central storage area.
All items for clinical procedures should be set out for use on each patient immediately before the treatment episode. During clinical procedure, when extra items stored in drawers or cupboards are required, good local systems for retrieval to avoid potential contamination of other items must be in place. This may involve glove removal and use of clean tweezers to ensure efficient safe practice.
Practices may have adopted different ways of fulfilling the requirements for storage related to their specific storage spaces and practice layout. Avoiding the potential for recontamination is essential and should be considered fully to ensure there are safeguards to ensure the risk of this is eliminated as far as possible.
In general:
- No unnecessary items intended for clinical use should be set out on work surfaces during clinical procedures. Reduced clutter means easier cleaning.
- Items set out for a specific patient treatment and not used must be fully reprocessed or disposed of if single use.
- Sterilised items even in closed storage such as cupboards or drawers should be covered.
There is no specific guidance in Scotland as far as the timescale for safe storage of non-sterile or sterile items. HTM 0105, the guidance applied in other areas of the UK apart from Scotland, stipulates more exacting requirements for storage (click here to see PDF)
Training
The need for suitable training enabling the application of good infection control and decontamination, in line with Scottish guidance, is essential for the whole dental team. Another essential requirement is quality assurance. Audit is the accepted method of choice. This is essential, not only for infection control purposes, but also to fulfil NHS terms of service.
NHS Education for Scotland can provide both and help to avoid the pitfalls.
Our national infection control support team is made up of dental nurses with extensive experience both in practice and as trainers. They have been trained specifically to Scottish infection control and decontamination guidance requirements. They have a wealth of knowledge and are fully aware of the differences in guidance in others parts of the UK. Our team can tailor sessions to meet any needs the practice feel they have. For example. if you are struggling to integrate your washer disinfector into your usual process. our team can help.
The training does provide knowledge, but the real focus is on practical application. In a busy practice, knowing what to do doesn’t mean we all do it every time. Our sessions are designed to identify what makes the application of that knowledge challenging and what might help to make that change. Providing the practice with an action plan is an essential element to enable these changes. This plan will be supported and followed up. We also have two short e-learning programmes that are useful for updates or induction for new staff. These can be accessed though the NHS Education Portal (https://portal.scot.nhs.uk/)
On request, in conjunction with booking a training session, dentists can access four pre-populated audits via the NES Portal covering four areas of infection control and decontamination. Our team can review data collection and provide feedback on audit reports. After submission of a satisfactory report, dentists will have evidence of quality assurance in their practice and be eligible for audit hours and allowance.
NHS Education for Scotland has worked hard over the last years to ensure a consistent message based on Scottish guidance requirements has been delivered to the whole dental team in every practice in Scotland. NES has delivered 2,313 in practice training sessions to 6,511 dentists and 1,335 DCPs.
The message is out there. If you feel your team could benefit from our training, please contact Natalya.Zhernakova@nes.scot.nhs.uk or call 0141 352 2642.
About the author
Irene Black graduated from Glasgow University in 1980, gained her Membership of the Faculty of General Dental Practitioners in 1999 and the Certificate in Effective Dental Management in 2005.
Along with her husband, she owned an NHS dental practice in Eaglesham for 27 years where she continues to work on a part-time basis.
Irene has been a dental practice adviser in Greater Glasgow and Clyde health board for 14 years and her interest in education developed during nine years spent as a vocational trainer.
She has worked as an assistant director for NHS Education with the remit for infection control and decontamination for the last eight years. This has included developing both in-practice and other training packages for the dental team. As part of this role, she has worked with Scottish Government and other NHS organisations in an effort to determine how the difficulties related to decontamination in dental services might be resolved.
Irene also works with the Scottish Dental Clinical Effectiveness Programme in guidance development and research.
References
Scottish Health Planning Note 13 Part 2, Local Decontamination Units (www.hfs.scot.nhs.uk/online-services/publications/decontamination/)
Local Decontamination Units: Guidance on the Requirements for Equipment, Facilities and Management (www.documents.hps.scot.nhs.uk/hai/decontamination/publications/ldu-001-02-v1-2.pdf)
Compliant Dental Local Decontamination Units in Scotland (Primary Care) (2013) (http://www.hfs.scot.nhs.uk/publications-1/decontamination/)
Modern dentistry has undergone a revolution in the area of cosmetic or aesthetic dentistry. Patients more frequently put an emphasis on improving the appearance of their teeth and often have high expectations. This article aims to demonstrate some factors that need to be considered and techniques used in order to achieve this goal. Clinical cases will be used to illustrate this process.
Patient history
Patients who wish to improve the appearance of the front teeth generally do so as there is a particular feature of their smile with which they are unhappy. Discolourations, previous dentistry, missing teeth, misshapen teeth, excessive gingival display, gingival recession, tooth crowding, spacing or movement are some examples of the dental factors affecting the smile (Figs ı and 2).
Depending on the individual patient’s presentation, different treatment options may be indicated to achieve their goals. The most important factor for success is accurately distilling from the patient what particularly concerns them about their teeth. Once this has been established, the clinician can then begin to visualise how the case will look upon completion. It goes without saying that it is particularly important to undertake a thorough extra-oral examination (Table ı). The clinician should be looking for any indications of factors that are detrimental to the appearance of the teeth.
During the intraoral examination, attention should be given to the occlusion, both static and dynamic, as this may influence the treatment plan, restoration type, number of teeth to be restored and even the materials to be used. Of importance also is the presence of tooth wear. Its location, distribution and characteristics will point to the underlying aetiologyı and correct management. A diagnosis of bruxism or parafunction may impact on the treatment plan.
Dento-gingival complex and importance of pink aesthetics
An understanding of the normal size, shape, position and arrangement of the natural dentition is essential. Much has been written about certain values or proportions that are key to a “perfect smile” but in reality, there is no single formula for all.
In practical terms, average anterior tooth size2, height:width ratios2 and relative proportion of anterior teeth3 are of use. This information can be taken together with a desired incisal edge position of the final restorations to arrive at a tentative starting point. When restoring anterior teeth, the most important starting point is the proposed final incisal edge position as this then determines tooth size and length. This may have important consequences on the gingival margin positions in order to maintain ‘ideal’ tooth proportions for an aesthetic outcome (Figs 3 and 4).
An example of this would be where tooth wear has occurred and the worn teeth may have experienced compensatory over-eruption maintaining the position of their incisal edges. In this instance, further addition to the incisal aspect of the teeth would not result in an aesthetic outcome and consideration must be given to either orthodontic repositioning of the teeth prior to restoration, or possibly crown lengthening to reposition their gingival margin levels.
The relationship of the periodontal tissues – in particular, the gingival margin positions, symmetry, interdental papilla and amount of gingival display – are all important (Fig 5). Much has been written on the need for aesthetically correct gingivae to frame the teeth or restorations to provide highly aesthetic outcomes. Periodontal plastic procedures can aid the outcome of restorative dentistry, so co-ordination with periodontal colleagues is vitally important. An understanding of the limitations of grafting procedures is also important and the use of alternatives, in particular the use of pink porcelain, should be considered (Fig 6). Careful communication with your laboratory is needed in order to develop natural-looking prosthetic gingivae.
- Patient A intra-oral. Discoloured, leaking restorations. Teeth are too broad and have poor axial alignment
- Patient A smiling. Poor smile aesthetics, occlusal plane disruption and poor tooth form
- Patient A – provisional restorations with corrected incisal edge position
- Patient A – in order to develop correct tooth size (Height:Width ratios) minor crown lengthening was undertaken
- Patient B – combined vertical and horizontal ridge defect with loss of gingival architecture
- Patient B – use of pink porcelain to create an artificial interdental papilla and achieve more ideal pink-aesthetics
Excessive gingival display (gummy smile)
Most often as restorative dentists we are challenged by a deficiency in periodontal tissues either as a consequence of periodontal disease or tooth loss. However, an excess of gingival tissue display can also be unsightly and can lead to a patient being unhappy with their gummy smile (Table 2).
In certain instances, subtractive periodontal procedures alone can be sufficient in the management of such cases. Where roots of teeth may become exposed by surgical crown lengthening procedures, root coverage may become necessary and should be planned for.
Depending on the aetiology and the contributing factors, dentistry alone may not provide the solution. Orthodontic treatment in isolation or together with maxillofacial or plastic surgery may be necessary to achieve the ideal aesthetic outcome, therefore a careful assessment should be made for such patients prior to treatment.
- Patient A – smooth tooth preparations and well-fitting provisional restorations allow for maintenance of periodontal health and ease of impressions
- Patient A – final restorations with improved proportions, alignment and characterised porcelain
- Patient A – overall improvement in smile from restoring six anterior teeth
- Patient C – bright natural teeth with minor surface loss
- Patient C – conservative preparations and restoration with feldspathic veneers to improve appearance
- Dark crown preps with discoloured cores
- Opaque zirconia based restorations to mask underlying discolouration
Treatment planning: diagnostic wax-up or virtual smile design
Before making any reversible alterations to the existing teeth, it may be necessary to undertake a diagnostic wax-up. This is of particular importance if changes are planned in relation to tooth size, shape or position. This can aid in patient acceptance, but more importantly gives a clear indication of the proposed final appearance of the teeth.
More recently, digital manipulation of clinical photographs using dedicated software has become available and this can be very useful to contrast pre-op images and planned results. Ideally, some form of temporary mock-up should be provided to see the effects of proposed changes in the patient’s mouth. This is not always feasible, as in some instances subtractive changes are being planned and this is where virtual smile design has an advantage.
Provisionalisation and tissue management
Once a treatment plan has been accepted and teeth have been prepared, careful provisionalisation following the blueprint of a diagnostic wax-up may be required. A period of time spent in provisional crowns can be useful for a number of reasons. This gives the clinician an opportunity to review questionable teeth, assess planned occlusal changes and finally review with the patient any alterations and their effects on the final aesthetic arrangement of the teeth. Should further changes be requested, provisional crowns can easily be adjusted and once acceptable can then be copied to create a go-by cast to be followed in final restorations.
In order to achieve acceptable aesthetic results with anterior crowns, subgingival crown margin placement is generally required. The maintenance of periodontal health is essential in order to allow for accurate impressions of the prepared teeth. Highly accurate impressions of stable gingival tissues allow for crowns to be made precisely resulting in better marginal fit and ongoing periodontal health. This is essential for predictable long-term aesthetic success (Fig 7).
Tooth colour: selection of appropriate materials
Patients generally do not complain that their teeth are too light and trends towards brighter teeth are seen in everyday practice. When restoring anterior teeth, the colouration of the prepared teeth should be carefully considered.
How light will interact with the final restorations is important here. Currently available indirect restoratives can be grouped according to their degree of translucency or opacity. Indeed, some currently available systems offer a range of translucency depending on the prevailing clinical conditions (Table 3).
In achieving the most aesthetic outcome, a balance must be struck between the nature of the prepared teeth, selection of the appropriate restorative materials and the degree of tooth preparation undertaken. The ideal situation would consist of a naturally coloured tooth allowing for a translucent restoration with minimal tooth preparation (Figs ı0 and ıı).
The other end of the spectrum, however, is also frequently encountered. Teeth that are highly discoloured will require more opaque restorations to mask their underlying darkness and the ceramist will need additional thickness of porcelain to create lifelike restorations. Unfortunately, there is no perfect system for all eventualities.
In the author’s opinion, there is still a place today for porcelain fused to metal crowns on anterior teeth in aesthetic dentistry in selected cases. Excellent results can be achieved when the ceramist is given enough room in terms of tooth preparation for creating natural-looking porcelain.
In order for our technicians to achieve the results we desire, as much information as possible should be made available to them. The final desired shade often is not enough and the shade of the prepared tooth stump should also be indicated. Photographs of prepared teeth are beneficial in this respect (Figs 12 and 13).
Customising the smile
When considering “ideal” aesthetics using “normal” measurements and relationships there can be a tendency towards arriving at an artificial or a “too-perfect” result. Many discerning patients want their teeth to be improved upon, but also request that the end result appears natural.
Nature inevitably demonstrates some asymmetries
and this usually adds character to an individual’s smile. Minor tooth rotations and attention to detail in terms of surface texture and shading can go a long way to achieving this goal.
Incorporating characteristics from the patient’s own natural teeth into the final restorations can also be a useful tool. Photographs of unprepared healthy adjacent or opposing teeth offers the ceramist an idea of shade transitions, enamel surface texture, tooth form and translucency and adds to the overall micro-aesthetics of the case (Figs 8 and 9).
Tables
| Table 1: Extra-oral examination | |
|---|---|
| FACIAL VIEW: | |
| Occlusal plane orientation | Tooth display (incisal edge position) |
| OVD assessment | Gingival display |
| facial symmetry/centre lines/alignment of teeth | |
| SAGITTAL PROFILE: | |
| Skeletal pattern. | OVD assessment |
| Labial-lingual position of incisor teeth | |
| SMILING VIEW: | |
| Smile line-normal, flat, reversed | Tooth display |
| Gingival display | buccal corridor |
| Tooth colour | Any other obvious deviations from ideal |
| Table 2: Factors associated with excess gingival display | |
|---|---|
| Tooth position | Large maxilla (vertical maxillary excess) |
| Delayed passive eruption | Gingival overgrowth |
| Short upper lip | Hyper-mobile upper lip |
| Table 3: Translucency of commonly used indirect restorative materials |
||
|---|---|---|
| TRANSLUCENT MATERIALS | VARIABLE TRANSLUCENCY | OPAQUE MATERIALS |
| Feldspathic Porcelain | E-Max | Zirconia based |
| Empress Esthetic | Procera Alumina | Metal-ceramic |
About the author
Dr Tom Canning, DentSc MFD (RCSI) DChDent (Prosthodontics), is a specialist prosthodontist and maintains a specialist prosthodontic practice at Clontarf Aesthetic Dentistry, 9 Clontarf Road, Dublin 3. Contact the practice at 00353 (0) 1 525 0490 or by visiting www.clontarfaestheticdentistry.com
References:
- Verrett RG (2001): Analysing the aetiology of an extremely worn dentition. J. Prostho; 10:224-233.
- Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. Sterrett JD, Oliver T, Robinson F, Fortson W, Knaak B, Russell CM. J Clin Periodontol. 1999 Mar;26(3):153-7
- Dentists’ preferences of anterior tooth proportion-a web-based study. Rosenstiel SF, Ward DH, Rashid RG. J Prosthodont. 2000 Sep;9(3):123-36
The following case reports on a patient initially referred for dental implant rehabilitation of posterior segments who, following comprehensive planning, elected for an entirely different treatment option.
The case
The patient was a 60-year-old female with a heavily restored upper and lower dentition. She was referred
for possible implant replacement of upper and lower posterior dentition.
Previous dental history
She was a regular attender with significant restorative care over her lifetime, most recently restorations and tooth loss required as teeth have failed due to loss of tooth structure.
Last treatment was fabrication of a new upper p/- chrome and RCT of lower 6s following crown loss.
Medical history
Slightly elevated blood pressure, controlled, otherwise clear.
Patient requirements/goals
- Aesthetics was the highest priority. She disliked the spaces in the upper and lower posterior segments as well as visible clasps of upper chrome (Fig 1).
- Longevity and planning for future problems was important.
- She would also like to improve function.
Patient assessment
Extra-oral
Soft tissue assessment – no abnormalities detected.
Smile line – medium/high, showing gingival margins during a wide smile.
Intra-oral
Soft tissue assessment – no abnormalities detected.
Teeth present:
7__4321 – 12345_7
76__321 – 123__67
(Figs 2-4)
Restorative status and prognosis of remaining teeth:
Maxillae
Eleven teeth remain, having had premolars on either side previously removed. Of the 11 remaining teeth, all of them are restored, with the eight upper front teeth having full coverage crowns (which have apparently been present for about 20 years). Three of these have root canal treatment and posts. The root fillings are all inadequate, with short posts.
No significant periapical pathology. A number of the crowns do not fit the underlying teeth, with the possibility that secondary dental decay is ingressing. The three root-filled teeth are sufficiently heavily restored that further treatment is unlikely and they are likely to be lost in the future.
The remaining back teeth on both sides, while again heavily restored, do appear sound at this time. There are no immediate dental restorative needs in the upper arch, just the concern that, as and when problems occur with the crowns in the upper front teeth, these teeth will be lost (Fig 5).
Mandible
Ten teeth remain, again having lost premolars on either side. The lower six remaining front teeth, other than being slightly discoloured, are intact with minimal restoration and good prognosis. The second molars on either side have direct placement silver amalgam restorations, but are otherwise sound with good prognosis.
The first molars on either side recently had temporary crowns placed following root canal treatment. Radiographs show incomplete root canal fillings and insufficient tooth structure for predictable re-restoration (Fig 6).
- Visible clasp from existing denture
- At presentation
- Right lateral view
- Left lateral view
- Upper full arch mirror view
- Lower full arch mirror view
- Existing removable restorations
- OPG
- Radiographs of upper anteriors
Existing removable restorations
The upper denture is a cobalt chrome reinforced denture with a palatal strap and visible buccal clasping. In the lower, there is a temporary all-acrylic denture (Fig 7).
Periodontal condition
BPE
1/1/1
0/2/1
Full chart not required.
Oral hygiene was fair, some areas of supra and subgingival plaque deposits. OHI practical required for effective plaque removal.
Occlusal assessment
TMJ healthy – full range of motion and no pain on loading.
Centric relation – first point of contact UL7 /LL7 and less than 1mm vertical slide to centric occlusion.
Guidance – group function on both sides with non working side interferences on both lower 7s.
Interarch spacing – limited above roots of lower 6s.
No evidence of significant parafunction.
Aesthetics
Medium/high smile line showing gingival margins of all upper anterior crowns and clasps of p/- chrome.
Unaesthetic old PFM crowns, poor width/length ratio, unaesthetic margins.
Lower spacing evident.
Staining and colour mismatch from restorations to remaining tooth structure.
Radiographic assessment
OPG – no non-dental issues, assessment of vertical bone height for possible implant placement suggest favourable situation in the lower arch with the need for bilateral sinus augmentation in the upper. (Fig 8 – OPG).
Periapical radiographs – upper anterior dentition heavily restored with root canal fillings, posts and crowns on teeth, no significant apical pathology (Fig 9 – periapical radiographs).
Diagnosis
Reduced aesthetics and function as a result of repeat restoration and tooth loss in a heavily restored dentition, with a high likelihood of further tooth loss, especially in the lower posterior and upper anterior sextants.
Discussion/treatment options
The patient was initially referred for possible implant replacement of missing posterior teeth in both arches. Initial assessment would suggest this as a reasonable and predictable way of restoring the posterior sextants to full function, with good bone height available in the lower and predictable augmentation likely in the upper.
Critical in any case assessment, however, is the overall assessment of the full mouth in order to predict, as far as possible, where problems will next occur and how they can be managed within the context of the planned treatment. This is never more important than when considering dental implants.
However it is managed, dental implant treatment is a costly process, financially and in terms of what patients may have to endure. It is important that, if we can predict that more implants are likely, the patient is made aware of this at the outset of treatment. Often a patient will stretch themselves for the treatment they have been told they need, but be unable to rise to additional complex treatment in the future.
Therefore, we need to look to the evidence available in order to predict what may happen to a heavily restored dentition. With this information, the patient is then much better informed and able to make the right decision about their care. In addition, as clinicians we are much better able to manage a situation if we have predicted and explained it in advance.
In compiling the treatment plan, advice on evidence-based prognosis and treatment outcomes was sought from specialist clinicians in prosthodontics, oral and maxillofacial surgery and endodontics.
With this particular case, the restorations most at risk of future failure are the upper post crowns. Due to the proximity of a number of post crown restorations, failure of any one would result in a significant challenge:
- Tooth loss will result in unaesthetic apical migration of the gingival margin.
- Fixed bridgework is unpredictable due to lack of structural integrity of adjacent teeth.
- Lifting a flap for implant placement, in the upper anterior sextant, will likely result in exposure of the crown margins on adjacent teeth. Restoration of these teeth to manage this would again be unpredictable due to lack of ferrule and structural integrity.
- Were it either of the lateral incisors that was lost, implant placement would be in a less than ideal strategic position, given that future tooth loss is likely.
Discussing the situation with the patient involves presenting the information in such a way that they can balance their wishes, what is possible and what is affordable both now and in the future.
In this case, we established that to resolve the original concerns, a minimum of two implants would be required in the upper arch and four in the lower.
Multidisciplinary planning suggests that additional treatment as problems arise in the upper would likely result in an additional two to four implants carried out in a “piecemeal” approach on an “as required” basis.
Many patients are happy to accept this and proceed as they originally intended. Here, however, the patient felt that their previous experiences and our observations meant further treatment would be highly likely and that they could not, and did not wish to, afford piecemeal implant dentistry.
The patient was willing to compromise their criteria to accept “removable” rather than “fixed” restorations if their other wishes could be achieved.
We therefore looked to provision of removable chrome reinforced partial dentures, designed in such a way as to achieve as many of the patients original wishes as possible as well as managing predicted future problems.
Agreed treatment:
Upper arch
Using a modified RPI (rest/plate/i-bar) system (Equipoise System), we were able to design an upper removable partial denture that did not show any of the metal clasping which had been bothering the patient. In addition, by opening the occluso-vertical dimension, in centric relation, it was possible to provide an anterior chrome bite platform that would both limit functional and para-functional forces on the existing post crowns while providing support for possible future tooth addition as and when required.
Lower arch
A “rotation” type chrome was fabricated to rest on composite additions to the lingual of the lower anteriors and within distal undercuts. The interocclusal space was limited over the remaining roots of the first molars, deeming them unsuitable as potential overdenture abutments, and these were therefore removed three months before restoration fabrication.
During treatment, the patient was instructed on optimal oral hygiene for the existing and planned restorations.
Treatment progression
Figs 10-18.
- Left lateral completed case
- Right lateral completed case
- Upper fitted
- Upper and lower chromes fitted
- Try-in of Equipoise framework
- Upper Equipoise framework
- Lower rotational denture fitted
- Completed lower rotational chrome
- Composite rests lingually on lower canines
Conclusion
A case has been presented demonstrating comprehensive, multidisciplinary, treatment planning as a result of which the patient chose a different treatment option from that which they had originally intended.
Planning advanced restorative dental care, in an already heavily restored dentition, is a complex and challenging process. If predicable results and patient satisfaction are to be achieved, then informing patients fully of all potential outcomes and possible future complications is essential at the outset.
About the authors
This article was submitted by Edinburgh Dental Specialists.
References
References available by request, email Tele-dentist@edinburghdentist.com for more information.
The members of the dental team hold a unique position in the safeguarding of children. This article seeks to highlight the important role of each member of the dental team in the safeguarding of children and aims to ensure that passivity related to this issue will become a thing of the past.
Dentists and dental care professionals (DCPs) are not expected to make the often difficult decision to remove children from abusive carers, but should be confident in their professional responsibility to highlight and escalate concerns in an appropriate and timely manner. The importance placed on this professional duty is supported by the recent changes to recommended Continuing Professional Development (CPD) topics by the General Dental Council (GDC), with the addition of safeguarding children and young people added in April 2015.
The professional standards expected of every member of the dental team regarding safeguarding are clearly stated in the Standards for the Dental Team GDC guidance1 and highlighted below:
Standard 1.9
You must find out about laws and regulations that affect your work and follow them.
1.9.1 – You must find out about, and follow, laws and regulations affecting your work. This includes, but is not limited to, those relating to:
- data protection
- employment
- human rights and equality
- registration with other regulatory bodies.
Standard 8.5
You must take appropriate action if you have concerns about the possible abuse of children or vulnerable adults.
8.5.1 – You must raise any concerns you may have about the possible abuse or neglect of children or vulnerable adults.
You must know who to contact for further advice and how to refer concerns to an appropriate authority such as your local social services department.
8.5.2 – You must find out about local procedures for the protection of children and vulnerable adults. You must follow these procedures if you suspect that a child or vulnerable adult might be at risk because of abuse or neglect.
What is child abuse?
- The national guidance for child protection in Scotland 2010 describes abuse as “forms of maltreatment of a child”.2 This can be caused by significant harm directly to the child or failing to act to prevent this harm occurring. In this guidance there are four recognised types of abuse:
- Physical abuse: causing of significant physical harm to the child: examples are shaking, hitting, burning and choking.
- Emotional abuse: continued emotional neglect or ill treatment that has a detrimental and long-term adverse effect on a child’s emotional development. This can be caused by the child being made to fear their guardian, or feel worthless. In all types of child abuse, there will be an emotional factor attached.
- Sexual abuse: any child involved in any activity for the sexual gratification of another person. This is irrespective of whether it is claimed that the child has consented to the act. These activities can be physical or non physical, which includes using sexual language towards a child.
- Neglect: “persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of the child’s health or development”. This general neglect may result in the child being diagnosed with “non-organic failure to thrive”, meaning that the child has significantly failed to reach the normal weight, growth and development levels of those of similar age.
Child abuse is rarely inflicted on a child by a stranger, it is much more likely to occur by someone who is known to the child whether that is a direct relation or not. Radford, L et al (2011)3 states that over 90 per cent of sexually abused children were abused by someone they knew, and that one in 20 children have suffered from some kind of sexual abuse.
Dentists may be the only healthcare professionals that “at risk” children visit, so it is important that a thorough examination is carried out. Children are likely to have bumps and bruises, however the location of these injuries may make you suspect that there is a non-accidental cause. Dental trauma can also be a presentation of child abuse, so it is important to obtain a clear history of the incident from both the child and the parent.
Aspects to consider when carrying out this examination are:
- Do the child’s and parent’s stories match?
- Does the story change when being retold?
- Do the parent and child have a normal relationship?
- How is the child’s demeanour in the surgery?
- Do the injuries match the description of the incident?
- Is there a history of trauma?
As dental professionals, we are not expected to diagnose these types of abuse, nor are we qualified to tackle such sensitive issues alone. This being said, we must be able to recognise patients who are at risk, look out for the signs of abuse and know when and with whom we should share our concerns. (Figs 1 and 2)
What is dental neglect?
The British Society of Paediatric Dentistry defines dental neglect as “the persistent failure to meet a child’s basic oral health needs, likely to result in serious impairment of a child’s oral or general health or development”.
Dental decay is a disease that is almost completely preventable yet, the most common cause for a child to be admitted to hospital is for tooth extraction under general anaesthetic (GA).4 There are numerous factors contributing to this issue and in isolation they should rarely raise suspicion about the care the child is under. The child’s general health, social-economic status and previous dental experience should all be considered when deciding if you have concerns for a child’s welfare.
Some features, which cause particular concern, are:
• Severe untreated dental disease, especially if it can be noticed by a non-dental health professional
• Disease that is significantly impacting upon the child
• Parents/carers that have access to treatment and dental care but persistently fail to obtain treatment for the child
• Repeated failed appointments
• Failing to complete treatment plans
• Only returning for emergency appointments
• Repeat GAs for dental extractions.
If a child’s dentition is neglected they may experience toothache, loss of sleep and have difficulty eating. They commonly have repeated courses of antibiotics, have only attended the dentist for emergency appointments and have had repeated GAs. All these factors increase the likelihood of the child to grow up having an overall negative perception of the dentist. These children are therefore more likely to be dentally anxious adults and continue the pattern of attending only for emergency care, which creates a vicious cycle for generations to come.
Dental neglect can be part of a wider problem in the child’s life and it is important to decide whether you need to raise your concerns. If, after repeated failed appointments to complete treatment and a discussion with the parents regarding your concerns you are still not satisfied, then you must share your concerns.
- Typical features of accidental injuries
- Typical features of non accidental injury
- The GIRFEC Wellbeing Wheel
- Child Protection and the Dental Team: Flowchart for action
What is the relevant legislation and how is this applied to dentistry? UN Convention on the Rights of the Child 1989 5
This international treaty states that the best interests of the child should be a primary consideration and children should be protected from all forms of physical or mental violence, injury, abuse or neglect. The core values from the Convention underpin the ethos of all subsequent legislation regarding child protection.
Scottish Legislation
Legislation passed within Scotland is of most relevance to dental teams working in Scotland and are detailed here:
Children’s Act Scotland 1995 6
This act has incorporated key defining principles of the UN Convention on the Rights of the Child into Scottish law. This act works to promote child welfare, preventing discrimination and ensuring ‘the voice of the child’ is heard.
Children and Young People Scotland Act 2014 7
This act is the legislative embodiment of the Scottish Government’s ambition for “Scotland to be the best place to grow up in by putting children and young people at the heart of planning and services”. The legislation from this act is currently in the process of being implemented through “Getting it Right for Every Child” (GIRFEC).8
The GIRFEC Wellbeing Wheel (Fig 3) shows eight areas of wellbeing, which if all are attained, should enable the child to grow and develop into a healthy and well rounded individual. It has also highlighted the need for an improvement in “joined up working” between agencies, education and healthcare. To facilitate this co-operation, two key roles have been identified, which are discussed below to help members of the dental team understand their roles and how to communicate effectively with these role-holders.
Who is the Named Person?
A Named Person should be appointed for every child in Scotland from birth until their 18th birthday or until they leave secondary education. The role will usually be given to someone already known to the family, for example the health visitor or a senior teacher. The Named Person should be used as a starting point for specific concerns. It could be useful for a general dental practitioner to make a record of a child’s Named Person, for example at their first appointment, in case contact regarding a concern is ever required.
The Named Person’s role is to act as a single point of contact, and to instigate further help, advice and support. They can support the family’s confidence to raise their personal concerns and to ensure the young person’s views are heard.
The infrastructure supporting the provision of Named Persons is currently being rolled out nationwide and may not yet be in place everywhere. We advise that you check locally regarding the stage of implementation that has been reached so far in your area.
Who is the Lead Professional?
When two or more agencies are involved in helping a child or young person, a Lead Professional will be appointed. The Lead Professional holds a number of responsibilities, from acting as the main point of contact, to promoting interagency working to supporting the child through crucial transitional stages.
This role is usually undertaken by a social worker. A dentist would not be expected to undertake the role of either a Named Person or a Lead Professional, but to simply consider contacting these individuals with concerns.
What is expected of me and what do I do if I have a concern?
The protocols for this scenario are clearly outlined in the flowchart in Figure 4, which has been taken from ‘Safeguarding Children and Young People: A Guide for the Dental Team’.9
The first concern should be to obtain as detailed a history and examination as possible, as these records may be relied on later as evidence. Negative findings as well as positive are important to record. Important questions to consider have been discussed earlier in this article. Regarding examination, it is important to examine the child thoroughly, noting any facial, oral or dental injuries. You should also appraise the overall appearance of the child: do they appear well cared for or are they “failing to thrive?” The child’s interaction with their carers can give insight into the presence or absence of abuse within the relationship.
You should always make it a priority to discuss any injuries with the child and allow them the opportunity to tell their story if they volunteer it. Do not ask leading questions and always take disclosures seriously. You should listen to the child in a non judgemental way and remain calm.
It is extremely important that you treat any injuries or symptoms appropriately, and the child should not be left in pain.
Your next consideration should be to discuss your findings with an experienced colleague to gain their insight into the situation.
If your concerns remain following this discussion, you should follow your local protocol by referring to your local social services department, the police, Area Child Protection Committee or equivalent. Referrals should be made by telephone, and should be followed up in writing within 48 hours. Ensure that the telephone conversation is documented in your clinical record, along with a clear action plan.
Best practice would indicate you should discuss your concerns with the parents and child, and inform them of your intention to escalate your concerns. Each case should be assessed individually, and it is reasonable to not disclose to the parents if you feel by doing so the child would be placed at greater risk or the referral would be unnecessarily delayed.
Comprehensive medical assessments (CMAs) are a common tool employed to compile evidence in suspected cases of child abuse/neglect. A paper published recently in the British Dental Journal10 explored the impact of dental input into CMAs conducted in Glasgow in recent years and clearly illustrates the importance of co-operation between different healthcare specialties. The two case studies described in this article are extremely useful learning tools. Common themes are revealed with regard to “at risk” children including multiple failed healthcare appointments, signs of dental neglect and the general appearance of the child. The case studies are an important opportunity to reflect upon your own clinical learning, including:
- Have I seen a patient with a similar presentation?
- Did I feel something was not quite right?
- Did I ask the right questions?
- Would I do anything differently the next time?
The dental practice as a whole can also reassess their practice policies with regard to safeguarding, and ask the question: “What measures have we put in place to ensure our paediatric patients are safe and healthy?” For example, policies regarding missed appointments should not punish or exclude the child patient, and patterns can become obvious more quickly if all the siblings of the same family are linked and their attendance patterns monitored as a unit.
Empowering the dentist and other DCPs to have the confidence to realise and utilise their role in safeguarding is paramount. General dental practitioners should be encouraged to discuss their concerns with colleagues within the practice and liaise with other healthcare professionals. For example, a telephone call to the patient’s general medical practitioner to ask their opinion on a patient’s unkempt appearance or uneasy interaction with their carer. Verbalising a concern does not automatically lead to social work involvement or a court case, but it is always better to be safe than sorry.
Conclusion
Recognising child abuse, in particular dental neglect, is an important part of dentistry and must be followed up in an appropriate manner to make sure that children do not slip through the care net. With new legislation coming into place in Scotland and the GDC recommending safeguarding of vulnerable children and young people as a CPD topic, dentists should understand their role in child protection.
As previously mentioned, dentists are not expected to make the diagnosis of child abuse, however they may be the only health professional a child is coming into contact with, so any relevant findings should be raised appropriately. Healthcare professionals should be moving away from assuming that someone else will voice concerns about a child, as this can allow a cycle of neglect or abuse to continue. The only way this can be achieved is by knowing when it is appropriate to seek help and by focusing on multidisciplinary communication and care for each vulnerable young person.
References
1. Standards for the Dental Team, GDC, 2013.
2. National Guidance for Child Protection in Scotland 2010. www.gov.scot
3. Radford, L.et al. Child abuse and neglect in the UK today. London: NSPCC. 2011.
4. C L Stevens. Is dental caries neglect? British Dental Journal. 2014; 217: 499-500.
5. UN Convention on the Rights of the Child, United Nations, November 1989.
6. Children’s (Scotland) Act 1995
7. Children and Young People (Scotland) Act 2014
8. GIFREC – Getting it Right for Every Child, Scottish Government publication
9. Harris J, Sidebotham P, Welbury R, Townsend R, Green M, Goodwin J, Franklin C. Child protection and the dental team: an introduction to safeguarding children in dental practice. Sheffield: Committee of Postgraduate Dental Deans and Directors (COPDEND) UK, 2006. www.cpdt.org.uk
10. C. M. Park, R. Welbury, J. Herbison & A. Cairns. Establishing comprehensive oral assessments for children with safeguarding concerns. British Dental Journal. 2015; 219: 231 – 236.
About the authors
Catherine McCann, BDS, MFDS(RCPSG). Core Trainee 2
Myles Gillespie, BDS. Core Trainee 1
Gillian C Glenroy, BDS, MFDS (RCPSG), MPaed Dent (RCSEd). Specialist Dental Officer- Paediatrics,
Public Dental Service, NHS Greater Glasgow & Clyde.
With each turn of the wheel of time the societal prejudices of the western world have slowly been eroded away. The ethos of pioneering equalitarians from Abraham Lincoln to Emmeline Pankhurst and Martin Luther King Jnr. has begun to resonate within our modern society to include vulnerable adults. As a privileged profession charged with the duty of caring for our patients, the holistic healthcare practice we undertake must endeavour to include safeguarding to protect and promote the welfare of vulnerable people.
The population of Scotland is ageing1 and the number of people living with chronic medical conditions requiring treatment is rising.2 This is in part due to medical advances, whilst environmental and social changes including improvements to living and working conditions have also contributed. Prolonged life can come at a cost as, with pre-term birth rates increasing, there is also a resultant poorer long-term health outlook for these individuals3 whilst those nearing death later in life are kept alive as a result of advanced medical intervention and current ethical beliefs. There is predicted to be a future explosion in the rate of dementia diagnoses burdening our already stretched health and social care systems.4 One to three people in every 100 suffer from bipolar disease or schizophrenia5 and while often they manage well with their condition they may go through periods of being acutely unwell. Collectively, these points illustrate the number of people within our society who are likely to be vulnerable at some stage in their life.
The neglect and abuse of many vulnerable people has been brought to light in multiple arenas including The Francis Report6 which has propelled the issue of adult protection into the foreground of healthcare. Appropriate multi-level measures must now be put in place to ensure these events are never allowed to happen again. This neglected issue must now become a priority for education and training to ensure the profession is able to perform its important role in safeguarding.
Safeguarding
Safeguarding involves a spectrum of measures with the purposes of:
- Preventing harm and promoting welfare
- Protecting individuals from harm
Safeguarding is more than an acute response to abuse or neglect. It incorporates anticipatory methods which actively seek to improve the welfare of individuals potentially at risk and prevent harm. This role is inclusive of the dental profession as many vulnerable adults experience poor oral health.7 Addressing oral health and its common risk factors in order to promote welfare requires input at all levels, from government policy to the essential practices of the clinician.
Protecting Vulnerable Groups Scotland
The Protection of Vulnerable Groups Scheme (PVG) came into existence in 2011.8 Its purpose was to improve the disclosure process to better protect both children and vulnerable adults. This measure, whilst not foolproof, is a worthwhile system and plays a vital role in preventing predators and those willing to abuse positions of trust from gaining access to vulnerable groups.
Application to the scheme is necessary for anyone who takes part in regulated work with children or protected adults. This includes dentists and dental care professionals. It is essential as employers, dental practitioners and health boards are actively involved in ensuring all employees are registered with the scheme.
For the purposes of PVG a protected adult is defined as an individual aged 16 or over who is provided with a type of care, support or welfare service and includes health services.
Application to the scheme instigates a search of registers to determine if the applicant is barred from working with vulnerable groups. Further vetting information is acquired from agencies to determine if the individual has any convictions, cautions, children’s hearing findings or if there is any other additional police information of interest. On receipt of this information, Disclosure Scotland decides on the suitability of the person to perform a role with at-risk groups. One of the benefits of this new disclosure system is that it will be continually updated. Thus any new information which may affect an individual’s position will be recorded and employers informed.


Adults with Incapacity Act
As users of health services we have an expectation that our choices in relation to the treatment we receive will be respected and honoured. Some people are unable to make decisions or communicate their decisions as a result of dementia, learning disability, acquired brain injury, mental illness or severe sensory impairment.
Yet, they still have a right to healthcare which ensures their wellbeing is protected. As a profession we must respect these basic human rights and utilise the existing processes which seek to protect vulnerable adults in relation to the provision of medical and dental treatment.
While this article cannot cover every aspect of the Adults with Incapacity Act nor its clinical applications, it must be touched upon to allow the reader to appreciate its role in the safeguarding of individuals who lack capacity.
The Adults with Incapacity Act was passed by Scottish Parliament with the intention of “safeguarding the welfare and managing the finances of adults who lack capacity due to mental disorder or inability to communicate due to a physical condition”.9 Part 5 of the Act specifically relates to medical treatment and research. It plays an essential role in the safeguarding of patients who lack the capacity to make decisions about healthcare and are reliant upon others to make a decision on their behalf.
For the purposes of the Act, incapacity is defined as being incapable of:
(a) Acting; or
(b) Making decisions; or
(c) Communicating decisions; or
(d) Understanding decisions; or
(e) Retaining the memory of decisions,
It must be reinforced that capacity is not an all or nothing entity and each decision must be made on an individual basis. Equally, the stigmatisation of every person with a learning disability or other medical disease affecting cognitive ability being unable to consent is completely wrong; we must assume capacity until proven otherwise ensuring it is an active process. Each decision in relation to capacity is procedure specific. It may be that a patient is able to consent for certain procedures but not others – if a procedure were complex, or involved multiple risks, then a patient may not be able to consent despite the ability to do so for something more straightforward.
It is the responsibility of the dental practitioner to initially assess capacity. The process is not always black and white but can be established using a simple question and answer conversation. The patient must have the ability to understand what the procedure will involve, why it is required, the benefits and risks of that procedure, and the consequences of having no treatment. The patient must then be capable of making a decision based on the information they have been given, and communicate that decision (with aids if required). Asking your patient to explain to you in their own words their understanding of information you have given them about the procedure or treatment is one way of doing this. It is also worth remembering that some adults who lack capacity one day may not be in the same condition the next. Fluctuation in capacity necessitates continual reassessment.
If the person is deemed not to have capacity, and treatment is being considered, it is important that the principles of the Act are followed (Fig.1).
The next stage in the process would be for the practitioner to determine if the person without capacity has in place a welfare power of attorney, welfare guardian or person appointed by an intervention order (proxy) who should be consulted prior to the provision of any treatment. Where none of these individuals are in place a nearest relative should be consulted. Only if consent is given on the individual’s behalf should an Adults with Incapacity (Scotland) Act section 47 form be completed prior to the provision of treatment. An exception to this rule is the provision of essential emergency care, whereby as long as the principles are observed it may be correct to provide treatment without undertaking the capacity process described. These situations are few and far between in dentistry and should subsequent treatment be required an appropriate section 47 should be completed as required.
Only a few dental practitioners in Scotland have the training necessary to legally assess capacity and sign a section 47 form. However, every dentist must assess capacity before providing treatment. For the practitioner without this training there is a responsibility to contact the patient’s general medical practitioner, who is able to assess capacity in the eyes of the law and sign Section 47 forms. The dental practitioner can provide a treatment plan to the patient’s doctor listing the treatment intervention necessary and should the patient be deemed to lack capacity it can be signed off.
At present, dental treatment requires financial payment if an individual is not in receipt of exemption. A proxy involved in the consent process may also hold financial powers for an individual. If the proxy is refusing necessary treatment which is in the best interests of the person without capacity on financial grounds the intentions of that individual should be questioned. If the dental practitioner is certain that all the principles of the Act have been followed then it may be necessary to raise concerns with the local authority about the suitability of that legal guardian.
The importance of this Act to the safeguarding of vulnerable people should not be underestimated. Without education and training the profession cannot fully embrace the benefits of this Act and ensure the safety of those who lack capacity. There is a clear need for educators to disseminate their knowledge and skills at both undergraduate and postgraduate levels to improve the Profession’s use of the Act and ultimately the safety of our patients.
Until then there must be an opening of the channels of communication, to remove the barriers to care, between dental practitioners without the necessary training and general medical practitioners who can assess capacity on their behalf. Equally, dentists with expertise in this area are most numerous in the Public Dental Service and must be open to discussing such issues with colleagues as we throw away the compartmentalisation of services and work together as a team for the benefit of patients and practitioners alike.
The Adult Support and Protection (Scotland) Act 2007
The Adult Support and Protection (Scotland) Act 2007,10 is the core piece of legislation relating to the protection of potentially vulnerable adults in Scotland. Its role is to support and protect those members of society who are (or are likely to be) at risk of harm through their own conduct or that of others. The term harm when applied is specific to each individual but may include conduct which is physical or psychologically harmful, adversely affects property rights or interests and self-harm.
The Act defines adults at risk as persons aged 16 or over, who:
a) are unable to safeguard their own well-being, property, rights or other interests,
b) are at risk of harm
c) because they are affected by disability, mental disorder, illness or physical or mental infirmity, are vulnerable to being harmed than adults who are not so affected.
As a three-point test, all features must be present to say an adult is at risk. One of the fundamental themes of the Act is to ensure that where an individual is at risk any response should be multi-disciplinary necessitating the need for co-operation between bodies including health boards. Vulnerable individuals often interface with multiple services which may hold information of value in protecting that individual. When access to information is required during an investigation under the Act, the oral health practitioner has a duty to co-operate. In rarer instances the oral health physician may be asked to perform an examination and provide evidence in cases of neglect or physical harm which include traumatic injuries to the head and neck.
Table 1: Types of abuse and examples of possible indicators (adapted from Social Care Institute forExcellence)12
| Type of abuse | Definition | Example of possible indicators |
|---|---|---|
| Physical | The non-accidental infliction of physical force that results in bodily injury, pain or impairment |
|
| Sexual | The direct or indirect involvement of the adult at risk in sexual activity or relationships, which they: 1. Do not want or have not consented to 2. Cannot understand and lack the mental capacity to be able to give consent to 3.Have been coerced into because the other person is in a position of trust, power or authority (for example a care worker) |
|
| Psychological / Emotional | Actions or behaviour that have a harmful effect on the emotional health and/or development of an adult who is at risk |
|
| Financial | The use of a person’s property, assets, income, funds or any resources without their informed consent or authorisation. |
|
| Neglect and Acts of Omission | The failure of any person, who has responsibility for the charge, care or custody of an adult at risk, to provide the amount and type of care that a reasonable person would be expected to provide. Neglect can be intentional or unintentional. |
|
| Institutional | Is the mistreatment, abuse or neglect of an adult at risk by a regime or individuals. |
|
Protection of adults
The very essence of humanity must be questioned when we read of the events at Winterbourne View Hospital.11 People with a learning disability and autism were cold-heartedly abused by those they were dependent upon for care. This report has been succeeded by further discoveries highlighting a shameful lack of care including the neglect witnessed at a Mid Staffordshire hospital. Francis, in his seminal report, gave a framework from which the NHS could move forward into a brighter dawn and regain the respect it once possessed as the shining beacon of the world’s healthcare services. As lessons are learned and grand plans are made to prevent further such instances, each and every dental practitioner has a role to play at the front line.
The dental practitioner may undertake domiciliary work visiting a patient’s own home, care home or supported housing whilst other dentists may work within a hospital setting. Privileged access to these environments should never be taken for granted as they provide a vantage point from which concerns about the safety of an individual or group may come to light. Equally, such signs may present in the patient who attends the surgery.
Empowerment is important, both for the adult at risk but also for the practitioner who has concerns. We must have the confidence to be able to report concerns to ensure safety and provide a vital link in the chain. We often interface with care environments more often than other healthcare colleagues and have built up trusting relationships with our patients for years such that they are able to disclose concerns to us.
The types of abuse and indicators vary but the dental practitioner must always remain vigilant and alert to potential signs. Table 1 provides some of the key types of abuse and the indicators which are most likely to be encountered.
Whilst being aware of the potential for abuse, we must appreciate that dental neglect, particularly in our older population, is complex. At face value there is no doubt that many older people resident in care homes have their oral health neglected and in no way can this be deemed acceptable. Yet, there are multiple barriers to the provision of oral care in this setting.
Work is currently being undertaken at The University of Glasgow Dental Hospital and School to gain a better understanding of these factors with the ultimate aim of improving oral health and quality of life for these people. At present, The Caring for Smiles Programme is being rolled out across the country as an intervention to improve the oral health for residents in care homes. The success of the programme is yet to be fully evaluated but the initial response appears promising, yet true success is dependent on high standards being maintained in the long term.
The Adult at Risk
The healthcare professional has a duty of care and a responsibility to report and record any concerns, suspicions or disclosures made by or about an adult who may need protection. Every dental practice and health board should have a protocol in place should such an event occur.
The role of the dental practitioner in adult protection is three-fold:
- Recognise – Being able to identify an adult at risk
- Respond – Manage the acute situation and inform other services as required
- Record – Document and report in detail the information obtained and the actions taken
If concerns arise or a disclosure is made to the practitioner the following steps outline the initial management:
- Remain calm and reassure the individual
- Seek further information – obtaining who, what, when, where and why?
- Record the information given
- Inform person of the your next actions.
A non-judgemental approach is important while no attempt should be made to contact the alleged perpetrator nor should forensic evidence be removed. No promises should be made to the individual or assurances that you will keep any secrets.
Should there be concerns about the immediate safety of the individual the emergency services (police or ambulance services) should be contacted.
The capacity of the individual is not of primary importance in a life-or-limb situation and therefore, in an emergency, it is acceptable to contact services without the person’s consent. When contacting emergency help, the practitioner should never put themselves at risk and should always undertake appropriate risk assessment ensuring they are in a safe environment from which to communicate.
Responding to issues which are not of immediate urgency should involve a line manager in the first instance. This should facilitate discussion around the information available, the capacity of the person to consent and what action, if any, should be taken. If action is required contact with social services should be made within 24 hours.
If the individual lacks the capacity to consent then in those circumstances a referral to the local social work department should be undertaken. However, if the individual has capacity, the only instances where referral can be made without consent are if:
- a person is, or may be, an adult at risk, and action needs to be taken in order to protect that person from harm;
- there is an issue of public safety.
- the person is/may be a service provider, and other people may also be at risk.
A referral should be made by telephone initially to the local social work department and followed up in writing by the practitioner. In such matters communication is essential, even if you are only seeking advice it is better to do so than neglect your duty. The process of actions undertaken by social services and associated agencies should an adult protection issue be raised are briefly outlined in Figure 2.
The recording of every aspect of adult protection is essential to ensure there is a contemporaneous record of events. The time taken to ensure these notes are of a high standard cannot be underplayed as they are important for services to establish if the adult is at risk but also for the dentist and their associated legal responsibilities.
Conclusion
The safeguarding of adults is a key area of practice for dental practitioners and is one of the few aspects of care which, if not acted upon correctly, could result in serious harm to an individual. Safeguarding affects many areas of practice which may not have been previously considered, including PVG and Adults with Incapacity. While this article provides an overview of safeguarding, further dedicated training is necessary for the dental community to ensure we are practicing safely and are able to promote welfare and protect vulnerable groups.
References:
1. Office for National Statistics. Population Ageing in the United Kingdom, its Constituent Countries and the European Union. March 2012. http://www.ons.gov.uk/ons/dcp171776_258607.pdf
2. The Scottish Government. Scotland’s National Dementia Strategy 2013-2016. http://www.gov.scot/Resource/0042/00423472.pdf
3. Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, Quigley MA. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ. 2012 Mar 1;344:e896.
4. The Scottish Government .Living and Dying Well Living and Dying Well: A national action plan for palliative and end of life care in Scotland. 2008 .
5. Perala et al (2007) Lifetime prevalence of psychotic and bipolar I disorders in a general population Archives of general psychiatry, 64:19-28
6. Francis, R (Chair). Report of The Mid-Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office, 2013. http://www.midstaffspublicinquiry.com/report
7. Daly, B. Disability in Oral Health, Social Inequalities from evidence to action. ICOHIRP. Published: UCL. 2015
8. Disclosure Scotland. The Protection Vulnerable Groups Scheme. 2011. http://www.disclosurescotland.co.uk/disclosureinformation/pvgscheme.htm
9. Adults with Incapacity (Scotland) Act, 2000. http://www.legislation.gov.uk/asp/2000/4/contents
10. The Adult Support and Protection Act (Scotland), 2007. http://www.legislation.gov.uk/asp/2007/10/contents
11. The Department of Health, England. Transforming Care: A National Response to Winterbourne View Hospital. https://www.gov.uk/…/final-report.pdf
12. Social Care Institute for Excellence. Identifying the Signs of Abuse. http://www.scie.org.uk/…/Identifying-the-signs-of-abuse.pdf
About the Authors
Nicholas G. Beacher, BDS, MFDS (RCPSG) Clinical Lecturer and Honorary StR in Special Care Dentistry. University of Glasgow Dental School, School of Medicine, College of Medical, Veterinary & Life Sciences, Glasgow, UK
E-mail: Nicholas.Beacher@glasgow.ac.uk
M. Petrina. Sweeney, BDS, MSC(Med Sci), DDS, FDS (RCPSG) Senior Clinical Lecturer and Honorary Consultant in Special Care Dentistry. University of Glasgow Dental School, School of Medicine, College of Medical, Veterinary & Life Sciences, Glasgow, UK
Gillian C. Howie, BDS Longitudinal Dental Foundation Trainee, NHS Lothian.
More than 500,000 people in Scotland currently take one or more anticoagulants or antiplatelet drugs to treat or prevent thrombotic events1. It is, therefore, very likely that at some point most dentists will encounter such patients, under circumstances where they require dental treatment likely to cause bleeding.
The primary concern for those performing dental procedures on this patient group is likely to be the potential for bleeding complications due to the drugs’ effects on clot formation, and the practitioner’s aim will be to manage the bleeding risk through the use of appropriate treatment planning and haemostatic measures. However, given the variety of these drugs and the other factors that can influence bleeding risk, deciding on the best course of action for an individual patient is often not straightforward.
Various guidelines exist nationally and internationally, providing advice and recommendations for the dental treatment of patients taking the most commonly used of the drugs, including the oral anticoagulant warfarin and the antiplatelet agents aspirin and clopidogrel2-7. These drugs have been in use for a number of years, allowing for the accumulation of significant dental clinical experience and evidence to underpin best practice.
However, since 2008, several new anticoagulant and antiplatelet drugs have entered the UK market and are being increasingly prescribed for cardiac and thrombotic conditions. Dabigatran, rivaroxaban and apixaban belong to the group of so-called novel oral anticoagulants, or NOACs (also known as direct oral anticoagulants; DOACs, or target specific oral anticoagulants; TSOACs)8. These are a newer class of oral anticoagulants that act in a different way to warfarin, by directly inhibiting specific components of the anticoagulation cascade. New antiplatelet drugs prasugrel and ticagrelor also became available at around the same time and are usually prescribed in combination with aspirin as dual antiplatelet therapies.
The availability and increasing use of these new anticoagulants and antiplatelet drugs has driven the need for new guidelines to assist dental practitioners in the management of patients taking them. Currently, local guidelines from different Scottish health boards make conflicting recommendations for the treatment of patients taking NOACs, with divergence of opinion on whether the NOACs should be interrupted for invasive dental procedures or not. This has the potential to lead to variation in dental treatment for the patients taking these anticoagulants. The conflicting advice is also a source of concern and confusion for dentists and has resulted in calls for a single national guideline on the topic9.
New guidance
In response to the identification of this topic as a priority in oral healthcare, the Scottish Dental Clinical Effectiveness Programme (SDCEP) has developed new guidance on the ‘Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs’.
The aim of the guidance is to provide advice covering both the new and the conventional drugs, with clear recommendations for the management of invasive dental treatment for this patient group. The guidance was published in August 2015 and printed copies have been distributed widely to members of the dental profession in Scotland.
The main guidance document includes information on each of the drug groups and provides practical advice and recommendations to inform the assessment of bleeding risk and decision making for treatment planning. A quick reference guide, which provides the main recommendations and advice in an easily accessible flow-chart format, is also available.
Additional tools have been developed to support the implementation of the guidance, including printable patient information leaflets specific for the different drug types. A form for recording the contact details of key medical, dental and emergency care contacts, which can be kept on hand by dentists for use should the need arise, is also provided.
The aim of the patient information leaflets is to make patients aware of the importance of informing their dentist about all medical conditions that they have and all of the medications they are taking, even if these are non-prescribed. Ideally, these leaflets should be provided to patients identified as taking anticoagulants or antiplatelet drugs before they require an invasive procedure.
Additionally, the leaflets provide information about how the patient’s dental treatment may be affected by their drugs so as to manage their expectations with regards to the extra precautions that may be taken and to provide a basis for communication between the patient and their dentist. Also available are post-treatment advice sheets, with space for recording local emergency contact details, which can be adapted as required by dental practices and provided to patients.
The guidance and all of the supporting documents are freely available via the SDCEP website (www.sdcep.org.uk).
Development of the guidance
SDCEP’s approach to the development of this guidance was to engage the clinical knowledge, expertise and experience of a multidisciplinary group of individuals with a wide range of perspectives to provide a balanced view on the clinical questions to be addressed.
This guidance development group was chaired by Garry Sime, a senior dental officer and specialist in special care dentistry based at Broxden Dental Centre in Perth. The other 17 members of the advisory group included dental consultants of various specialities, comprising oral surgery, oral medicine, special care dentistry, oral and maxillofacial surgery and restorative dentistry. A cardiologist, a haematologist, two senior pharmacists and a general medical practitioner provided medical and pharmaceutical expertise and opinion. Three primary care dental practitioners, including one from Orkney to ensure that issues relevant for remote and rural locations were fully considered, and a dental therapist represented the views of end-users.
Importantly, the guidance development group also included a patient representative who, in addition to having personal experience of anticoagulant use, is a patient contact for the anticoagulation charity ACE (Anticoagulation Europe) and so was well placed to represent patient views and perspectives.
Scoping research with dental practitioners and patients was carried out at the outset of the project to explore their experiences and views to inform the development and content of the guidance. This research was carried out by TRiaDS (Translation Research in a Dental Setting; www.triads.org.uk), who work in partnership with SDCEP and have long-standing experience of carrying out research projects, within an established framework, to support and inform the development and implementation of SDCEP guidance10.
The TRiaDS research confirmed that, while dental practitioners were generally confident in their approach to treating patients taking warfarin or the commonly used antiplatelet drugs, there was considerable variation in the dentists’ knowledge and confidence for the treatment of patients taking the newer drugs. Variation in referral decisions was also identified. Furthermore, accurate medical history taking emerged as a significant issue from both the perspective of the dentists and the patients. Difficulties in obtaining accurate details were highlighted by dentists and uncertainty in whether this information had been collected and recorded was highlighted by patients.
The evidence to inform the clinical questions addressed in the guidance was obtained through systematic searching of the literature. SDCEP was fortunate to be able to employ the expert skills and experience of the Cochrane Oral Health Group for this task (www.ohg.cochrane.org).
The recommendations developed by the group were based on considered judgements of the evidence, where available, clinical experience and expert opinion, and on the perspectives of patients and practitioners. The balance of risks, the values and preferences of patients, and the practicalities of the proposed treatment options were all taken into consideration. In line with an increasing number of national and international guideline developers, SDCEP uses the GRADE approach (Grading of Recommendations, Assessment, Development and Evaluation; www.gradeworkinggroup.org) for assigning evidence levels and developing recommendations.
Following this approach, the evidence quality and strength of each of the key recommendations presented in the SDCEP guidance are stated clearly, so that dental practitioners can be aware of how clear-cut the recommendations are when planning treatment on an individual patient basis.
Prior to publication, the guidance was scrutinised through a national consultation process and it is endorsed by the Dental Faculty of the Royal College of Physicians and Surgeons of Glasgow and the Faculties of Dental Surgery of the Royal College of Surgeons of Edinburgh and the Royal College of Surgeons of England. Public Health England also supports the guidance recommendations.
The balance of risks
The overarching consideration when performing an invasive procedure on a patient taking any anticoagulant or antiplatelet drug is the balance of the risk of a bleeding complication if the medication is continued versus the risk of a thrombotic event if the patient’s medication is interrupted. There is insufficient evidence from which to obtain an accurate measure of the relative risks of these events for each of the different anticoagulant and antiplatelet drugs or combinations. However, the relative seriousness of the different outcomes is a very important factor to be considered in the judgements leading to the development of recommendations.
Bleeding complications following a dental procedure are usually understood to mean excessive, prolonged or delayed bleeding, or bleeding that requires unplanned measures such as repacking and suturing. In extreme and rare cases, the patient may need to attend hospital for a medical intervention such as a transfusion. While it is acknowledged that a bleeding complication following dental treatment may be a worrying or distressing situation for both patient and practitioner, these events are rarely life threatening. In contrast, a stroke caused by a thromboembolism can have a catastrophic effect on the patient, with the potential to cause serious disability and even death.
Evidence reported over the last 50 years for patients taking warfarin was analysed in a recent review article11. Of more than 5,000 patients having in excess of 11,000 dental surgical procedures carried out without interruption of their warfarin medication, only 31 (0.6 per cent) experienced a bleeding complication which required more than local haemostatic measures. In many of these cases, the patients had other medical complications such as being on combined anticoagulant/antiplatelet therapies or having excessively high post-operative INR levels which, in some instances, was attributed to antibiotic usage.
On the other hand, the records for more than 2,500 patients whose warfarin therapy was interrupted or reduced prior to a dental procedure reported that 22 (0.8 per cent) experienced a thromboembolic event, six of which proved fatal.
Furthermore, the majority of studies identified in a recent systematic review found no significant difference in bleeding complications following dental procedures when comparing patients who had continued taking warfarin with those who had modified their drug intake or were not taking any anticoagulants12. This evidence also supports the argument to not interrupt warfarin therapy for dental treatment.
Although some guidelines initially advocated warfarin interruption for dental procedures, it is no longer considered best practice to do so. Most current guidelines, including the new guidance from SDCEP, recommend that invasive dental treatments should be carried out without warfarin interruption, as long as the patient’s INR is of an acceptable level. This recommendation is consistent with documented patient preference, with evidence suggesting that patients place a higher value on avoiding a thromboembolism than avoiding a bleeding complication following a dental procedure when considering the potential outcomes of each13.
Accumulated data from studies of patients taking antiplatelet drugs also indicates that serious bleeding complications experienced while continuing their antiplatelet medication for dental procedures are rare (estimated at 0.2 per cent)14. As with warfarin, none of the bleeding complications have been reported to result in a fatality.
The evidence also indicates that there is an increased risk of a thrombotic complication if antiplatelet medications are interrupted14. The estimates vary and depend on the condition for which the patient is being treated and the duration of interruption. It is likely that the risk is highest for patients on dual antiplatelet therapy following a coronary stent.
What about the NOACs?
While the recommendations for dental patients taking warfarin or antiplatelet drugs can be informed by evidence and accumulated clinical experience, this is not the case for the newer drugs, particularly the NOACs. There is, as yet, no direct evidence reporting on the impact of the NOACs on bleeding outcomes following dental procedures. Instead, the likely effects on bleeding can only be indirectly inferred from the evidence that relates to other types of bleeding.
Large trials conducted by the manufacturers of apixaban, dabigatran and rivaroxaban found comparable rates of spontaneous bleeding events for each compared to patients taking warfarin15-17. However, how relevant these results are as predictors for bleeding following dental procedures is not clear.
Current advice from the manufacturers of the NOACs is to interrupt the medication for one to four days (depending on the drug and the patient) prior to any kind of surgical procedure. However, not all types of surgery will cause the same levels of bleeding or carry the same risk of bleeding complications.
Although not yet the case for the NOACs, the distinction in terms of extent and controllability of bleeding between general surgical and dental surgical procedures is now acknowledged for warfarin. The product sheets provided by manufacturers of warfarin provide separate advice for surgery and dental surgery, with continuation of anticoagulation therapy recommended for the latter18.
The SDCEP guidance recommendations
Key recommendations made by the new SDCEP guidance, in common with many other guidelines, are that neither warfarin nor antiplatelet drugs should be interrupted for dental procedures.
Because of the lack of evidence on which to base the recommendations for the NOACs, further deliberation was carried out by the guidance development group in formulating their advice. Particular emphasis was placed on the potential seriousness of the outcomes for bleeding complications versus thromboembolic events.
The outcome was that for the NOACs, the SDCEP guidance takes a dual approach and advises that drug treatment is: (i) continued for more minor dental procedures, which are judged to have a low risk of bleeding complications; and (ii) briefly interrupted for more invasive and extensive dental surgery.
The opinion of the group was that the interruption of a patient’s NOAC medication was justified, but only for dental procedures with a higher risk of bleeding complications, and as long as the drug interruption was kept to a minimum.
The recommendation given in the guidance is to advise patients to miss (or delay, depending on the drug) their morning dose of NOAC on the day of treatment, giving a window of 12-24 hours (drug dependent) of drug interruption prior to their dental surgery. Because of the short-half lives of the NOACs (~12 hours), levels of anticoagulation fall quickly and can also be reinstated quickly, minimising the length of time that a patient is sub-therapeutically anticoagulated.
For the relatively low-risk dental procedures, it was judged that, taking the balance of likely risk of a severe bleeding complication versus a thromboembolic event and all other factors into account, these procedures can be carried out without drug interruption. However, as a precaution, the guidance advises that for these dental procedures, initial treatment should be limited so that the extent and controllability of bleeding can be assessed before proceeding further with the treatment.
Future research and recommendations
As with all guidelines, the recommendations for the new drugs will have to be reviewed in due course and revised if new evidence or experience emerges and indicates that this is appropriate.
It is very important that any adverse events occurring when providing dental treatment to patients taking the newer anticoagulant or antiplatelet drugs are recorded to inform future recommendations.
The national Yellow Card Scheme (www.yellowcard.mhra.gov.uk) collects data on adverse drug events, but this does, of course, rely on these being reported by practitioners and in sufficient detail. High-quality research studies are urgently required to investigate the impact of the drugs on bleeding complications after invasive dental procedures, and with longer patient follow-up, the effect on thrombotic events.
Another new oral anticoagulant, edoxaban, and an antiplatelet drug, vorapaxar, are now on the horizon, with both recently gaining EU marketing approval. Further drugs are also in the pipeline. Again, data on the impact of these for patients having dental treatment will be of great value to inform future guidelines for the management of such patients.
About the authors
Dr Michele West is a research and development manager with the Scottish Dental Clinical Effectiveness Programme (SDCEP) based in Dundee at the Dental Education Centre. She was the project lead for the development of SDCEP’s new dental clinical guidance for the ‘Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs’.
Garry Sime is a Specialist in Special Care Dentistry. He is currently working in NHS Tayside as the Senior Dental Officer for Outreach at Broxden Dental Centre in Perth. He was the chair of the guidance development group for the recently published SDCEP guidance document ‘Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs’.
To get in touch or for further information, email scottishdental.cep@nes.scot.nhs.uk
Please note
The information given in this article on the recommendations provided in the ‘Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs’ guidance is only a brief overview. For more detailed information about these recommendations and advice for following them, the dental practitioner should refer to the full guidance, which is available at www.sdcep.org.uk
References
1. Prescribing Information System, Information Services Division (ISD) Scotland, NHS National Services Scotland. (Extracted 25/08/2015)
2. Randall C. Surgical management of the primary care dental patient on warfarin: North West Medicines Information Centre. 2007; www.app.dundee.ac.uk/tuith/Static/info/warfarin.pdf.
3. Randall C. Surgical management of the primary care dental patient on antiplatelet medication: North West Medicines Information Centre. 2007; http://www.app.dundee.ac.uk/tuith/Static/info/antiplatelet.pdf.
4. Perry DJ, Noakes TJ, Helliwell PS, British Dental S. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br Dent J. 2007;203(7):389-393.
5. Aframian DJ, Lalla RV, Peterson DE. Management of dental patients taking common hemostasis-altering medications. Oral Surgery Oral Medicine Oral Pathology Oral Radiology & Endodontics. 2007;103 Suppl:S45.e41-11.
6. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
7. Armstrong MJ, Gronseth G, Anderson DC, et al. Summary of evidence-based guideline: periprocedural management of antithrombotic medications in patients with ischemic cerebrovascular disease: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80(22):2065-2069.
8. Barnes GD, Ageno W, Ansell J, Kaatz S, Subcommittee on the Control of Anticoagulation. Recommendation on the Nomenclature for Oral Anticoagulants: communication from the SSC of the ISTH. J Thromb Haemost. 2015;13:1154-6.
9. Scott A, Gibson J, Crighton A. The management of dental patients taking new generation oral anticoagulants. Primary Dental Journal. 2014;3(4):54-58.
10. Clarkson JE, Ramsay CR, Eccles MP, et al. The translation research in a dental setting (TRiaDS) programme protocol. Implementation Science : IS. 2010;5:57.
11. Wahl MJ, Pinto A, Kilham J, Lalla RV. Dental surgery in anticoagulated patients – stop the interruption. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(2):136-157.
12. Kämmerer PW, Frerich B, Liese J, Schiegnitz E, Al-Nawas B. Oral surgery during therapy with anticoagulants – a systematic review. Clin Oral Investig. 2015;19(2):171.
13. Devereaux PJ, Anderson DR, Gardner MJ, et al. Differences between perspectives of physicians and patients on anticoagulation in patients with atrial fibrillation: observational study. BMJ. 2001;323(7323):1218-1222.
14. Wahl MJ. Dental surgery and antiplatelet agents: bleed or die. The American Journal of Medicine. 2014;127(4):260-267.
15. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine. 2009;361(12):1139-1151.
16. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine. 2011;365(11):981-992.
17. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. The New England Journal of Medicine. 2011;365(10):883-891.
18. Warfarin 0.5mg Tablets: Summary of Product Characteristics. Amdipharm Mercury Company Limited; 2014. (www.medicines.org.uk/emc/medicine/25626)
Demand for dental implants is growing and patient acceptance of removable appliances is lower than in the past, as those who can afford to pay request restorations that are “fixed” in their jaws. Much of this demand, especially when multiple tooth replacement is considered, is from patients with a history of, or ongoing, periodontal problems.
This demand brings its own set of challenges, as many of the factors which put patients at risk of periodontitis and ongoing bone loss around teeth seem to apply to implants. What we are doing for many of these individuals is moving them from a state where periodontal disease has compromised tooth retention, one which they and their dentists have been unable to control, to a situation where they have complicated and expensive restorations, which need high degrees of skill to maintain, and which are susceptible to similar challenges in the medium and long term.
Our challenge as professionals advising and caring for these patients is to understand this and to plan and execute treatments to take their history into account. How can we reduce the likelihood that patients who had periodontitis, which caused them to lose their teeth prematurely, don’t suffer the same fate five, 10 or 15 years down the line after they have implants placed?
The aim of this article is to outline periodontal considerations when planning for successful restorations and working with this challenging group of patients.
Risk assessment
In long-term studies looking at implant retention, patients with periodontitis affecting their natural dentition were more at risk of developing problems in an implant restored one, whether or not they retained some natural teeth1,2. Current research seems to support the contention that implants will fare less well in patients with a history of aggressive periodontitis3,4. These problems become more pronounced with time1 and apply not principally in terms of absolute survival but in terms of problems which require intervention but may not result in implant loss, e.g. peri-implantitis. Key to success for patients with periodontal problems who are considering implants is assessing and then reducing this risk5.
Using historical evidence relating to periodontitis in an individual can be a valuable assessment tool in terms of potential ongoing risk. This is done by considering the history with regard to periodontal disease and the presence of additional risk factors6, which may contribute to implant-related problems.
For the purposes of this assessment, a thorough periodontal history and examination is required.
History
In the patient history the following factors may be indicative of higher risk:
- Smoking
- Systemic factors, particularly diabetes and stress
- Family history of early tooth loss that is related to periodontal disease
- History of tooth loss secondary to periodontal problems
- Poor outcomes of previous periodontal treatments.
Examination
In patients with complicated disease, as displayed by increased BPE scores, this examination will involve a full six-point pocket chart as well as an assessment of levels of oral hygiene and gingivitis. Radiographs should be assessed for the presence of periodontal bone loss (Fig 1).
Periodontal examination will highlight levels of periodontal attachment, the presence of areas of inflammation (as observed by bleeding on probing), areas of infection (suppuration on probing) and levels of tooth mobility. This thorough assessment enables the clinician and patient to understand the level of disease present, quantify risk of inflammatory breakdown and plan comprehensively for potential restorations at an early stage.
Donos et al7 categorised patients as low, medium and high risk for implant placement partially on the basis of these combined periodontal risk factors and clinical examinations:
High risk (Fig 2)
- Presence of aggressive or refractory periodontitis
- High plaque and bleeding on probing scores
- Smoking
- Systemic factors e.g. diabetes.
Medium risk (Fig 3)
- Previous periodontal disease overall successfully treated but still limited number of residual pockets >5mm and less than ideal oral hygiene.
Low risk (Fig 4)
- Systemically healthy
- Good response to periodontal therapy and displaying optimal oral hygiene
- Non-smoker.
Treatment modality selection
One of the fundamental questions when planning for this group of patients is the question of when to retain or extract teeth. The essential question is: will implants fare better, or even as well as, teeth in the medium and long term for the high-risk patient? A reasonable starting point may be that implants are a replacement for no teeth rather than a replacement for teeth.
Prior to removing teeth it is sensible to consider whether the patients’ own natural implants, their teeth, could be retained by a specialist rather than be extracted. Many long-term studies8,9 have shown that, following good-quality periodontal treatment and stabilisation of the periodontal tissues, it is possible to retain even severely compromised teeth for long periods of time.
This retention involves high degrees of skill and diligence by patients and support on a regular basis from a dental professional. However, this degree of required ongoing maintenance is not different with implants. Indeed, it is often much easier to maintain teeth than implant-supported restorations when one considers the morphology of restorations and the rough nature of many implant surfaces.
In high-risk patients, Donos et al.7 suggested that implants should not be provided and, instead, that maintenance of teeth should be a priority and restoration based on removable and conventional dental restorations supported on teeth rather than implants. This concept challenges opinion when one considers that many perceive removal of teeth and placement of implants as a good option for periodontally compromised teeth.
Of course, the decision to remove teeth is not purely periodontal, often due to compromised aesthetics following periodontitis, for example drifting of anterior teeth, or as a result of other restorative failure a decision is made to remove teeth. This is often, in fact, what patients request. Even in these cases the long-term consequences of removing teeth and rebuilding an aesthetic replacement, which will have to be retained and maintained, need to be carefully discussed with the patient. Loss of implants often leaves large tissue defects which can be extremely challenging to restore at a later date.
- Figure 1 – Radiographic presentation of aggressive periodontitis
- Figure 2 – Clinical features of aggressive periodontitis; high risk for implant restorations
- Figure 3 – Controlled chronic periodontitis and good maintenance; medium risk for implant restorations
- Figure 4 – Patient with external resorption of central incisor, no evidence of periodontitis, good OH and non smoker; low risk for implant restorations
Patient preparation
If the decision has been made to provide an implant-retained restoration for a patient with a history of periodontitis, it is vital that the patient is fully prepared for the procedure.
Patients should understand what will be required to maintain their restoration and prosthesis design should be discussed in terms of the ease of maintenance of a fixed versus removable, semi-fixed option. They should be given the opportunity to learn the skills needed to maintain their restoration prior to the uncomfortable post-surgical phase that challenges them in this respect. If patients are having a mixed restoration, i.e. retained teeth and implants, these skills can be acquired around natural teeth (Figs 5-10).
In this preparation phase we are essentially trying to accomplish several things:
- Turn a previously “bad” patient, one who has lost teeth secondary to disease, into a “good” one, where disease is controlled and burnt out and the patient’s risk is substantially reduced by their changed habits – i.e. good and regular OH, smoking cessation and attendance for regular and tight maintenance
- Establish conditions of periodontal health which reduce the risk to implants in the medium and longer term
- Allow the dentist some time to assess more fully what can and should be done to best restore the dentition. It may be possible to save teeth or a clearer picture may emerge as to what sort of restoration is best, if at all. Many patients function well on the shortened dental arch and the maintenance requirements are low.
Control of periodontitis
If patients have existing periodontitis, this should be controlled prior to implant placement. The aim is to reduce the risk of post-implant placement problems by reducing the likelihood of future periodontal problems. In practice, we should aim for:
- Probing pocket depths below 6mm
- High standard of oral hygiene
- Minimal BOP
- No pus on probing
- Smoking cessation
- Compliance with a regular supportive maintenance programme.
In a dentition where teeth are planned for retention, this will involve well-executed, non-surgical periodontal therapy10,11 but, in more severe cases, may mean that specialist periodontal treatment is needed during that first phase. In many cases specialist periodontal treatment can save teeth which may be deemed hopeless and the need for implants reduced8.
If that is the case then this should be accessed at an early stage to allow for healing of soft tissues and stabilisation of gingival margins prior to restoration. In patients who are to have all teeth extracted it is still worth investing time prior to extractions to control levels of inflammation and improve oral hygiene as a platform for future maintenance of implants12.
Every patient is, of course, an individual but in general terms early periodontal treatment and stabilisation involves:
- Discussion with the patient of aetiology of periodontitis, their risk profile and the effect that may have on implant restorations
- Extraction of teeth with a hopeless prognosis and arrangements for transitional restorations
- Liaison to control any systemic factors contributing to increased tissue breakdown
- Establishment of high levels of oral hygiene as monitored in the medium term, on an objective basis
- Support for smoking cessation
- Scaling to remove supragingival calculus and ease OH
- Sub gingival instrumentation to provide clean, bio-compatible root surfaces and allow the establishment of healthy periodontal support
- In some cases antibiotics may be required if the patient has a more aggressive form of disease
- Opportunity to further discuss with the patient ongoing maintenance requirements and establish habits of attendance for supportive treatment around implants.
If pockets are persistent after non-surgical treatment then principle options will be:
- Surgery for pocket reduction prior to implant placement
- Extraction of non-responding teeth and incorporation into the planned restoration
- Tooth retention and the postponing or cancelling of implant work either until the tissues have stabilised at a later stage or altogether if control is not possible.
Consolidation after this pre-surgical phase allows the clinician to understand better what the longer-term outcome for the patient is likely to be. Any restorations subsequently planned are therefore more predictable. Cancelling or delaying planned implant work is disappointing, however it may be the best option for some patients where periodontitis is not fully controlled. Conventional restorations are less expensive and are often easier to adjust and add to if teeth fail at a later date. This may be the case particularly for those who are have multiple high-risk indicators, e.g. smokers or those with poorly controlled diabetes.
Prosthesis planning
When planning the prosthesis for a patient who has had periodontitis in their natural dentition, the priorities should be to:
- Allow ease of access for good oral hygiene
- Ensure retrievability of restorations so that implant fixtures can be directly assessed and maintained on a regular basis.
The following factors should be considered:
- Removable or fixed
Retrievable restorations are a good option as they allow for maintenance of periodontal tissues by patients and professional staff. This ability to remove a prosthesis and examine tissues directly gives reassurance that implants can be comprehensively inspected and, if problems occur, they can be addressed swiftly.
In terms of how this may be managed, restorations can be removable by patients, as is the case with e.g. a locator-supported denture, allowing for daily plaque control, or screw-retained and removable by the clinician for maintenance, perhaps annually or biannually. Cemented restorations are often used to allow for correction of implant angulation and to avoid screw holes in positions which are aesthetically compromising.
This type of restoration, as well as running the risk of excess cement around the fixture head and “peri-cementitis”13, is extremely difficult to remove for routine maintenance without destroying the superstructure. Unless the patient can adequately access the peri-implant tissues, a cemented design will make maintenance extremely challenging.
- Figures 5-10 56-year old female presenting for implants. Long-standing severe periodontitis leading to multiple previous tooth loss. Staged approach to treatment tackling periodontal disease and extracting hopeless teeth at an early stage. Adhesive bridge placed in the lower anterior region. Once inflammation stabilised and probing pocket depth reduced, upper teeth extracted in stages and implants placed. Plan in place for an overdenture to allow for easy long-term maintenance of the upper arch
- Figures 5-10 56-year old female presenting for implants. Long-standing severe periodontitis leading to multiple previous tooth loss. Staged approach to treatment tackling periodontal disease and extracting hopeless teeth at an early stage. Adhesive bridge placed in the lower anterior region. Once inflammation stabilised and probing pocket depth reduced, upper teeth extracted in stages and implants placed. Plan in place for an overdenture to allow for easy long-term maintenance of the upper arch
- Figures 5-10 56-year old female presenting for implants. Long-standing severe periodontitis leading to multiple previous tooth loss. Staged approach to treatment tackling periodontal disease and extracting hopeless teeth at an early stage. Adhesive bridge placed in the lower anterior region. Once inflammation stabilised and probing pocket depth reduced, upper teeth extracted in stages and implants placed. Plan in place for an overdenture to allow for easy long-term maintenance of the upper arch
- Figures 5-10 56-year old female presenting for implants. Long-standing severe periodontitis leading to multiple previous tooth loss. Staged approach to treatment tackling periodontal disease and extracting hopeless teeth at an early stage. Adhesive bridge placed in the lower anterior region. Once inflammation stabilised and probing pocket depth reduced, upper teeth extracted in stages and implants placed. Plan in place for an overdenture to allow for easy long-term maintenance of the upper arch
- Figures 5-10 56-year old female presenting for implants. Long-standing severe periodontitis leading to multiple previous tooth loss. Staged approach to treatment tackling periodontal disease and extracting hopeless teeth at an early stage. Adhesive bridge placed in the lower anterior region. Once inflammation stabilised and probing pocket depth reduced, upper teeth extracted in stages and implants placed. Plan in place for an overdenture to allow for easy long-term maintenance of the upper arch
- Flange design
Restorations may incorporate deep or ridge lap flanges designed to close space, improve aesthetics and limit air and fluid escape. In these cases a pontic becomes very difficult to clean for the patient. In addition, the clinician will have no access to peri-implant tissues at maintenance visits to allow for visual inspection or to clean the area unless the superstructure is removed. If this sort of restoration is, in addition, cemented in a patient with a history of periodontitis the risk of disease developing is potentially high due to the problems it creates with oral hygiene and the difficulty of maintenance. Flange design should take into account the patient’s need to clean around the implants and beneath the pontic over the ridge and should allow for the use of interdental brushes or bridge floss in the area.
- Embrasure closure
Long and tight embrasures, designed to avoid black triangle spaces and fluid leakage, can make it extremely difficult to clean around implants when the spaces are too narrow to allow access for cleaning aids. This may be less of a problem if the patient is manually dexterous. However, if the patient is older and relying on help, for example if they are resident in a care home, the levels of oral care provided may be poor and implant health compromised.
Maintenance
Following delivery of the implant supported restoration it is essential that the patient is supported in their efforts of maintenance at home9,14,15,16. This applies whether there are remaining teeth or the dentition is implant-supported. At fitting of the prosthesis, all patients should have a good-quality periapical radiograph taken to establish baseline bone levels. If the patient has had periodontitis in the past then a comprehensive supportive care programme should be in place and can be modified to ensure adequate maintenance of the implants.
Once again plaque control was identified as a major risk for peri-implant mucosisitis in a recent systematic review17. As part of their completion review, patients should be given detailed instruction on exactly how to maintain their new restoration to avoid this. This will involve helping them to find the appropriate mechanical aids to access the peri-implant tissues and ensuring they can use them on a regular basis. At this stage, the benefits of the preparatory phase will become very apparent. Patients will already be used to and in the habit of cleaning to a high standard and have the knowledge of why that is necessary.
They may have personal experience of the benefit of periodontal treatment and support. Ideally, post-placement review should be a matter of modifying an existing good technique rather than attempting at that late juncture to introduce an entirely new one. All patients then need to understand the importance of supportive treatment either with a dentist or hygienist in ensuring long-term success of their restoration.
It is usual for patients to have an annual implant review appointment when radiographs are updated to monitor peri-implant bone levels and restorations checked. For those with retained natural teeth or with a history of periodontitis this is not likely to be adequate. A programme should be followed which will support their periodontal tissues, control inflammation and reduce risk of implant problems as well as monitoring the implants directly. For periodontitis evidence is plentiful that those following and compliant will have considerably increased chance of stability8,18.
Conclusion
In the current climate of using fixed implant-supported restorations to replace teeth, it is essential that patients are fully assessed prior to treatment. This is particularly important when considering the patient with a history of periodontitis who is at increased risk of peri-implant problems. If periodontitis is present it should be controlled prior to placement and the patient should be fully informed of their increased risk.
If periodontitis cannot be controlled then consideration should be given to a restoration not dependant on implants in a tooth/implant situation. Once placed, restorations need tight maintenance on a regular basis by both patient and dentist/hygienist. All those involved in planning and provision of implant treatment need to ensure they and their team have the skill to support their patients not only in the immediate surgical and restorative phases but in the longer-term life of the prosthesis.
About the author
Madeleine Murray, BDS, MSc, MPhil, FDS(Rest.Dent.) RCPS, MRD RCS Eng, qualified BDS from the University of Glasgow in 1984. She went on to train in the speciality of periodontics in London and then restorative dentistry in Glasgow and Manchester. Since the late 1980s, her principal clinical interest has been periodontology, especially the treatment of young individuals with aggressive periodontitis and, more recently, the management of patients with periodontitis who are having implant therapy. After specialist training, she taught on the Masters in Primary Dental Care in Glasgow and worked in specialist practice before moving with her family to Shanghai, China, for five years. She returned to Scotland in 2011 and is now based at the specialist clinic Vermilion in Edinburgh. She is an examiner for the specialist MRD in Periodontology at the Royal College of Surgeons in Edinburgh. She is married with two daughters.
References
1. Schou S1, Holmstrup P, Worthington HV, Esposito M Outcome of implant therapy in patients with previous tooth loss due to periodontitis. See comment in PubMed Commons below Clin Oral Implants Res. 2006; 17 Suppl 2: 104-23.
2. Ong CT, Ivanovski S, Needleman IG, et al. Systematic review of implant outcomes in treated periodontitis subjects. Journal of Clinical Periodontology. 2008; 35: 438-462.
3. De Boever A, Quirynen M, Courke W, Theuniers G, De Boever J. Clinical and radiographical study of implant treatment outcomes in periodontally susceptible and non-susceptible patients: a prospective long term study. Clin Oral Implants Res 2009; 20: 1341-1359
4. Mengel R, Behle M and Flores-de-Jacoby L. Osseointegrated implants in subjects treated for generalized aggressive periodontitis: 10 year results of a prospective, long term cohort study. J Periodontol 2007; 78: 2229-2237
5. Jepsen S, Berglundh T, Genco R, Aass A-M, Demirel K, Derks J, Figuero E, Giovannoli J-L, Goldstein M, Lambert F, Oritz-Vigon A, Polyzois I, Salvi G E, Schwarz F, Serino G, Tomasi C and Zitzmann N.U. Primary prevention of peri-implantitis: Managing peri-implant mucositis. Journal of Clinical Periodontology. 2015; 42(S16) S152-S157
6. Paulander J, Wennstrom JL, Axelsson P, Lindhe J. Some risk factors for periodontal bone loss in 50-year-old individuals. A 10-year cohort study. Journal of Clinical Periodontology. 2004; 31: 489-496.
7. Donos N, Laurell L and Mardas N. Hierarchical decisions on teeth vs implants in the periodontitis susceptible patient: the modern dilemma. Periodontol 2000 2012; 59: 89-110
8. Graetz C, Dörfer CE, Kahl M, Kocher T, Fawzy El-Sayed K, Wiebe JF, Gomer K, Rühling A. Retention of questionable and hopeless teeth in compliant patients treated for aggressive Periodontitis. Journal of Clinical Periodontology 2011; 38: 707-14
9. Axelsson P, Nystrom B and Lindhe J. The long term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. Journal of Clinical Periodontology 2004; 31: 749-57
10. Suvan JE. Effectiveness of mechanical nonsurgical pocket therapy. Periodontology 2000. 2005;37:48-71.
11. Eberhard J, Jervoe-Storm PM, Needleman I, Worthington H, Jepsen S. Full-mouth treatment concepts for chronic periodontitis: a systematic review. Journal of Clinical Periodontology. 2008; 35: 591-604.
12. Cortes AR, Cortes DN, No-Cortes J, Arita ES. Transition from failing dentition to full-arch fixed implant-supported prosthesis with a staged approach using removable partial dentures: a case series. J Prosthodont. 2014; 23: 328-32
13. Piñeyro A, Ganeles J. Custom abutments alone will not eliminate the clinical effects of poor cementation techniques around dental implants. Compend Contin Educ Dent. 2014; 35: 678-80, 682-6.
14. Carnevale G, Cairo F, Tonetti MS. Long-term effects of supportive therapy in periodontal patients treated with fibre retention osseous resective surgery. I: recurrence of pockets, bleeding on probing and tooth loss. Journal of Clinical Periodontology. 2007; 34: 334-341.
15. Tonetti MS, Muller-Campanile V, Lang NP. Changes in the prevalence of residual pockets and tooth loss in treated periodontal patients during a supportive maintenance care program. Journal of Clinical Periodontology. 1998; 25: 1008-1016.
16. Zangrando MS, Damante CA, Sant’Ana AC, Rubo de Rezende ML, Greghi SL, Chambrone L. Long-term evaluation of periodontal parameters and implant outcomes in periodontally compromised patients: a systematic review. J Periodontol. 2015; 86: 201-21.
17. Renvert S and Polyzois I. Risk factors for peri-implant mucositis: a systematic literature review. Journal of Clinical Periodontology. 2015; 42(S16): S172-S186
18. Tomasi C, Wennstrom J L and Berglundh T. Longevity of teeth and implants – a systematic review. J Oral Rehabil 2008; 35(Supplement): 23-32
Apical periodontitis has been established to be a microbial-induced disease 1–3. The aim of root canal treatment is the prevention or treatment of apical periodontitis by the elimination of micro-organisms from the root canal system and the prevention of subsequent recontamination 4. To this end, our primary treatment modality is chemo-mechanical debridement of the root canal 5.
Mechanical cleaning of the root canal system with hand or rotary instruments has been shown to engage only a proportion of the root canal wall – 35 to 53 per cent of the canal wall surface may remain untouched following preparation 6. Fins, lateral anatomy and communicating canals render the goal of mechanical removal of all infected tissue impossible; therefore, after gross debridement of the vital and non-vital tissue from the canal, the main goal of mechanical preparation is to enable chemical disinfection of the root canal 7.
The functions of endodontic irrigation include:
- Disinfection
- Degradation of pulp tissue
- Disruption of the biofilm
- Removal of the smear layer
- Lubrication of endodontic instruments
- Flushing of debris from the canal.
In practice, no single irrigant achieves all of these aims and a combination regime is recommended. Saline and local anaesthetic have each been employed, but these provide only a flushing and lubricating function. Irrigation with such chemically inert media has been shown to be incapable of adequately reducing the viable microorganisms in infected root canal systems 5.
Irrigants in contemporary use can be classified as antimicrobial or decalcifying 4 (see table).
| Antimicrobial Irrigants |
|---|
| Sodium hypochlorite |
| Chlorhexidine |
| Electro-chemically activated water |
| Iodine-potassium-iodide |
| Hydrogen peroxide |
| Decalcifying irrigants |
|---|
| Ethylenediaminetetraacetic acid (EDTA) |
| Citric acid |
Mechanical instrumentation has been shown to result in the burnishing of organic material and dentine debris against the canal wall and into depressions and lateral anatomy 8. The role of decalcifying agents such as EDTA incudes chelation of the mineral content of this “smear layer” and the opening of access to the lateral anatomy 9.
Sodium hypochlorite
Sodium hypochlorite (NaOCl) is recommended as the main endodontic irrigant due its ability to dissolve organic tissue and its broad anti-microbial spectrum 9. Its action on organic tissue enables it to disrupt and kill biofilms adherent to the root canal walls.
Concentrations in use in endodontics range from 0.5 to 5.25 per cent.
Chlorhexidine
Chlorhexidine is a bisguanide, generally used in the form of chlorhexidine digluconate. As a root canal irrigant, it is generally presented in 2 per cent concentration. While several in-vitro studies have shown anti-microbial efficacy to be similar to sodium hypochlorite, some in-vivo studies have demonstrated chlorhexidine to be inferior, with more culture reversals from negative to positive between visits. This is likely to be due to its inability to dissolve pulpal remnants 10.
The major advantages chlorhexidine has over sodium hypochlorite are lower toxicity, less objectionable smell and taste and substantivity, meaning it persists on the walls of the canals. Like sodium hypochlorite, chlorhexidine lacks the ability to dissolve the smear layer 4.
Chlorhexidine should not be used in conjunction with sodium hypochlorite due to the formation of a precipitate or flocculate. This flocculate contains para-chloroaniline (PCA), which is known to be carcinogenic, although the level of exposure in such cases is likely to be low. The presence of the flocculate may lead to blockage of narrow anatomy and subsequently hinder adequate penetration of hypochlorite.
Alternative concepts for antimicrobial irrigation include electrochemically-activated water (eg. Sterilox), laser photo activated disinfection and ozone gas filtration of the root canal system. Studies comparing the antimicrobial efficacy these approaches to irrigation, with a 3 per cent sodium hypochlorite solution found all to be inferior to varying degrees 11–13.
Decalcifying agents
Although sodium hypochlorite has the ability to dissolve organic tissue, it cannot dissolve the inorganic component of dentine. Decalcifying agents such as EDTA and citric acid are recommended for dissolution of dentinal debris and removal of the smear layer from canal walls. In addition, inorganic obstructions to negotiation of the root canal during preparation may be overcome with the aid ofchelation agents 9.
It is not recommended that EDTA be used as an alternating rinse with sodium hypochlorite due to the deactivation of sodium hypochlorite by EDTA 14. It is recommended that EDTA be used as a penultimate rinse. The canal is dried of sodium hypochlorite and the EDTA is introduced and left in the canal for one minute. This is then rinsed out and the canal dried again before the final rinse with sodium hypochlorite. In this way, the smear layer is removed, opening the dentinal tubules and any lateral canals to penetration with hypochlorite.
There is clinical folklore that mixing sodium hypochlorite in the canal with EDTA and creating an acid-base reaction, the so-called “Champagne Effect”, aids with coronal transportation of debris. No evidence exists to support this claim 9.
Factors that influence the effectiveness of irrigation:
- Concentration of the irrigant
- Temperature of the irrigant
- Level of corono-apical penetration of the irrigant
- Volume of irrigant exchange.
Concentration
The antimicrobial and tissue dissolution capacity of sodium hypochlorite are both a function of its concentration, but so is its toxicity. Spangberg found that a 0.5 per cent solution of sodium hypochlorite was sufficient to kill most micro-organisms, with the exception of Staphylococcus aureus, and retained the ability to dissolve necrotic tissue, though not vital tissue. One per cent solution killed Staphylococcus aureus 15 and 5.25 per cent sodium hypochlorite has been found to reduce the elastic modulus and flexural strength of human dentine, while 0.5 per cent solution does not 16.
The risk of apical extrusion of sodium hypochlorite also militates against the use of unnecessarily high concentrations, although a concentration of 0.01 per cent has been demonstrated to be lethal to fibroblasts and a case of skin injury with exposure to 2.5 per cent following rubber dam leakage is recorded 17.
Rapid dissolution of vital and necrotic tissue remnants within the pulp canal is an essential facet of the use of sodium hypochlorite irrigant. No other irrigant has been shown to dissolve pulpal remnants in the same manner. It is, therefore, necessary to balance the needs for a higher concentration of hypochlorite with the caveat that higher concentrations are more likely to result in tissue damage if accidentally extruded through the apex or exposed to the mucosa. A concentration of 2.5 per cent is commonly used. An alternative to increased concentration has been experimented with ex-vivo as described below.
Temperature
Heating the hypochlorite solution has been shown to increase both its bactericidal and tissue dissolving effects. The capacity of a 1 per cent solution of sodium hypochlorite at 45ºC to dissolve human pulp tissue was found to be equal to that of a solution of 5.25 per cent at 20ºC 18. No clinical studies have been carried out to determine the applicability of this technique in-vivo, however; the benefit of using heated, weaker solutions of hypochlorite is that a temperature equilibrium is quickly reached within the root and extrusion or mucosal exposure is less likely to cause serious injury.
Corono-apical penetration
Root canal irrigants are conventionally delivered using a side-vented needle, fitting loosely in the canal. Side venting and loose fit are important to reduce the risk of apical extrusion of irrigant and to increase the flushing effect on debris. Vapour lock (a body of gas trapped in the apical portion of the root canal) means that penetration of the irrigant under such passive irrigation circumstances has been shown to be no more than 1mm beyond the tip of the needle 19. In order to increase the efficacy of the irrigation, it is vital to:
- Maximise the extent to which the needle can penetrate
- Activate the irrigant in order to increase the penetration of the root canal.
The needle penetration is a function of both the size of the needle and the size of the apical preparation of the canal. Apical preparations in the order of ISO size 25-30 and the use of currently available 27-30 gauge needles will enable penetration to approximately 1mm from Working Length (Figure 1). This has been found by at least one study to be the most dominant factor in irrigant penetration 20.
The preparation taper has also been found to affect irrigant exchange, with apical preparations of greater taper producing greater flow of irrigant than narrow tapers 21.
Irrigant activation may be enabled either by manual or machine-assisted means. Manual techniques include agitation with the delivery needle, use of endodontic brushes or by manual dynamic irrigation. In this technique, a well-fitting gutta percha cone is placed into the irrigated canal and moved rapidly in and out with a 2-3mm stroke. This action is thought to create a hydrodynamic effect increasing the penetration and exchange of the reagent 20. A drawback of manual pumping is that it is laborious (Figure 2).
Machine-assisted agitation systems have come about to facilitate better penetration. Rotary brushes, such as Canalbrush, can be used in a handpiece but, again, only where the brush can penetrate.
Quantec-E provides continuous irrigation during rotary instrumentation. This concept should provide for greater irrigant exchange than needle irrigation alone and this has been shown to be true in the coronal third of canals; however, this has not resulted in cleaner canal walls in the middle and apical thirds of canals studied 22.
Sonic agitation devices, such as the Endoactivator from Dentsply, work at lower frequencies than ultrasonic devices and demonstrate higher amplitudes of displacement. Endoactivator utilises a smooth-sided polymer tip that has been demonstrated to be resistant to fracture and passive towards the dentinal walls of the canal (Figure 3).
Passive ultrasonic irrigation (PUI) has been demonstrated to be highly effective in increasing both the penetration and cleaning efficiency of irrigant solutions. Although PUI can be used with intermittent irrigation, it has been demonstrated to be most effective when applied to the completed canal preparation 9. The prepared canal is flooded with irrigant such as sodium hypochlorite. A file is then introduced to the maximum length at which it does not bind with the canal walls and activated with an ultrasonic unit. With the file tip free, a node of vibration is established, generating a wave of energy that streams irrigant coronally. Endosonore files are highly effective for this technique (Figure 4).
While passive irrigation with sodium hypochlorite does not remove the smear layer, when a 3 per cent solution of sodium hypochlorite is used with PUI, several studies have found complete removal of the smear layer 23–24. These findings were not reproduced when the irrigant was replaced with saline.
The precise mode of action of PUI is unclear, but acoustic streaming is thought to be the primary factor in debris removal. Cavitation has also been postulated as an effect. Cavitation occurs with the generation and collapse of microbubbles within the irrigant solution as the pressure drops momentarily below the liquid’s vapour point. This has been shown to generate high temperatures in the micro-environment and may explain the synergistic effect of PUI and sodium hypochlorite 25.
Pressure alternating devices
Devices have been introduced that create alternating negative pressure and positive irrigation within the canal. Examples include EndoVac and RinsEndo. A study of one of these systems (RinsEndo) found that it outperformed passive irrigation in the removal of a layer of stained
collagen from the canal walls but was inferior to manual dynamic irrigation 26.
Summary
Despite attempts to create alternative solutions and methods, the evidence supports a regime that involves:
- A solution of sodium hypochlorite with a concentration in the range 1 per cent to 3 per cent
- The use of a decalcifying agent to remove the smear layer
- Ultrasonic activation of the irrigant
- Adequate apical preparation and taper of the canal to permit placement of the irrigant within 1mm of the apex and enable sufficient irrigant flow.
Figure 5 shows two completed cases demonstrating accessory anatomy that is not accessible to files, but which has been cleaned by irrigant penetration.
- Figure 1 – Top: A 27G cutaway irrigation needle. Bottom: A 30G side-ported needle. Middle: A Protaper F2 rotary file for comparison
- Figure 2 – A well-fitting GP cone can be used in a rapid pumping motion for manual dynamic irrigation
- Figure 3 – The Endo Activator from Dentsply
- Figure 4 – An endosonic file in its adaptor
- Figure 5 – Two teeth with accessory anatomy that has been cleaned by the reagent regime, not filing
About the author
Adrian Stewart BDS, PG Dip Endo (UCL), MSc, graduated from Queen’s University, Belfast in 1992. He holds an MSc in Clinical Dentistry (restorative dentistry) from Leeds University and the Post Graduate Diploma in Endodontic Practice from the Eastman Institute, UCL. Adrian works in practice limited to endodontics, taking referrals for non-surgical and surgical endodontics at 1 Manor Place, Edinburgh.
References
- Kakehashi S, Stanley HR, Fitzgerald RJ. The Effects of Surgical Exposures of Dental Pulps in Germ-Free and Conventional Laboratory Rats. Oral Surg Oral Med Oral Pathol. 1965 Sep;20:340-9.#
- Moller AJ, Fabricius L, Dahlen G, Ohman AE, Heyden G. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res. [Research Support, Non-U.S. Gov’t]. 1981 Dec;89(6):475-84.
- Nair PN. Apical periodontitis: a dynamic encounter between root canal infection and host response. Periodontol 2000. [Review]. 1997 Feb;13:121-48.
- Excellence Cf. Root canal irrigants and disinfectants. Endodontics [serial on the Internet]. 2011; Winter.
- Bystrom A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res. 1981 Aug;89(4):321-8.
- Gulabivala KP, B.; Evans, G.; Ng, Y-L. Effects of mechanical and chemical procedures on root canal surfaces. Endodontic Topics. 2005;10:103-22.
- Hulsman MP, O.A.; Dummer, P.M.H. Mechanical preparation of root canals: shaping goals, techniques and means. Endodontic Topics. 2005;10:30-76.
- Hulsmann M, Rummelin C, Schafers F. Root canal cleanliness after preparation with different endodontic handpieces and hand instruments: a comparative SEM investigation. J Endod. [Comparative Study]. 1997 May;23(5):301-6.
- Zehnder M. Root canal irrigants. J Endod. [Review]. 2006 May;32(5):389-98.
- Ringel AM, Patterson SS, Newton CW, Miller CH, Mulhern JM. In vivo evaluation of chlorhexidine gluconate solution and sodium hypochlorite solution as root canal irrigants. J Endod. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S.]. 1982 May;8(5):200-4.
- Seal GJ, Ng YL, Spratt D, Bhatti M, Gulabivala K. An in-vitro comparison of the bactericidal efficacy of lethal photosensitization or sodium hyphochlorite irrigation on Streptococcus intermedius biofilms in root canals. Int Endod J. [Comparative Study]. 2002 Mar;35(3):268-74.
- Gulabivala K, Stock CJ, Lewsey JD, Ghori S, Ng YL, Spratt DA. Effectiveness of electrochemically activated water as an irrigant in an infected tooth model. Int Endod J. [Comparative Study]. 2004 Sep;37(9):624-31.
- Hems RS, Gulabivala K, Ng YL, Ready D, Spratt DA. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. [Comparative Study Evaluation Studies Research Support, Non-U.S. Gov’t]. 2005 Jan;38(1):22-9.
- Rossi-Fedele G, Dogramaci EJ, Guastalli AR, Steier L, de Figueiredo JA. Antagonistic interactions between sodium hypochlorite, chlorhexidine, EDTA, and citric acid. J Endod. 2012 Apr;38(4):426-31.
- Spangberg L, Engstrom B, Langeland K. Biologic effects of dental materials. 3. Toxicity and antimicrobial effect of endodontic antiseptics in vitro. Oral Surg Oral Med Oral Pathol. [Comparative Study In Vitro]. 1973 Dec;36(6):856-71.
- Sim TP, Knowles JC, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. [Clinical Trial Comparative Study Randomized Controlled Trial]. 2001 Mar;34(2):120-32.
- Serper A, Ozbek M, Calt S. Accidental sodium hypochlorite-induced skin injury during endodontic treatment. J Endod. [Case Reports]. 2004 Mar;30(3):180-1.
- Sirtes G, Waltimo T, Schaetzle M, Zehnder M. The effects of temperature on sodium hypochlorite short-term stability, pulp dissolution capacity, and antimicrobial efficacy. J Endod. [Evaluation Studies]. 2005 Sep;31(9):669-71.
- Ram Z. Effectiveness of root canal irrigation. Oral Surg Oral Med Oral Pathol. 1977 Aug;44(2):306-12.
- Bronnec F, Bouillaguet S, Machtou P. Ex vivo assessment of irrigant penetration and renewal during the final irrigation regimen. Int Endod J. 2010 Aug;43(8):663-72.
- Boutsioukis C, Gogos C, Verhaagen B, Versluis M, Kastrinakis E, Van der Sluis LW. The effect of root canal taper on the irrigant flow: evaluation using an unsteady Computational Fluid Dynamics model. Int Endod J. [Comparative Study Research Support, Non-U.S. Gov’t]. 2010 Oct;43(10):909-16.
- Setlock J, Fayad MI, BeGole E, Bruzick M. Evaluation of canal cleanliness and smear layer removal after the use of the Quantec-E irrigation system and syringe: a comparative scanning electron microscope study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. [Clinical Trial Comparative Study Randomized Controlled Trial]. 2003 Nov;96(5):614-7.
- Cameron JA. The use of ultrasound for the removal of the smear layer. The effect of sodium hypochlorite concentration; SEM study. Aust Dent J. [Research Support, Non-U.S. Gov’t]. 1988 Jun;33(3):193-200.
- Alacam T. Scanning electron microscope study comparing the efficacy of endodontic irrigating systems. Int Endod J. [Comparative Study]. 1987 Nov;20(6):287-94.
- van der Sluis LW, Versluis M, Wu MK, Wesselink PR. Passive ultrasonic irrigation of the root canal: a review of the literature. Int Endod J. [Review]. 2007 Jun;40(6):415-26.
- McGill S, Gulabivala K, Mordan N, Ng YL. The efficacy of dynamic irrigation using a commercially available system (RinsEndo) determined by removal of a collagen ‘bio-molecular film’ from an ex vivo model. Int Endod J. 2008 Jul;41(7):602-8.
I feel your pain
The risk of anti-fungal resistance in dentistry: lessons from a Japanese fungus
Globally since 2009, Candida auris, a fungal species closely related to Candida albicans, has been responsible for a number of… Read more
The anxious patient: Empathy, planning and a team-approach
[ Words: Ilyaas Rehman, BDS (Glas) ] Introduction Introduction This case report documents the treatment provided for a very anxious… Read more
Meaningful milestone
Consultation represents the next step on the journey towards achieving a more effective system of CPD Some dental professionals feel… Read more
Top tips for practicing evidence-based dentistry: Part 3
Introduction Implementing the best available evidence and enabling positive sustainable change in practice is an enviable goal for anyone providing… Read more
The management of a paediatric dental avulsion in general dental practice
Abstract A paediatric dental avulsion is not a clinical scenario that you will be faced with on a daily basis… Read more
Intraoral scanners In dentistry – an update on digital technology
With the introduction of the first intraoral scanner, CEREC (Chairside Economical Restoration of Esthetic Ceramics) by Dentsply Sirona in 1985,… Read more
CBCT and clinical decision-making
Arvind Sharma, BDS(Dund), MSc(Endo), MJDFRCS(Eng), MFDSRCPS(Glas) Arvind Sharma presents the second and final part of a structured critical review to… Read more
Problems of a phobic patient
Day One Ms B attends as a new patient at a local dental surgery complaining of sensitivity in a number… Read more
The power of regeneration
Due to its powerful regenerative properties, platelet rich growth factor Endoret (PRGF) is being increasingly used in many fields of… Read more
Suitability of patients for conscious sedation
Patients suitable to undergo conscious sedation (CS) include those with moderate-severe anxiety, a swallow/gag reflex or a mild learning/physical disability… Read more
Top tips for practicing evidence-based dentistry
In the first article, we explored how to establish a research question using the PICO (Population, Intervention, Comparator and Outcome) method… Read more
Quick, aesthetic restoration
A new patient in her early 30s attended for a check-up. A routine radiograph revealed caries under the amalgam filling… Read more