There are four main domains where the workings of the mind have had an influence on our daily practice. These are: the dentist-patient relationship, dental anxiety, chronic oral facial pain and the stress of dental practice. In this article, I will address the first two domains and suggest ideas as to how both patients and the dental team would be better served by a more holistic body mind paradigm. In the next issue, I will discuss the final two influences. The duality of mind and body, first advocated in the 17th century by René Descartes, is finally beginning to find a home in Western medicine.
The influence of the mind on the development and progress of disease, both physical and psychological, is receiving the research attention that it merits. Descartes postulated that there was a real distinction between the immaterial mind and the material body. Although mind and body are ontologically distinct substances, they causally interact.
Psychology is defined in the Oxford dictionary as the scientific study of the human mind and its functions, especially those affecting behaviour. The etymology of the word is from modern Latin meaning the study of the soul. The history of psychology dates back to the Ancient Greeks who regarded it as a philosophy rather than a science. It was not until the late 1800s that it developed into a scientific subject.
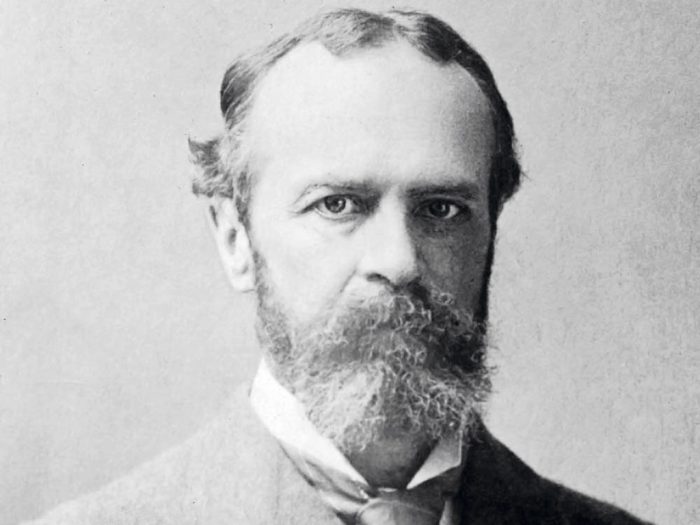
The first psychology lab was at the University of Leipzig where Wilhelm Wundt studied reaction times. The father of American psychology was William James who wrote The Principles of Psychology and was interested in conscious human experience. The dichotomy of thought in psychology made its appearance in Austria around the same period, with the work of Sigmund Freud on the unconscious. His psychoanalytic theory arose from work with hysterical patients were he proposed the unquiet mind derived from unresolved childhood conflicts.
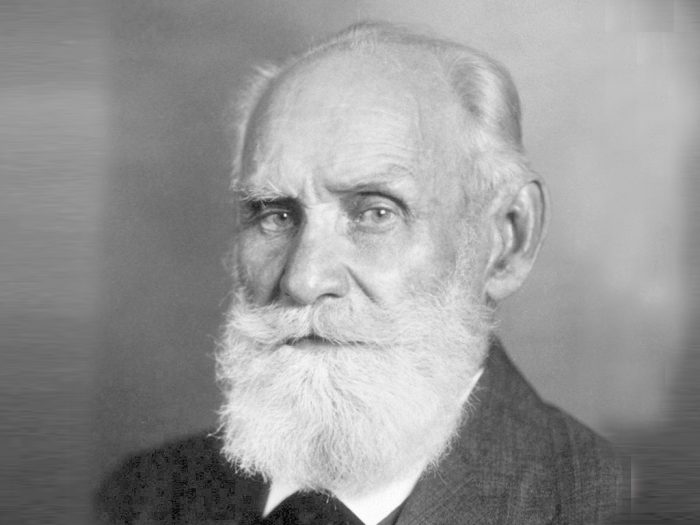
The work of the Russian psychologist Ivan Pavlov heralded in the age of behaviourism, his most famous experiment being Pavlov’s dogs showing classical conditioning. This was soon followed by Skinner and operant conditioning looking at behaviour in terms of actions and consequences. Carl Rogers’ theory gave birth to the third force in psychology known as humanistic psychology. It emerged as a paradigm to counteract the limitations of behaviourism and psychoanalysis.
Psychologists such as Rogers and Maslow were interested in the meaning and purpose of human behaviours. They were fascinated as to what conditions fostered the growth of the human person to self-actualise within the constraints of their own environment. The term cognitive psychology was first used by Ulric Neisser in 1967 and is a branch of psychology which is goal orientated and problem focused. The three main therapies arising from this way of thinking are:
- Albert Ellis’s rational emotive behaviour therapy (REBT)
- Aaron Beck’s cognitive therapy (CT)
- Donald Meichenbaum’s cognitive behaviour therapy (CBT)
The main principles under lying these therapies were first voiced by William James at the beginning of the 20th century: “Thoughts become perception, perception becomes reality. Alter your thoughts, alter your reality.”
Today, psychology is very much rooted in neuroscience and neurobiology. The advent of magnetic resonance imaging has provided a non-invasive way of examining the human brain. The amygdala, hippocampus, and medial prefrontal cortex have been shown to be involved in the stress response and in PTSD. Research in this domain is bringing understanding as to how therapies like eye movement desensitisation and reprocessing (EMDR) and brainspotting might work.
This brief introduction serves to demonstrate the plethora of knowledge that seeks to understand the human mind and human behaviour. The richness of psychological knowledge permeates into every area of society yet the primacy of this way of thinking is sometimes overlooked in the reductionist materialistic way that we teach our medical and
dental students.
Dentist-patient relationship
The work of Mills et al (2015) attempts to classify the main indicators of a good patient experience. In the UK, the NHS Patient Experience Framework highlights the Picker Principles of Patient-Centred Care as the optimum way to provide care. This form of care embraces much more than the daughter test as it invites us to see the other through the lens of compassion.
Patient-centred patient care has evolved from the philosophy of the humanistic psychologist Carl Rogers. Rogers believed that the patient is the expert in their own lives and, if given the opportunity, will self-actualise within their own environment. He used the metaphor of a potato in a darkened room sending out shoots towards a crack of light. If a patient is treated with empathy, unconditional positive regard and congruence within the dental domain then the framework for a positive patient experience is put in place.
This is fine rhetoric but words have no value unless they can be put into action. The following narrative, although not based in the dental surgery, involved a patient who sadly was in the end stages of oral cancer. His name has been altered to protect his identity. Many years ago, I had recourse to visit this man – let’s call him Bob – in hospital, he was dying from the ravaging effects of oral cancer. He was being fed through a peg tube and his breathing eased by a tracheostomy. This gentleman had been a rough sleeper for most of his life and had enjoyed solace from a homeless centre where I worked. On visiting him in his hospital room I brought him shower gel and soap to which he promptly replied: “What the hell are you bringing me these for? I need Guinness and fags!”
On exiting the room I put this request to the nursing sister; she looked at the patient and then myself and said to bring him some Guinness and some fags. On my next visit, I watched Bob syringe the Guinness into his peg tube and smoke his cigarette through his tracheostomy.
That nurse had treated Bob as a human being, she had given him dignity and respect. This man had lived on the streets where alcohol and cigarettes, for whatever reason, had been his only consolation. At this end stage of his life the nurse had looked on him with empathy and unconditional positive regard and bestowed upon him the dignity of being permitted to die with the tools that had enabled him to live. She, within the limits of her environment, had not allowed rigid protocols to undermine the humanity of the other.
Empathy and unconditional positive regard in the dental surgery invites us to treat others as we would like to be treated ourselves. It does not judge or stereotype our patients but treats each individual as unique. In this uniqueness, the encounters with our patients hold the potential of enriching both our lives and the life of the other. In my experience, kindness is the medium through which empathy is conveyed to the patient. Unconditional positive regard is the prising of the other for no other reason than they are our fellow travellers on this earthly sojourn. To hold the other in a positive light is to convey to them that they matter, they are not simply another extraction or a bridge to be fitted. They too have a place in society and their wellbeing is of prime importance to us.
The research of Sherman at the University of Washington Dental school shows that there is a decrease in clinical empathy over the four-year training course. This mirrors the work done by Chen (2012) on medical undergraduates. Research demonstrates that students who have a high level of empathy are more competent at history taking, have a higher physician and patient satisfaction, decreased malpractice litigation and are significantly better at motivating patients.
The importance of empathy in health care was emphasised in the Francis Report after the systemic failings at the Mid Staffordshire Foundation Trust. The GDC in their Preparing for Practice document highlight the importance of communication and professionalism in the training of undergraduates. Much research is needed in defining clinical empathy and discovering how best it may be taught.
Dental anxiety
The 2009 Adult Dental Health Survey, commissioned by the NHS Information Centre, revealed that 36 per cent of adults had moderate dental anxiety and 12 per cent were classified as being dentally phobic managing their anxiety by avoidance of all things dental. The impact of dental anxiety can have far-reaching consequences on a patients health and wellbeing, both psychologically and physically. Yet the literature reveals that there are no specific guidelines on the diagnosis or treatment of dental anxiety.
The work of Professor Tim Newton of King’s College London Dental Institute, Health Psychology Service and Art De Jongh of the Netherlands go along way to address this. Both authors offer a framework in which to classify dental anxiety and suggest different treatment modalities dependent of the level of anxiety. They propose that mild dental anxiety can and should be treated in the dental surgery by the dental team.
Research reveals that good interpersonal skills and empathy can of themselves decrease dental fear. Good communication enables the establishment of trust and a framework in which to carry out treatment. Precise information regarding the exact nature of treatment is essential to allay fears as is the establishing of a sense of control by adopting a stop signal. The “tell, show, do” technique has been about for more than 50 years and can be used for the simplest to the most complex treatment. There is also a place for the consideration of premedication and the use of nitrous oxide. The use of coping strategies such as distraction through visual or auditory stimuli and relaxation techniques all have part to play in mild dental anxiety management.
Hypnosis was first used in 1841 by the English physician James Braid and has been used in dentistry for well over half a century. It is a non-pharmacological method of inducing a trance-like state. In this state of altered consciousness, the patient is able to focus all of their attention on an image, thought or feeling and in so doing take their attention away from their feelings of anxiety. This method can also be very helpful in treating an overactive gag reflex, which is often found in dentally anxious patients. In order to aid the dental team in their treatment of patients with mild to moderate anxiety the website dentalfearcentral.org is an excellent resource for both staff and patients.
Patients who present with a moderate to severe level of dental anxiety should, in many cases, be referred to a secondary centre for the treatment of their dental anxiety. This secondary centre could be managed by a psychologist or a dentist with psychotherapy training (generic training or CBT training). The reason for this referral would be to assess the level of dental anxiety and also determine if there are any co-morbid psychological conditions.
In research done at Kings by Kani et al (2012), 37 per cent of the patients who had dental phobia were also shown to have high levels of generalised anxiety, 12 per cent had clinically significant depression and 12 per cent were shown to have suicide ideation. A referral centre that would enable assessment of dentally anxious patients would compliment a sedation service and offer patients definitive tailored treatment to address their dental anxiety.
A study done by Woolley in 2009 showed that individuals who are referred for sedation are highly anxious and fear a range of different dental stimuli. Yet previous research demonstrated that referring dentists to a sedation clinic did not consider psychological management for their patients. Sedation has, and always will have, a part to play in the management of dental anxiety but the only way to address the underlying issues is to complement the service with psychological interventions.
The study conducted by Kani et al (2012) showed that, of the 130 dentally phobic patients referred to the King’s College London Dental Institute, 79 per cent went on to have dental treatment without sedation. These patients were treated by CBT. This therapy has proven efficacy for the management of anxiety and depression. CBT is a synthesis of behaviour therapy and cognitive therapy which uses behaviour modification techniques and cognitive restructuring. It is a short-term therapy involving five to 10 sessions, usually of one hour duration. It is a collaborative enterprise and usually involves the patient doing homework.
Unlike many other psychotherapy treatments, it is a here and now therapy as what started a problem in the past is not often what keeps it going at the present time. The behaviour modification techniques involve such things as breathing exercises and in certain cases systematic desensitisation. The cognitive therapy involves identifying and challenging negative thoughts through the use of socratic questioning and the testing of hypothesis. The success of CBT is such that, in 2009, the Department of Health (England) recommended this therapy in conjunction with sedation services as a model of excellence in the management of dental fear.
The comprehensive assessment of patients allows different psychological interventions to be considered in the treatment of patients. The work of Art De Jongh has shown that were patients have a specific memory of dental trauma, EMDR may offer complete resolution of their dental phobia. EMDR stands for eye movement desensitisation and reprocessing and has been used extensively in people suffering from post traumatic stress disorder. The traumatic nature of memory formation in these individuals means that the memory of the trauma is unprocessed and the person is plagued by intrusive thoughts and flashbacks. By a process of bilateral stimulation either visual or auditory, the memory is accessed and desensitised of its affective content and negative cognitions. The memory is then accessed again and reprocessed with much less affect and a positive cognition. I have found this to be very successful in two or three visits where a phobia follows on from a specific dental trauma even when that trauma occurred many years previously.
Dental hypnosis has been revisited in the treatment of patients with moderate to severe dental anxiety. A study by Halsband et al (2015) has demonstrated that even brief dental hypnosis sessions can have an influence on the fear processing structures of the brain. Twelve dental phobic patients and 12 healthy control patients were tested by a 3T MRI whole body scanner observing brain activity changes after brief hypnosis. In the dental phobic group, dental fear was represented in the brain by increased activity in the left amygdala and bilaterally in the anterior cingulate cortex (ACC), insula and hippocampus (R<L).
- Mary Downie
- Tim Newton
- William James (Portrait 1890)
- Ivan Pavlov
- René Descartes
Amazingly, during hypnosis the scan revealed significantly reduced activity in these areas. In the healthy group of patients, no amygdala activity was observed. This study demonstrates objectively what hypnotherapists have been subjectively experiencing with their dentally phobic patients. In these times of great uncertainty, the wisdom of past ages is reemerging to show us a way forward without our heavy reliance on drugs.
The currency on which most psychological treatments thrive is time, unfortunately this is in short supply in busy NHS practices. In order to give dentally anxious patients the treatment that offers possible resolution of their condition, this paper proposes that psychological services must work in collaboration with dentistry.
This article has attempted to demonstrate that psychology can and does have an influence on the way we treat and manage our patients. The next article seeks to show how the treatment of chronic oral facial pain and the stress encountered in dental practice can be positively influenced by looking outward from the biomedical model. The wisdom of great scholars has been revisited as we seek to offer both our patients and the dental team a more balanced and productive way of practising.
References
Adult Dental Health Survey 2009, NHS Digital.
Chen DC, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school.
Med Teach. 2012;34(4):305-11. doi: 10.3109/0142159X.2012.644600.
DeJongh A, Adair P, Meijerink-Anderson M. Clinical Management of Dental Anxiety: What works for whom? International Dental Journal (2005) 55, 73-80
De Jongh. A, Van Den Oord. H, Ten Broeke, E. Efficacy of Eye Movement Desensitization and Reprocessing in the Treatment of Specific Phobias: Four Single-Case Studies on Dental Phobia Journal of Clinical Psychology, Vol. 58(12), 1489–1503 (2002)
GDC Publications Preparing for Practice.
Halsband, Ulrike; Wolf, Thomas Gerhard; NLM Functional changes in brain activity after hypnosis in patients with dental phobia Journal of physiology, Paris109.4-6 (Dec 2015): 131-142.
Kani E, Asimakopoulou K, Daly B, Hare B, Lewis J, Scambler S, Scott S, and Newton JT. Characteristics of patients attending for cognitive behavioural therapy at one UK specialist unit for dental phobia and outcomes of treatment. British Dental Journal Volume 219 No. 10 Nov 27 2015
Mills I, Frost J, Kay E, and Moles DR. Person-centred care in dentistry – the patients’ perspective. British Dental Journal 218, 407 – 413 (2015) Published online: 10 April 2015 | doi:10.1038/sj.bdj.2015.248
Newton T, Asimakopoulou K, Daly B, Scambler S, and Scott S. The management of dental anxiety: time for a sense of proportion? British Dental Journal 2012; 213: 271-2 74
Sherman J and Cramer A. Measurement of Changes in Empathy During Dental School. Journal of Dental Education Vol 69 Number 3
Woolley SM, Summary of: Who is referred for sedation for dentistry and why? Published online: 28 March 2009 | doi:10.1038/sj.bdj.2009.233
About the author
Mary graduated from Glasgow University in 1980 and from the Open University in 2001. She obtained a postgraduate diploma in counselling and psychotherapy from Stirling University in 2013. She has enjoyed a plethora of experiences in dentistry both in the UK and abroad.She especially enjoyed her post in Glasgow University teaching oral surgery. Mary is now in full-time psychotherapy practice but would like to combine psychotherapy and dentistry if the right post became available.
A 49-year-old male patient attended for an emergency appointment due to experiencing pain and swelling from a lower left tooth/teeth. He was experiencing pain with biting and pressure. Patient had been experiencing pain from the lower left quadrant for the past few days and the tooth area had now become swollen. He reported no sleep loss or pain with temperatures reported. The quality of pain reported as a dull throbbing pain.
Patient was able to identify tooth LL4 as the source of pain. Analgesics (paracetamol and ibuprofen) had been taken.
Patient had RCT on tooth LL4 while on holiday in Las Vegas, Nevada, US, in 2003. Emergency treatment had been provided by a GDP and definitive RCT completed. A temporary restoration had been placed. On return to Scotland, a composite onlay had been provided as a definitive coronal restoration since the patient reported no pain and was reassured by the Las Vegas dentist that treatment had been completed. The radiograph copy provided by the patient showed a completed root canal treatment on tooth LL4 with all visible canals obturated. Tooth LL4 had been symptom-free until now.
Previous dental history
The patient is registered with NHS Scotland. He is a regular attender, attending six-monthly examinations and hygienist appointments. He is well-motivated about his dental health.
Previous medical history
No relevant medical history noted. No medication taken. Patient was a smoker (20 per day) up until March 2011.
Social history
Married. Telephone engineer. Non-smoker and moderate alcohol intake.
Examination
Extra-oral
Examination revealed some submandibular swelling on the left mandible. No other significant findings noted.
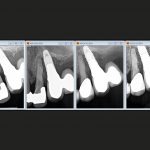
Intra-oral (Fig 1a-c)
- Soft tissues – Some gingival swelling was palpable buccal to tooth LL4. Oral mucosa, tongue, sublingual tissue and soft/hard palate appeared within normal limits. LL4 was also tender to percussion and appeared to have a small degree of mobility. No lingual swelling was noted.
- Periodontal condition – A Basic Periodontal Examination was recorded as per Table 1.
- Occlusal examination – Angles class I anterior relationship; Class I molar relationship on the left and
a Class I canine relationship on the right. Left and right lateral excursions were canine guided.
Protrusive guidance was provided by palatal surfaces of the maxillary incisors. - Dentition – The dentition present are recorded in Table 2.
The dentition was heavily restored posteriorly on the left and with 1 occlusal restoration present on the right. Upper anterior incisors had porcelain bonded crowns in situ. - Specific examination of the problem site (LL4) – Tooth LL4 was restored with a composite onlay in situ. This was fitted in 2009 and had a good marginal seal and good occlusal relationship with the maxillary teeth. Intercuspal relationship was noted and the buccal cusp was involved in left lateral excursions. There were no isolated periodontal probing defects, no signs of coronal or root fracture and the tooth was TTP.
| 2 1 4 |
| 4 3 3 |
| 7 4 3 2 1 1 2 3 4 5 6 7 |
|---|
| 7 4 3 2 1 1 2 3 4 5 6 7 |
Special investigations
Special investigations were carried out in order to form a provisional and ultimately a definitive diagnosis and to enable the formulation of a definitive treatment plan. The tests performed with results are provided in Table 3 above. The contralateral tooth was used as a control.
Special investigations
| Special test | LL3 | LR4 |
|---|---|---|
| Digital axial/horizontal pressure | Yes | No |
| TTP-axial/horizontal | Axial | No |
| Digital palpation-buccal/lingual | Buccal/lingual | No |
| Endo-Frost | No | Yes |
| EPT | No | Yes |
| Periodontal probing | Within normal limits | Within normal limits |
Radiographic examination
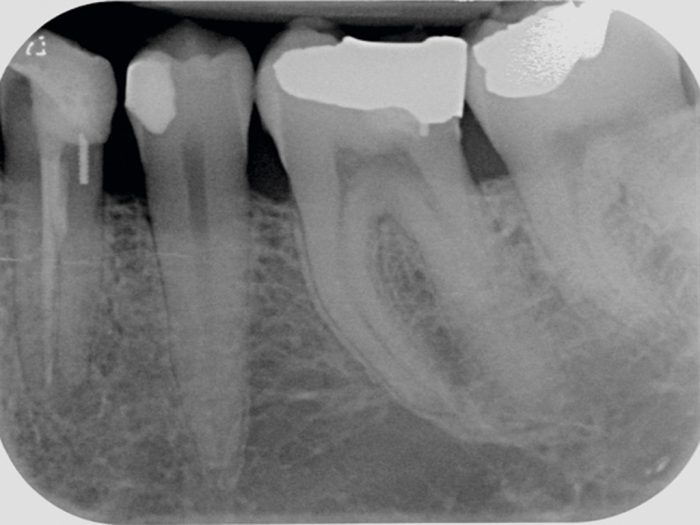
A periapical radiograph (Fig 2) taken at the emergency appointment, revealed a marginally sound coronal restoration. A dentine pin appeared to be present in the distal of the tooth. Some horizontal bone loss was evident at the distal of the tooth. A radio-opaque material was present in the root canal which appeared sub-optimal (non-homogenous obturation) and possibly short of the radiographic apex.
The root appeared wide and a ledge/step was visible mid root with the obturating material. This seemed to suggest two root canals being present with only one obturated. A feint canal root canal space is evident in the distal root. A periapical radiolucency was apparent with some widening of the periodontal ligament space.
The other teeth visible in the radiograph appeared to be clinically sound.
Provisional diagnosis
- Periodontal abscess associated with LL4
- Dental cyst associated with LL4
- Failed primary root canal treatment (apical periodontitis).
Definitive diagnosis
Moderate, non-suppurative, localised, chronic apical periodontitis with a non-obturated root canal. A failed primary root canal treatment. This diagnosis was reached after careful consideration of the clinical signs and symptoms, the special test results and the radiographic information.
Since the special test results showed digital axial/horizontal pressure with axial TTP and tenderness to buccal-lingual pressure, inflammation of the periapical tissues or apical periodontitis, was diagnosed. A dental cyst was considered and it was decided that if definitive treatment was unsuccessful then further tests would be performed to investigate possible cyst formation with associated treatment.
The patient was advised that the reason for treatment was due to bacteria being present in the un-instrumented root canal and quite possibly in the obturated canal also since the obturation appeared suboptimal. Bacterial cause of apical pathology has been shown by Kakehashi et al. 1965 and residual micro-organisms in the root canal system and cementum has been shown by Dalton et al. 1998 and Molander et al. 1999.
Strictly speaking, a definitive diagnosis is only truly possible with a histological analysis of the infected area (Nair et al. 1990 and 1999). However, the resources or facilities for this were not possible.
- Figures 1 a-c: Inra-oral clinical photographs
- Figures 1 a-c: Inra-oral clinical photographs
- Figures 1 a-c: Inra-oral clinical photographs
- Figure 2: LL4 pre-op radiograph
Treatment options
- Reduction of the infection and keep tooth LL4 under observation;
- Reduction of the infection and root canal retreatment of tooth LL4;
- Extraction of tooth LL4 with assessment for prosthetic replacement in 6 months.
Treatment plan
Since the patient was well motivated and wished for a predictable long-term solution he opted for reduction of the infection with root canal retreatment under private contract. He did not wish to keep the tooth under observation since there was a risk of his symptoms returning and he did not wish for extraction of tooth LL4, as this would have functional and aesthetic implications for him.
The treatment procedures with risks were discussed at length. The patient was advised that treatment success would be achieved by removing all of the previous obturation materials, locating the additional canal(s), chemically and mechanically disinfecting the canals and finally obturating the canals and providing a definitive coronal seal.
The patient was given the opportunity to ask questions and these were answered to the patient’s satisfaction. The patient was given a good prognosis upon successful completion of treatment with a success rate approximated at 62-86 per cent based of evidence published by Sjogren et al 1990. The patient was advised that non-surgical root canal retreatment was indicated as a primary treatment option as indicated by Rahbaran et al 2001. Consent was taken and two subsequent appointments made.
Treatment schedule
- Antibiotic prescription to reduce facial swelling
- Oral hygiene advice and instruction plus interdental cleaning demonstration
- Scale and polish
- Restorability assessment and root canal re-treatment of tooth LL4 over two visits
- Definitive composite restoration of access cavity
- Review (one year).
Items 2 and 3 were performed by the practice dental hygienist.
The second part of this article will look at the treatment and case discussion.
References
Dalton BC, Rstavik D, Phillips C, Pettiette M and Trope M, 1998. Bacterial reduction with nickel-titanium rotary instrumentation. Journal of endodontics, 24(11), pp. 763-767.
Kakehashi S, Stanley HR and Fitzgerald RJ, 1965. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surgery, Oral Medicine, Oral Pathology, 20(3), pp. 340-349.
Molander A, Reit C and Dahln G, 1999. The antimicrobial effect of calcium hydroxide in root canals pretreated with 5% iodine potassium iodide. Dental Traumatology, 15(5), pp. 205-209.
Nair PR, Sjgren U, Figdor D and Sundqvist G, 1999. Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 87(5), pp. 617-627.
Nair PR, Sjgren U, Krey G, Kahnberg K and Sundqvist G, 1990. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. Journal of endodontics, 16(12), pp. 580-588.
During the natural ageing process, the production of our own collagen is reduced and the elasticity of our skin degrades. There is an increasing popularity within our population today of people seeking non-invasive alternatives to skin tightening procedures to help combat the first signs of aging.
As mentioned in our previous article (SDM Nov/Dec 2016), Forma (InMode Inc, Richmond Hill, ON, Canada, North America) is a FDA-approved bipolar, non-invasive radio frequency (RF) device that generates controlled dermal heating.
Forma is based on ACE (Acquired Control Extend) technology which is comprised of the following steps:
- Acquire – Forma has a temperature sensor built into the handpiece which reads skin surface temperature 1,000 times per second, allowing clinicians to acquire skin temperature in real time.
- Control – Software algorithm allows unprecedented safety of RF delivery. The ‘cut off temperature’ feature reduces RF energy automatically when the handpiece senses that the required skin temperature has been reached.
- Extend – Clinical evidence suggests prolonged exposure to temperature above 40º C is advantageous for optimal clinical outcomes. Only InMode’s ACE technology allows you to utilise therapeutic temperatures safely and efficiently 1
Non-invasive skin tightening represents a rapidly emerging area in cosmetics, as patients increasingly seek to avoid facelifts and other invasive procedures. Non-ablative heating of the dermis and subcutaneous tissue offers the potential for skin tightening and rhytid reduction with minimal pain, downtime, and low risk of scars or other adverse events 2.
Forma is a non-invasive treatment that can be used to target fine lines, wrinkles and loose/lax skin. This treatment will stimulate new collagen formation within the skin which in turn will improve elasticity and give skin a firmer, rejuvenated appearance.
This RF device offers several advantages over currently available technologies, which likely explains this high level of clinical efficacy. The Forma device utilises real-time temperature-monitoring mechanisms, assessed by measuring tissue impedance, temperature, and epidermal contact throughout the treatment. This allows the device to continuously monitor the targeted tissue, and adjust the delivery of the RF energy to create a uniform heating exposure. The device is also able to maintain this constant uniform heating exposure for prolonged periods over relatively large treatment areas, such as an entire unilateral cheek. This uniform, long exposure is likely more effective at inducing collagen remodelling and neocollagenesis. Additionally, since the thermal exposure can be extended and prolonged, lower temperatures that do not induce any pain can be utilised 2.
The main goal for this case study is to provide further information on alternative non-invasive procedures and to demonstrate the results that can be achieved from ACE technology.
Case study
- Fig 1: first appointment
- Fig 2: first appointment
- Fig 3: first appointment
- Fig 4: final treatment
- Fig 5: final treatment
- Fig 6: Before and after comparison
- Fig 7: Before and after comparison
- Fig 8: Comparison photo
A 58-year-old female patient with skin type II, concerned about the appearance of her lower face (jowls and nasolabial folds) and neck area.
During the initial consultation the main areas of concern for the patient were established. Information was then given to the patient on the Forma treatment – how the treatment works, advised treatment schedule and the benefits. Throughout this discussion, the patient was able to ask any questions they had on the treatment.
Contraindications of the treatment were then discussed. Contraindications include – pacemaker or internal defibrillator, permanent implant in the treatment area, cosmetic fillers in the last six months, botox within the last week, a history of skin cancer or pregnancy/nursing mothers.
After all of the relevant information was given to patient and any questions answered, the patient was then able to make an informed decision as to whether she would like to proceed with the case study. Pre–treatment photos were then taken (Figs 1-3). It is essential to take pre-treatment photographs as this will provide you with a reference point throughout the entire treatment.
Treatment
The proposed treatment schedule for our patient to be able to obtain the optimum results was eight sessions of Forma at weekly intervals. Each session would last one hour and would involve treating both sides of the lower face and neck. Throughout the entire process, the patient’s face was divided into three treatment zones – right side of face, left side of face and neck. These three areas were then further divided into treatment areas which were roughly 10x10cm in size.
Each sub-divided treatment area was concentrated on individually for 10 minutes giving a total treatment time of 60 minutes. The patient’s tolerance to the treatment was very good, so the working parameters were set to the maximum recommendations from the machine’s manufacturer:
- RF = 62 for lower face (jowls and around mouth)
Temp = 43 - RF = 50 for neck, Temp = 43.
The radio frequency was reduced when treating the neck area as the skin in this area tends to be thinner and patients tend to find this area more sensitive to treat. Once the set working temperature was achieved, each area was then treated for 10 minutes. The length of time it takes to achieve the required working temperature varies depending on various external factors such as temperature of room, surface temperature of patient’s skin, etc.
After every treatment, the machine was appropriately cleaned down using 70 per cent alcohol as recommended by the manufacturer. It is essential that the appropriate safety checks are always carried out by the operator prior to use.
Feedback was obtained from our patient throughout the treatment process. She reported that she found the treatment very relaxing and could feel and see the difference in her skin after the first few treatments.
At the end of the treatment process – post-treatment photos were taken (Figs 4 and 5) and compared to original photos taken at the initial consultation (Figs 6, 7 and 8).
My experience working with the InMode Machine
As a fully qualified dental nurse, providing treatments that offer a non-invasive alternative to skin tightening is a relatively new field for me. I am aware of the increasing popularity within our population today of people seeking a wide range of facial aesthetic procedures. The InMode machine is an excellent piece of equipment to work with; it offers the clinician operating it a great deal of reassurance and confidence when providing a treatment due to all the built in safety mechanisms.
For example – monitoring the skin’s surface temperature 1,000 times per second throughout the Forma procedure. The machine is very well ergonomically designed which allows the operator to provide treatments with ease. The only minor difficulty I have occasionally experienced when providing a Forma facial is the position of the cable that attaches the handpiece to the machine. When treating a patient’s neck area, the cable can occasionally sit against their shoulder due to the working angle. However, if this is explained to the patient at the time they are always very understanding.
Results
There was a noticeable improvement in the appearance of fine lines with the skin looking rejuvenated from the treatment. The overall results from this course of treatment were excellent with the biggest change seen on the neck area – the loose/lax skin on the neck now appears much firmer than in the pre-treatment photos.
At the end of the treatment process, our patient was extremely happy with the results she achieved. After a discussion with the patient it was agreed that we had achieved a moderate result after the eight sessions of Forma. There were no adverse reactions experienced throughout this course of treatment.
The results achieved in this case were comparable to the results from a study carried out in America in 2015 3. This study was carried out treating fifteen patients with an average age of 62. They reported: “Results: All patients (14/14) were determined to have a clinical improvement, as the pre-treatment and post-treatment photographs were correctly identified by the evaluators. It was observed that 21 per cent (3/14) of patients had significant improvement, 50 per cent (7/14) had moderate improvement, and 29 per cent (4/14) had mild improvement. No pain, side-effects, or adverse events were observed.”
Feedback from all of our patients is vitally important to us. Throughout every stage of the Forma treatment and we regularly monitor how the patient is finding the treatment and if they have noticed a change in the appearance/texture of their skin. It is also important to find out how the patient is coping with the treatment, if there is anything we could do or change to improve their experience of the Forma facial.
It is also important to manage an individual’s expectations from the initial consultation throughout the treatment to the final appointment. Due to the fact Forma is a non-invasive and non-surgical procedure, it is impossible to achieve the dramatic changes you see with any invasive procedures. Patients and treatment providers will be able to see clinical improvements in their skin, however this is achieved gradually throughout the process, hence the importance of pre and post-treatment photographs.
Unrealistic expectations can leave patients feeling disappointed and disheartened with the treatment they had. If a patient is looking for a drastic change in areas of loose/lax skin and are not opposed to invasive procedures, it may be a better option for them to seek information for a suitably qualified professional on the other treatments available to them prior to proceeding with a course of Forma.
References
- inmodemd.com
- Nelson A, Beynet D and Lask GP. Non-invasive facial aesthetics. Scottish Dental magazine, Nov/Dec 2016: 52-54.
- Nelson A, Beynet D, Lask GP. A novel non-invasive radiofrequency dermal heating device for skin tightening of the face and neck. J Cosmet Laser Ther. Vol. 17, Iss. 6, 2015.
About the author
Megan Brown is a dental nurse/face and body cosmetic therapist at the Scottish Centre for Excellence in Dentistry in Glasgow.
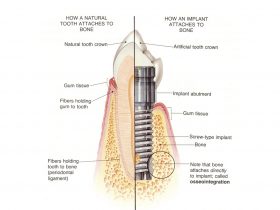
In the last issue we reviewed the literature on the validity of the use of periodontal indices to predict peri-implantitis. The conclusions were that current diagnostic tools are ineffective at predicting peri-implant problems, and, moreover, if they are used as an indicator of treatment needs, many patients will receive treatment that is of no benefit1.
To recap:
- The majority of implants will bleed on probing
- Pocket depth of >4mm cannot be used as a sign of pathology
- Increasing pocket depth alone is not an accurate predictor of peri-implant bone loss
- A single episode of bone loss is not an indicator of future bone loss and does not call for treatment, unless associated with other signs of active infection (bleeding and profuse suppuration on palpation)
- Peri-implantitis cannot occur within a year of implant placement as this is the adaptive phase of integration
- Radiographic evaluation of crestal bone levels over time seems to be the most reliable tool to identify those implants undergoing continuous bone loss and therefore in need of treatment.
The above points are uncomfortable as they may challenge what we have previously been taught in the clinical management of dental implants.
The following obvious questions arise:
- Just when should we intervene?
- Which patients really are at risk?
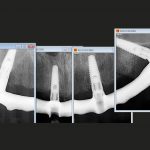
The bottom line, unfortunately, is that we don’t know (Figs 1 and 2). With hindsight it is, of course, easy to look at a failing implant case and postulate as to the probable causes of failure playing the, so called, “blame game”.
Likely suspects
- The patient – poor oral hygiene smoker, diabetic, previous periodontitis, bruxist, aggressive foreign body reaction
- The surgeon – surgical trauma, implant selection, positioning, technique
- The restoring dentist – occlusion, misfit, material/component choice, poor treatment planning.
While all the above factors have, at one time or another, been highlighted in crestal bone loss and failure, in reality what is more likely is, as described by Albrektsson,
a combination of a number of these factors2.
In terms of prevention of peri-implant problems, the “ideal” would be that ALL clinicians involved are experienced and knowledgeable in ALL aspects of dental implant treatment and planning, and are respectful not only of the others’ role but of their own limitations.
For example, while restoring a single tooth implant may appear simple from a technique perspective, the restorative dentist taking on this treatment has as much a role in the long-term survival of the implant as the surgeon. A poorly constructed crown can result in implant failure3.
A multidisciplinary approach can be argued to be the most effective as not only should all potential compromising factors be managed to a higher level, but responsibility is shared. It is essential, however, that such an approach is openly collaborative with the restorative dentist or prosthodontist taking the lead, as it is they that are ultimately responsible for the long-term management and care of the patient.
- Poor oral hygiene
- Crestal bone stability over seven years
- Profuse suppuration
- A single radiograph cannot diagnose peri-implantitis
- Bone loss radiographic series after maturation phase 2008-9
- Progressive bone loss after maturation phase surgical debridement was carried out in 2009 bone loss continued
- Despite visible threading and poor oral hygiene this is not perimplantitis without progressive bone loss
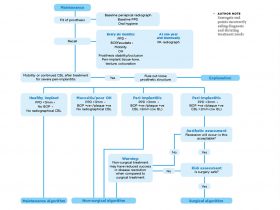
Proposed guidelines for follow-up of implants
In current practice, clinicians are challenged to provide a high level of care often within the constraints of a system which does not recognise the time/effort and expense required in providing it.
What is needed are simple diagnostic tools which can be integrated into routine daily practice, taking a minimum of time and providing a high degree of accuracy. Current implant maintenance advice does the opposite of this. Bleeding on probing and pocket charts take time and, as we now see, have a very low level of predictive accuracy.
Based on the current degree of knowledge, the most reasonable approach is that implant patients should be examined annually for the presence of clinical problems. The clinical examination should cover three areas:
Observation – absence of redness and swelling in the soft tissues, assessment of adequate plaque control4 and assessment of the occlusal scheme (paying particular attention to the possibility of parafunction and the excessive loads this may transfer to the restorations and implants)
Palpation – pressure on the tissues surrounding the implant to ensure absence of discomfort, bleeding and suppuration (see Fig 3)
Radiation – radiographs should be taken once a year during the first two to three years of function and thereafter at regular intervals (every two or three years, depending on the findings of the clinical examination and on the individual patient’s oral hygiene and co-operation) to monitor the crestal bone level stability.
It should be kept in mind that a stand alone radiograph after baseline radiography is insufficient to diagnose “disease” (Fig 4). To diagnose peri-implant health or disease, a series of radiographs from different times of follow up is needed to decide whether a particular implant has progressive loss of marginal bone (Figs 5a and 5b). Furthermore the “series” of radiographs only starts after the maturation/ adaptive phase of one year5.
Only significant, progressive loss of marginal bone, as verified in the series of radiographs, in association with clinical signs of inflammation such as redness, swelling, bleeding and suppuration at palpation and pressure on the soft tissues (not at probing) should be considered indicative of an ongoing peri-implantitis process (Fig 5c).
- FIGURE 6 – Radiographic series showing progresssive bone loss around three out of four implants
- FIGURE 7 – Clinical picture at completion of treatment
- FIGURE 8 – Surgical debridement of granulation tissue to attempt to treat suppurative infection
- FIGURE 9 – Clinical picture after healing
- FIGURE 10 – At presentation
- FIGURE 11 – Radiographic series showing stability of bone despite significant loss round implant and adjacent tooth
- FIGURE – 12 Remaining teeth and ailing implant removed and replaced for fullarch restoration
- FIGURE 13 – New baseline radiograph
- FIGURE 14 – Implant removal tool in failed implant
- FIGURE 15 – Failed implant counter rotated out to break osseointegration
Clinical aspects of true peri-implantitis lesions
True peri-implantitis lesions do of course exist, all be it in a thankfully smaller number that some might think, with an incidence of only 2.7 per cent 5. Peri-implantitis constitutes a threat to the longevity of the implant due to rapid marginal bone loss. Characteristic symptoms are, as outlined above: swelling, redness, pain and suppuration when palpating the peri-implant soft tissues in addition to the presence of rapid marginal bone loss.
The pathology of the development of a peri-implantitis lesion is not well understood. A primary peri-implantitis lesion has yet to be recognised and treatment is usually of the secondary infection which presents clinically. It is postulated that marginal bone resorption, for any reason, may have provided the conditions for a secondary infection with anaerobic bacteria, which in turn accelerates the tissue damage 2,6.
Treatment therefore should be aimed at resolving the presenting infection. This can include the use of local antibacterial rinsing, general treatment with antibiotics and surgical exploration of the area (Figs 6, 7, 8, 9).
There are, in addition, a number of innovative approaches to the surgical management of peri-implantitis lesions proposed:
- Laser treatment of cleaned implant surface
- “Implantoplasty” to attempt smoothing of the implant surface
- Use of antibiotics mixed with biomaterials to promote healing and soft tissue reattachment to the implant
- Soaking of the implant with various solutions after mechanical cleaning.
- While all these techniques show occasional impressive results to justify their use, it should be remembered, in the context of this and the previous article, that:
The diagnostic tools dictating treatment are poor and may have resulted in treatment of implants that did not actually have true peri-implantitis lesions, in which case there is little to be learned
In such cases there are no controls or long-term outcomes – these are low evidence techniques and do not justify routine practice
Surgical treatment of peri-implantitis is unpredictable whatever the method7.
As stated before, the pathology of a true peri-implantitis lesion is poorly understood. Even if the secondary infection is managed effectively, the cause of the original bone loss may still be present and continue to affect marginal bone levels. It is important, therefore, that all the potential compromising factors are also addressed (patient/surgeon/restorative).
Occasionally, bone loss results in the exposure of a large portion of the implant, deeming it unaesthetic, impossible to clean and a constant irritation for the patient. In such situations, if it has not already lost integration, removal of the implant should be considered. Implant failure is no longer a terminal event, in contrast to losing a tooth, as a new implant can be placed if a sufficient amount of bone is present. The replacement implant does not seem to be significantly worse off than any new implant might be.
Osseointegrated implants can now be removed in an atraumatic way by using a so-called removal tool. With this new development, removal of “ailing” implants can be carried out and treatment started anew, rather than lengthy, unpredictable surgical “management” (Figs 10-15).
Conclusions
There is still a lot that we do not know about peri-implantitis and hopefully future research will provide us with accurate diagnostic indicators of health and treatment needs, together with predictable management techniques. Until such a time, we need to approach peri-implant problems with a measured and pragmatic approach, assessing each case on its clinical presentation and deciding on a course of action that is best for that patient at that time.
References
1. Coli P, Christiaensen V, Sennerby L, De Bruyn H. Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontology 2000 Vol 73, 2017, 203-217.
2. Qian J, Wennerberg A, Albrektsson T. Reasons for Marginal Bone loss around Oral Implants. Clin Implant Dent Relat res 2012:14: 792-807.
3. Bryant SR. Oral implant outcomes predicted by age and site specific aspects of bone condition. PhD Thesis Department of Prosthodontics, University of Toronto, Canada 2001.
4. Attard N. Zarb G. Long term treatment outcomes in edentulous patients with implant-fixed prostheses: the Toronto study. Int. Journal Pros 2004:17:4.
5. Albrektsson T, Buser D, Sennerby L. Crestalbone loss and oral implants. ClinImplant Dent Relat Res 2012: 14: 783–791.
Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? ClinImplant Dent Relat Res 2014: 16: 155–165.
Listl S. Tu Y. Assessment of endpoints in studies on peri-implantitis treatment – A systematic review. Journal of Dentistry 2010: 38: 443-450.
About the authors
Dr Kevin Lochhead is a specialist in prosthodontics and principal dentist at Edinburgh Dental Specialists. He qualified from Kings College London in 1987.
Dr Pierluigi Coli is a specialist in periodontics and prosthodontics at Edinburgh Dental Specialists. He graduated with honours in dentistry at the University of Genova, Italy in 1990. He was trained in periodontology, dental implantology and prosthodontics in the prestigious Departments of Periodontology, of Oral Rehabilitation/Branemark Clinic and of Prosthetic Dentistry/Oral Material Sciences, Faculty of Odontology, University of Gothenburg, Sweden, where he specialised
and worked during the years 1993-2007.
Professor Lars Sennerby is a visiting professor in implantology at Edinburgh Dental Specialists. He graduated from the Faculty of Dentistry, University of Gothenburg, Sweden in 1986. He joined the research group led by Prof P-I Branemark in 1982 and participated in studies on osseointegrated dental implants. In 1991 he was awarded a PhD for his thesis entitled “On the bone tissue response to titanium implants”. He was trained in oral surgery at the Branemark Clinic, Public Health Service and Faculty of Dentistry in Gothenburg and worked there part-time from 1989 to 2001.
Impacted lower third molars are a common developmental anomaly in primary care that requires an evidence-based approach to gain informed consent from patients in treatment planning. The prophylactic removal of third molars has been discouraged since the development of SIGN 43 and NICE guidelines.
The SIGN guidance suggests “surgical procedures for extraction of unerupted third molar teeth are associated with significant morbidity including pain and swelling, together with the possibility of temporary or permanent nerve damage, resulting in altered sensation of lip or tongue” 1.
The introduction of SIGN guidance initially showed a reduction in the number of cases of third molar removal in primary care. However, since 2005 there has been a steady upward trend 2. McCardle and Renton suggest this initial change resulted in patients retaining third molar teeth due to rigid interpretation of the guidance. The extraction of third molars may have been delayed due to the use of antibiotics to manage pericoronitis or a more palliative approach to clinical decision-making. As patients retain third molars into later life they are more vulnerable to caries and pathology, particularly where the teeth are impacted leading to the ‘rebound’ in data.
Inferior alveolar nerve injury is a significant complication associated with the removal of third molars and is reported to occur in up to 3.6 per cent of cases permanently and 8 per cent of cases permanently 3. Such injuries can significantly impact a patient’s quality of life and should be taken into consideration when making clinical decisions and gaining informed consent. The coronectomy technique is an alternative procedure to complete removal of a third molar in high-risk cases and can reduce the risks of nerve damage.
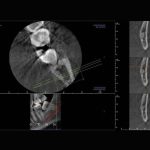
- FIGURE 1 – Example of low-risk case where tooth 48 is mesially impacted but not closely associated with the inferior dental canal. Note the presence of distal caries on tooth 47
- FIGURE 2 – Example of a moderate-risk case of horizontal impactions of 38 and 48
- FIGURE 3 – Example of a high-risk case where both 38 and 48 are closely associated with the inferior dental canal
- FIGURE 4 – CBCT imaging demonstrating a close relationship between the IAN and a mesially impacted 38
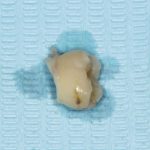
- FIGURE 5 – Roots remaining in situ after removal of crown
- FIGURE 6 – Crown sectioned below the ACJ and removed
- FIGURE 7 – Left OPT demonstrating post-op view of retained roots in situ
Assessment of lower third molars
A methodical approach to the gathering of relevant information from the clinical history is key to successful management. The guidance provided by SDCEP document ‘Oral Health Assessment and Review’ provides a comprehensive overview to history taking 4.
The patient’s history should be combined with a thorough clinical and radiographic examination. Practitioners are advised to follow IRMER 2000 5 in ensuring any exposure is justified, optimised and dose limited. Colleagues are also referred to FGDP’s ‘Selection Criteria for Dental Radiography’ 6 for guidance in their decision making process.
The guidance indicates that radiographs are indicated in the “extraction of teeth or roots that are impacted, buried or likely to have a close relationship to important anatomical structures. With the exception of third molars, the appropriate radiograph will normally be a periapical view”. As a result, an OPT is generally the radiograph of choice for assessment.
All images should be reported on by the practitioner and particular attention paid to the following radiographic signs that could result in a higher risk of inferior alveolar nerve damage as described by Palma-Carrió et al 7:
- Darkening of the root
- Deflection of the root
- Narrowing of the root
- Bifid root apex
- Diversion of the canal
- Narrowing of the canal
- Interruption in white line of canal.
Colleagues are advised to make an assessment of the difficulty of the case and their own surgical skills before considering the options of surgery in primary care, referral to a dentist with a special interest in oral surgery or referral to secondary care. Some radiographic examples are shown in Figs 1-3.
CBCT
In high-risk cases, the European Commission Cone Beam CT for Dental and Maxillofacial Radiology 8 guidance states: “Where conventional radiographs suggest a direct inter-relationship between a mandibular third molar and the mandibular canal, and where a decision to perform surgical removal has been made, CBCT may be indicated.”
Matzen et al carried out a study of 186 lower third molars that were assessed using both panoramic imaging and CBCT to decide whether surgical removal or coronectomy was indicated 9. Treatment planning was carried out after the initial two-dimensional imaging followed by a second treatment plan after three-dimensional imaging. The authors found that the treatment plan was changed for 22 teeth and thus CBCT influenced the decision making process in 12 per cent of cases. The authors advised that “narrowing of the canal lumen and canals positioned in a bending groove or in the root complex observed in CBCT images were a significant factor for deciding on coronectomy”.
The example in Figure 4 demonstrates a case of a mesially impacted tooth 38 that required CBCT investigation as part of the examination and consent process. CBCT demonstrated a close relationship between the roots of 38 and the IDN. In this case, the patient was offered the opportunity of both surgical removal and coronectomy. Given the potential for altered sensation or numbness, the patient opted to undergo a coronectomy.
Given the significant impact of CBCT imaging in treatment planning it is essential that patients in high-risk cases are offered three dimensional imaging and coronectomy where appropriate in order to gain informed consent.
Evaluation of findings and consent
On reviewing the findings of both clinical and radiographic assessment, clinicians should refer to the guidance available in the UK in deciding whether surgery is indicated 1,10,11:
- One or more episodes of pericoronitis
- Caries in the third molar or lower second molar. The future risk of caries in the second molar should be taken into account
- Pulpal/periapical pathology
- Periodontal disease
- Internal/external resorption of the tooth or adjacent teeth
- Follicle disease including dentigerous cysts
- Prophylactic removal in specific medical conditions such as before chemotherapy/radiotherapy
- To facilitate effective restorative treatment including prosthesis
- Patients whose lifestyle precludes ready access to
dental care.
This list is not exhaustive and practitioners are advised to make an individualised risk assessment and assist patients in making informed decisions in relation to their ongoing care.
Consent
Informed consent is an essential part of the assessment process and it is advisable to obtain written consent.
Patients should be alerted to the following risks:
- Pain and discomfort
- Swelling and trismus
- Bleeding
- Infection
- Localised alveolar osteitis or infection (around 20 per cent of cases)2
- OAF/OAC in the case of upper third molars
- Paraesthesia or anaesthesia of the inferior alveolar nerve or lingual nerve in lower third molars (8 per cent temporarily and up to 3.6 per cent of cases permanently) 3.
In high-risk cases, patients should be offered the opportunity of a coronectomy procedure where appropriate. Patients should be aware of the possible need for a second surgical procedure at a later date and the possibility that, should the roots become mobile, the need for complete extraction 12.
Patients should be given adequate time to consider the risks involved and an opportunity to have their queries answered, this may involve a second visit to allow sufficient time.
Procedure
The coronectomy technique or “deliberate vital root retention” is a means of removing the crown of the tooth but leaving roots intimately related to the inferior alveolar nerve untouched in order to reduce the risk of nerve damage. The procedure is carried out as follows 13:
IDB and long buccal infiltration anaesthesia are provided. The author’s preference is lidocaine 2 per cent, 1:80000 adrenaline, as an IDB and articaine 4 per cent, 1:100000 adrenaline, given as a buccal infiltration.
A full thickness mucoperiosteal flap is raised to obtain sufficient access and expose the third molar tooth.
A fissure bur is used to remove buccal bone and expose the crown of the tooth down to the ACJ. The fissure bur is used to drill into the pulp at the mid centre of the buccal grove as it intersects with the ACJ. This cut is lateralised to create space for an elevator. The cut should be no more than the length of the bur in order to avoid perforation of the lingual cortical plate.
An elevator, such as a Coupland’s or straight Warwick James, is used to fracture the crown from the roots. It is essential to take care and not apply too much pressure at this stage to prevent mobilisation of the roots. If mobilisation occurs, the roots must be elevated and removed.
A rosehead bur can then be used to remove any spurs of enamel and to reduce the roots a few millimeters below the alveolar bone crest.
The pulp chamber is left untouched and primary closure with resorbable sutures.
Contraindications
- Contraindications to coronectomy include:
- Teeth with active infection
- Mobile teeth
- Deep horizontal impactions as sectioning of the crown could in itself endanger the nerve 14.
Complications
Complications after coronectomy are rare but include
the following:
- Pain
- Infection
- Alveolar osteitis
Failed coronectomy i.e. mobilisation of the roots (9-38 per cent) - Inferior alveolar nerve injury
- Root migration (30 per cent) 14.
Post-operative pain is an expected complication but the more conservative nature of the coronectomy procedure results in less tissue disturbance and thus less post-operative pain than conventional surgical removal. Simple analgesia such as paracetamol and NSAIDs is adequate for post-operative pain relief in most patients 15.
The incidence of alveolar osteitis is 10 to 12 per cent. Should ‘dry socket’ occur, the management is similar to that in extractions of irrigation and placement of a dressing. Rates of infection after coronectomy range from 0.98 to 5.2 per cent. Local measures with antibiotics as an adjunct can be used to manage. If the retained root fragment is involved it may need to be retrieved, however, this is rare 15.
O’Riordan demonstrated in a study of 100 patients that the risk of infection was minimal and morbidity less after coronectomy than after surgical removal. Over the subsequent two years some roots migrated coronally and were removed under LA 16. Given the reduced risks of nerve injury, it has been recommended for patients where there is a high risk of nerve injury.
Root migration is estimated to occur in between 14 per cent and 81 per cent of cases. Pogrel estimates root migration of approximately 30 per cent over a six-month period 18. Similar results were found by Knutsson et al on a prospective trial of 33 patients where, after one year, all but six roots had migrated between 1 and 4mm 19. Migration can continue to the point where eruption into the oral cavity occurs. If this occurs, the roots will require retrieval but this is often at less risk than originally due to their migration away from the inferior alveolar nerve 15.
Conclusion
Inferior alveolar nerve injuries during third molar surgery can be reduced by:
- Thorough clinical assessment and decision making in line with guidance
- The use of appropriate imaging, including CBCT, to identify high-risk cases
- The use of the coronectomy technique where appropriate to prevent trauma to the inferior alveolar nerve.
Clinicians should consider coronectomy as an alternative to surgical removal for patients who are at a high risk of iatrogenic nerve injury.
References
- Management of unerupted and impacted third molar teeth. 1st ed. Edinburgh: Scottish Intercollegiate Guidelines Network; 2000.
- McArdle L, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J. 2012;213(5):E8-E8.
- Howe GL, Poyton HG. Prevention of damage to the inferior dental nerve during the extraction of mandibular third molars. Br Dent J 1960; 109: 355–363.
- SDCEP Oral Health Assessment and Review Guidance – Published March 2011. Available from: www.sdcep.org.uk/published-guidance/oral-health-assessment
- Ionising Radiation (Medical Exposures) Regulations 2000 (IRMER). Available from: www.legislation.gov.uk/uksi/2000/1059/contents/made
- FGDP – Selection Criteria for Dental Radiography: Third Edition. Published 2015. Accessed 14/06/2015. Available from www.fgdp.org.uk/publications/selection-criteria-for-dental-radiography1.ashx
- Palma-Carrio C, Garcia-Mira B, Larrazabal-Moron C, Penarrocha-Diago M. Radiographic signs associated with inferior alveolar nerve damage following lower third molar extraction. Medicina Oral Patología Oral y Cirugia Bucal. 2010;:e886-e890.
- European Commission – Radiation Protection No. 172 Cone Beam CT for Dental and Maxillofacial Radiology (Evidence-based Guidelines). Published 2012. Available from: www.sedentexct.eu/files/radiation_protection_172.pdf
- Matzen L, Christensen J, Hintze H, Schou S, Wenzel A. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy vs. surgical removal. Dentomaxillofacial Radiology. 2013;42(1):98870341-98870341.
- SIGN 43 – Management of Unerupted and Impacted Third Molar Teeth. Sign.ac.uk. Guidelines by topic. Available from: http://sign.ac.uk/guidelines/published/index.html#Dentistry
- NICE – Guidance on the Extraction of Wisdom Teeth. Available from: www.nice.org.uk/guidance/ta1
- Renton. T, Notes on Coronectomy. Br Dent J 2012; 212: 323-326
- Renton. T, Update on Coronectomy. A Safer Way to Remove High Risk Mandibular Third Molars Dent Update 2013; 40: 362–368
- Ahmed. C et al – Coronectomy of Third Molar: A Reduced Risk Technique for Inferior Alveolar Nerve Damage. Dent Update 2011; 38: 267–276
- Patel V, Gleeson C, Kwok J, Sproat C. Coronectomy practice. Paper 2: complications and long term management. British Journal of Oral and Maxillofacial Surgery. 2013;51(4):347-352.
- O’Riordan B. Uneasy lies the head that wears a crown. Br J Oral Maxillofac Surg 1997; 35: 209–212.
- Zola MB. Avoiding anaesthesia by root retention. J Oral Maxillofac Surg 1992; 50: 419–421.
- Pogrel MA. Coronectomy to prevent damage to the inferior alveolar nerve. Alpha Omegan 2009; 102: 61–67.
- Knutsson K, Lysell L, Rohlin M. Postoperative status after partial removal of the mandibular third molar. Swed Dent J 1989; 13: 15–22.
About the authors
Michael Dhesi is a GDP at Clyde Dental Centre. He qualified in 2012 with BDS(Hons) from the University of Glasgow and has subsequently completed MFDS RCPS(Glasg) and an MSc in Advanced General Dental Practice at the University of Birmingham. Michael’s focus is in minimally invasive and adhesive restorative dentistry.
He also has interests in the management of dental anxiety and oral surgery and welcomes referrals in these areas.
Clive Schmulian qualified from Glasgow University in 1993. Throughout his time in general dental practice, he has developed his clinical skills by obtaining a range of postgraduate qualifications, which in turn led him to develop an interest in digital imaging in both surgical and restorative dentistry. He is a director of Clyde Munro.
In 2013, 14 per cent of the world’s population was over 60 years of age. It is estimated that, by 2050, this figure will have increased to 19 per cent 1. However, as people age they develop more health conditions. Multimorbidity is the “presence of two or more diseases in one person” 2. Research indicates that, by 70 years of age, 63 per cent of people can expect to have developed two or more disorders 3.
Common chronic conditions in the elderly include cardiovascular disease, type 2 diabetes, depression, COPD and osteoarthritis. Multimorbidity has been shown to impact immune function greater than age alone 4.
These multiple chronic conditions can also result in polypharmacy where patients have to manage an increasing number of medications. In Europe, over half of the elderly population take more than six medications per day 5. This results in an increased risk of adverse drug events. Treatment plans for an elderly patient should be based on their individual risk factors, functional difficulties and preferences.
A growing elderly population increases the indications for partial removable dental prostheses and expands the indications for implant therapy. When considering implant surgery in elderly patients, pre-operative medical fitness is more important than chronological age 6.
The standard of care in geriatric patients has to be adapted to the patient’s motivation, medical condition and socio-economic circumstances. Oral health can significantly affect an elderly patient’s nutritional intake. It has been found that complete denture wearers have thinner masseter muscles whereas implant retained over-dentures lead to increased muscle thickness 7. Unlike most adults, a BMI >25 in elderly patients is associated with a reduced mortality. It is therefore important that elderly people can chew adequately to avoid restricted diets which offer lower nutritional values 8.
Medical consideration in elderly patients considering dental implant treatment
Cardiovascular diseases
These can be divided into atherosclerosis, hypertension, chronic heart failure and atrial fibrillation. A recent myocardial infarction, stroke and cardiovascular surgery is an absolute contraindication to implant surgery 9. Medical control of the disease is imperative prior to implant therapy. Patients with stent implantation after coronary artery disease usually have dual antiplatelet blood-thinning therapy to prevent clot formation.
Bleeding disorders
Bleeding can be prolonged in patients with haemophilia or those taking medication such as warfarin for anticoagulation. Current recommendations advise against modifying the anticoagulation provided the INR is <3.5. The exception may occur upon consultation with the patient’s medical team in cases of high volume bone grafting or extensive flaps. Splints can be used to manage expected bleeding.
The number of patients taking new oral anticoagulants such as dabigatran and rivaroxiban is increasing. New oral anticoagulants do not require monitoring, however, they lack a reversal agent. It is important that dentists follow the most recent guidelines regarding the management of these patients especially when considering invasive implant surgery 10.
Poorly controlled diabetes mellitus
This can result in delayed wound healing, an impaired response to infection and susceptibility to periodontal disease. Dentists should check their patient’s HbA1C (glycosylated haemoglobin) prior to implant placement. Implant and bone augmentation surgery in an uncontrolled diabetic can lead to serious wound healing complications.
- FIGURE 1 – Removable partial chrome cobalt denture
- FIGURE 2 – Extended implant fixed partial denture
- FIGURE 3 – Lower implant over-denture bar
- FIGURE 4 – Implant-retained over-denture
Osteoporosis
A decrease in bone mass and bone density increases the risk of fracture. Oral bisphosphonates reduce osteoclast function increasing the risk of bisphosphonate-related osteonecrosis of the jaw. Oral bisphosphonates are a potential risk factor for osteonecrosis of the jaw but not for implant success and survival 11.
Chronic obstructive pulmonary disease
Chronic bronchitis and emphysema result in a chronic cough, sputum production and shortness of breath. Special consideration needs to be given to the type of local anaesthetic administered. It is recommended that the maximum dose of local anaesthetic be halved in patients >65 due to reduced liver function 12. Also dentists should be mindful of the risk of adrenal insufficiency in elderly patients taking long-term steroids.
Psychological conditions
Depression is common among the elderly population. At the age of 90, three out of four patients have a diagnosis of dementia 13.
Treatment planning options
Shortened dental arch concept
The shortened dental arch is where 10 upper teeth oppose 10 lower teeth 14. Dentists can reduce the biological risks for the patient and avoid problems of low acceptance by providing this treatment option 15. Gerritsen et al concluded that a shortened dental arch can last for 30 years and that there is no recommendation for adding a partial denture. McKenna et al also examined the shortened dental arch concept in 89 patients who were >65 years old. His results demonstrated a better oral health related quality of life score in patients with a shortened dental arch compared with those wearing removable partial dentures 16.
Removable partial dentures (RPD)
This is an economical prosthodontic solution involving sound abutment teeth for increased retention. It helps maintain teeth of strategic value if implants are not an option 17. The prosthetic flange can also maintain facial fullness. However, abutment teeth for removable partial dentures are high risk for both caries and periodontal disease.
Prognostic factors for partial RPD abutments include 18:
- Crown-root ratio
- Root canal treatment
- Periodontal pocket depth
- Type of abutment – multi-rooted maxillary molars can make for unfavourable abutments
- Occlusal support and function of the abutment tooth.
Partial removable dentures with implants
Conventional dentures have limitations as oral function can decline with age. Old age is not a contraindication for dental implant treatment however; some medical conditions can increase their risk of failure. It is the degree of systemic disease control that is important rather than the nature of the disorder itself. Dentists should consider the American Society of Anesthesiology’s (ASA) Classification. The ASA restricts dental implants to ASA 1 and 2 patients. Dental implant placement may be undertaken in some very carefully considered ASA 3 cases.
In comparison with conventional dentures, implant over-dentures have the advantage of slowing peri-implant bone resorption and preventing bone atrophy 19. There is also a significant improvement in chewing ability with two lower implant supported over-dentures as a result of improved muscle co-ordination. Implants increase support, retention and can improve the aesthetic outcome of dentures by avoiding the use of clasps which results in greater patient satisfaction.
Strategic implant positioning can also help convert a Class I and Class II Kennedy arch into a Kennedy Class III configuration following the extraction of a hopeless abutment. This improves the elderly patient’s ability to eat harder food when compared with a conventional complete denture. This encourages elderly patients to eat a more diverse diet, which not only boosts their nutritional intake, but also enables them when socialising to finish their meals at the same time as family and friends 20.
Implant-supported over-dentures are also associated with psychological benefits such as improved social interactions and better self-confidence. Wismeijer et al examined patient satisfaction among 36 conventional and implant assisted partial denture wearers 21. The results showed a significant improvement in patient satisfaction with support of healing caps on implants as opposed to the conventional partial removable denture by itself. There was an even greater improvement in patient satisfaction when ball anchors were attached to the implants for retention.
In cases where patients are fully edentulous the recommended configurations are:
- Four or more implants in maxilla
- Two or more implants in mandible.
Removable options for the fully edentulous patient
The McGill Consensus statement on over-dentures recommends that “a two-implant over-denture should become the first choice of treatment for the edentulous mandible” 22. Implant-retained over-denture designs should be easy to clean, repair and also to re-activate retention. Long-term results suggest that a mandibular over-denture retained by two implants with a single bar may be the best treatment strategy for edentulous patients with an
atrophic ridge.
A bar can remove pressure from the tissue 23. There appears to be no influence with regards to the length of the cantilever arm (up to 12mm) and crestal bone loss 24. There is also good evidence to support the use of four implants with single retentive elements in the maxilla with a conventional loading protocol 25.
Combination syndrome
Two implants have an axis of rotation meaning that forces on the posterior ridge are higher than if the patient had a complete denture. Anterior flabby ridges and more posterior ridge loss can result from two implants necessitating more frequent denture relining in the upper jaw 26.
Short and reduced diameter implants
Short and reduced diameter implants are increasingly making dental implants possible in low and narrow alveolar ridges. They preserve bone and reduce the mouth opening requirements for an elderly patient. The surgery is less invasive and the need for augmentation procedures is eliminated, which results in less surgical morbidity.
The reduced complexity of the procedure also reduces the financial burden on the patient. Short and narrow implants make the reversible ‘backing off’ strategy easier if for instance a patient undergoing chemotherapy can no longer manage their dentures.
Implant configurations for Fixed Dental Prosthesis (FDP)
It is not necessary to replace every tooth that is missing in an elderly patient. Careful assessment is required when choosing the type and dimensions of implants. The minimal distance between teeth and implants must be respected and also bearing in mind the need for pink aesthetics. Short edentulous spaces that comprise of three missing teeth can normally be restored with two implants. Cantilevers help avoid bone augmentation procedures which can reduce the surgical morbidity for elderly patients.
Extended edentulous spaces have greater than three teeth missing. Implant positions are determined by the prosthodontic plan considering the number of teeth to be replaced, anatomical limitations and the bone volume present. When four teeth are missing in the anterior region, two implants and a FDP with a pontic or cantilever design can be utilised. When four teeth are missing posteriorly two to three implants are usually sufficient, utilising a one piece or segmented design.
An edentulous ridge can be restored with a one-piece FDP or three to four segmented FDPs. A full-arch one-piece FDP requires four to six implants. Utilising the shortened dental arch concept or cantilever units can help reduce the number of implants required for a FDP in the edentulous ridge. The implant sites should be evenly spaced if possible. Cantilevers can eliminate the need for a sinus augmentation procedure in the maxilla. Distal implants can also be straight or tilted to help avoid anatomical structures.
Full arch segmented FDP are indicated in certain cases where patients have gradually lost teeth or if segments need to be removed for periodic cleaning. Full arch segmented FDPs usually require more implants such as eight in the maxilla and six in the mandible. The implants can be strategically positioned to allow three to four short-span implant-supported FDP 27.
Conclusion
Dentists can provide life-changing treatment for patients of advanced age. Minimally invasive interventions with reduced healing times are recommended. Strategies for successful dental treatment for elderly patients must allow for frequent breaks, postural issues and increased chair time. Access and mobility issues can become barriers to care as patients become more reliant on others and experience reduced autonomy. It must be borne in mind that complications and prosthetic repairs are frequent 28.
Objective information should be clearly provided in writing and, where possible, with pictures. Declining cognitive function can affect a patient’s understanding of treatment, which raises the issue of valid consent. It is crucially important that patients have proven oral hygiene compliance. A prosthesis which is easy to manage and straightforward to clean will increase patient
acceptance 29. Neuroplasticitiy reduces in ageing patients making it difficult to develop new muscular patterns when adjusting to a denture.
Careful case selection is crucially important for patients advancing in age. It is important for dentists to address the patient’s specific concerns and to remember that the best treatment may not always be the most appropriate. Dentists must follow up on patients who have become institutionalised in order to implement a “back-off” strategy if necessary. Modifications that make denture management easier such as unscrewing an implant ball attachment and relining a denture can dramatically improve an elderly patient’s quality of life. The goal of treatment planning should allow for simple therapeutic step-back solutions if the patient enters a period of decline.
About the author
Dr Laura Fee graduated with an honours degree in dentistry from Trinity College, Dublin. During her studies, she was awarded the Costello medal for undergraduate research on cross-infection control procedures. She is a member of the Faculty of Dentistry at the Royal College of Surgeons and, in 2013, she completed the Certificate in Implant Dentistry with the Northumberland Institute of Oral Medicine and has since been awarded the Diploma in Implant Dentistry with the Royal College of Surgeons Edinburgh. Laura is currently completing the Certificate in Minor Oral Surgery with the Royal College of Surgeons, England. She has also been involved with undergraduate teaching in the School of Dentistry, Belfast where she has an honorary oral surgery contract.
References
- United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Ageing 2013
- Mercer et al Multimorbidity in primary care: developing the research agenda. Family Practice 2009 26(2):79-80
- Barnett et al Epidemiology of multimorbidity and implications for health care, research and medical education: a cross sectional study. The Lancet 2012:380:37-43
- Castle SC et al. Comorbidity is a Better Predictor or Impaired Immunity than Chronological Age in Older Adults. J Am Geriatr Soc. 53(9):1565-9
- Fialova et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005; 293:1348-1358)
- Seymour DG, Vaz FG. A Prospective-Study of Elderly General Surgical Patients 2: Postoperative Complications. Age and Ageing 1989 Sept, 18(5): 316-26
- F Muller et al. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: a cross-sectional multicentre study. Clinical Oral Implants Research, 2012, vol.23, no. 2,p.144-50
- Weiss A et al. Body Mass Index is Inversely Related to Mortality in Elderly subjects. Journal of General Internal Medicine 23(1) 19-24(2007)
- Hwang D, Wang HL. Medical contraindications to implant therapy. Part 1. Absolute contraindications. Implant Dent 2006;15(4): 353-60
- O’Connell JE, Stassen LF. New oral anticoagulants and their implications for dental patients. J Ir Dent Assoc 2014 Jun-Jul;60(3):137-43
- Kumar MN, Honne T. Survival of dental implants in bisphosphonate users versus non-users: a systemic review. Eur J Prosthodont Restor Dent 2012 Dec; 20(4):159-62
- Daublander M, Muller R, Lipp MDW. The incidence of complications associated with local anesthesia in dentistry. Anesth Prog 1997;44:132-141
- Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci USA 2010 107(22) 9985-90 – patients get happier as they age.
- Kayser AF. Shortened dental arch: a therapeutic concept in reduced dentitions and certain high-risk groups. Int J Periodontics Restorative Dent 1989;9(6):426-49
- Wostmann B. Indications for removable partial dentures: a literature review. Int J Prosthodont. 2005 Mar-Apr; 18(2):139-45
- McKenna et al The impact of rehabilitation using removable partial dentures and functionally orientated treatment on oral health-related quality of life: A randomised controlled clinical trial. Journal of Dentistry 2015 Vol.43(1):66-71
- Zitzmann et al. Strategic Considerations in treatment planning: deciding when to treat, extract or replace a questionable tooth. J Prosthet Dent. 2010 104(2):80-91
- Tada et al. Multifactorial risk assessment for survival of abutments of removable partial dentures based on practice-based longitudinal study. J Dent 41 (2013) 1175-1180
- Tallgren A.The continuing reduction of the residual alveolar ridges in completed denture wearers: a mixed-longitudinal study covering 25 years. J Prothet Dent 1972 Feb; 27(2):120-32
- Van Kampen FM. Masticatory function with implant-supported over-dentures. J Dent Res 2004 Sep; 83(9):708-11
- Wismeijer D. Multicentre prospective evaluation of implant-assisted mandibular bilateral distal extension removable partial dentures: Patient Satisfaction. Clin Oral Impl Res 24,2013,20-27
- J Feine, GE Carlsson et al. The McGill consensus statement on over-dentures. Gerodontology 2002 Jul 19(1):3-4
- Timmerman R, Stoker GT, Wismeijer D, Oosterveld P, Vermeeren JI, Van Waas MA. An eight-year follow-up to a randomised clinical trial of participant satisfaction with three types of mandibular implant-retained over-dentures. J Dent Res 2004 Aug; 83(8):630-3
- Semper W, Heberer S, Nelson K. Retrospective analysis of bar-retained dentures with cantilever extension: marginal bone level changes around dental implants over time. Int J Oral Maxillofac Implants. 2010 Mar-Apr; 25(2): 385-93
- Gallucci GO, Morton D; Weber HP Loading protocols for dental implants in edentulous patients. IJOMI 2009; 24(Suppl)132-146
- Kreisler M. Residual ridge resorption in the edentulous maxilla in patients with implant-supported mandibular over-dentures: an eight-year retrospective study. Int J Prosthodont 2003 May-Jun; 16(3):295-300
- Papadimitriou DE, Salari S, Gannam C, Gallucci GO, Friedland B. Implant-prosthodontic classification of the edentulous jaw for treatment planning with fixed rehabilitations. Int J Prosthodont.2014 Jul-Aug; 27(4):320-7
- Shamiri RA, Atieh MA Mandibular Kennedy Class 1 implant-tooth-borne removable partial denture: a systemic review. J Oral Rehabil 2010 Mar; 37(3): 225-34
- Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci USA 2010 107(22) 9985-90
As one of the largest specialist referral dental practices in the country and with more than 20 years of experience managing patients with dental implants, we have seen many surgical and restorative “trends” come and go (often on more than one occasion). These include: block bone grafting, guided surgery, distraction osteogenesis, cemented restorations, platform switching and composite resin bridgework.
In the last few years, the most concerning of these, for us, has been the rise of peri-implantitis, both in terms of perceived incidence and proposed management. Well-meaning practitioners (generalist and specialist), together with representative bodies in the profession, have advocated using periodontal indices to produce algorithms for monitoring dental implants (See ADI algorithm overleaf).
The algorithms dictate when and how “ailing” implants should be treated. Such algorithms are only effective if periodontal indices are a reliable predictor of treatment needs. If not, there is a very real concern that many patients will, and are being, unnecessarily treated, often at great expense and with significant mental anguish.
Our prosthodontists, periodontists and oral surgeons have analysed and discussed at length the literature available on peri-implantitis.
This article and the one that follows are taken from a more extensive paper which investigates in detail the evidence to support the use of periodontal indices in implant monitoring. The paper has been submitted and accepted for publication in Periodontology 2000.
Clinical evidence does not support the published data
Osseointegrated dental implants have been used for more than 50 years and have truly revolutionised modern clinical dentistry. This treatment modality has given clinicians the possibility to give totally edentulous patients back their teeth and dignity.
In the same way, partial edentulism and single tooth gaps can be successfully managed with dental implants as a first choice of treatment to restore function and aesthetics without damaging remaining teeth. The use of dental implants is scientifically well documented and numerous long-term studies have shown predictable results with few serious complications. Moreover, due to better understanding of the biology of implants, improved components and clinical techniques, the literature has shown increasingly improved clinical outcomes with time (Figures 1, 2 and 3).
In spite of this, critical reports claim that up to 56 per cent of dental implants show signs of disease when examined with periodontal indices such as probing pocket depth (PPD), bleeding on probing (BoP) and radiographic marginal bone loss (MBL)1,2. Extrapolation of these findings based on the rationalities of periodontal diagnostics tools, suggests a future tsunami of “peri-implantitis”, i.e. severe marginal bone resorption, and subsequent implant losses (Figure 4).
Based on the same logic, it is recommended that the diseased implants need to be treated with non-surgical or surgical interventions to “resolve the disease”3. In an editorial in a highly ranked dental journal4, a restricted use of dental implants was advocated. This advice was based on the findings from a series of studies5–7 in the same journal claiming high levels of peri-implant disease among a large group of patients. If correct, our waiting rooms would be crowded by previously treated implant patients, now suffering from peri-implantitis.
In addition, the literature would be dominated by clinical reports with catastrophic failure rates. On the contrary, large numbers of suffering implant patients are missing and the scientific literature repeatedly demonstrates dental implants to be very successful with failure rates around 5 per cent after 10 years with about 2-3 per cent of implants affected by severe marginal bone loss and so called peri-implantitis8.
One may argue that most scientific follow-up studies are made in well-controlled academic environments and for that reason the results do not reflect clinical reality out in the field. However, it is notable that from the series of studies claiming high levels of peri-implant disease as referred to in the critical editorial, the same research group demonstrated only a
1.4 per cent early failure rate for 11,311 implants placed in 2,765 patients in the hands of more than 800 clinicians, and a 3 per cent total failure rate for a subgroup of 596 patients examined after nine years of function6. However, in spite of this, the authors of the study6 concluded that “implant failure is not an uncommon event”. In reality most of us would rejoice over such outstanding results.
Risks with surrogate endpoints in clinical research
How is it even possible to reach so different conclusions based on the same knowledge?
The answer is that the different research groups use different endpoints in their research9. Most clinical implant investigations are using true endpoints as primary parameters and measuring clinical outcomes in terms of definitive events, i.e. loss and removal of the implants and of the associated prosthetic restorations, whereas others are using surrogate endpoints (BoP, increased PPD) that, according to their hypothesis, will eventually lead to a definitive event (implant loss).
One example is one of the first studies reporting on alarming levels of peri-implant disease based on BoP and bone loss occurring after the first year of function10. According to the authors, about 56 per cent of all implants were affected by disease and had an expected poor prognosis. However, when analysing the same patient cohort nine years later, there were no differences between “affected” and healthy implants with regard to implant failures11. Moreover, 91.4 per cent of the implants in the patients diagnosed with peri-implantitis showed either no or minimal annual bone loss during the nine years from the diagnosis. Hence, the surrogate endpoints used by the authors, namely bone loss associated with bleeding on probing, were shown to be poor predictors of future bone loss and implant failure and consequently poor indicators of treatment needs (Table 1). With such a periodontal approach for the diagnosis of peri-implant diseases, there is an obvious risk that patients will be subjected to unnecessary treatment, which is unacceptable from an ethical point of view as it may create iatrogenic as well as economic damage to the patients.
Teeth versus implants (Figure 5)
The periodontal complex is the result of millions of years of evolution and is built up by highly differentiated and specialised tissues. Osseointegration on the other hand, is the result of a foreign body reaction to an implant. The soft and bone tissue interfaces consist of lowly differentiated scar tissues12,13. Hence, from a morphological point of view, the tooth and the implant represent two different entities, which cannot be directly compared.
Inflammation and marginal bone loss at teeth, i.e. gingivitis and periodontitis, are considered as infectious and biofilm-mediated conditions. These are diagnosed by probing, where bleeding (BoP) indicates gingivitis and increased pocket depths (PPD) with bleeding (BoP) and bone loss indicate periodontitis. Removal of the biofilm and bacteria formation will resolve the inflammation/infection. This means that clean teeth will not show any signs of bleeding and increased pocket depths.
Dental implants and mucosa-piercing components are placed in edentulous areas of the jaws during one or two surgical interventions. It is well documented that some marginal remodelling will occur during the first year as a response to surgery, piercing of the mucosa and loading. For a large group of implants, the average bone loss during the first year in function varies from 0.5 to 1.5 mm, mainly depending on the geometry of the implant 14,15. After the first year in service, small changes of marginal bone loss are observed over the following years of follow-up.
However, if making a frequency distribution of bone loss, some implants will show more bone loss than other implants 16. The reasons for bone loss can be physiological atrophy after tooth extraction, non-optimal surgery and prosthetic design, overload, thin bone, soft bone, cement residues just to mention a few (Figure 6). This means that healthy and well-functioning dental implants, in contrast to teeth, can show non-infectious marginal bone resorption. Even in a hypothetical environment without bacteria, there will be bone loss around implants. For this reason, a zero-tolerance approach to bleeding, pocket depths and some marginal bone loss does not appear to be justified.
It is often pointed out that patients with a history of severe periodontitis are more susceptible to marginal bone loss at dental implant (Figure 7). Some authors see this as a proof of a bacterial and biofilm-induced process. However, another plausible explanation is that this is related to the immunologic foreign-body response to plaque and implant components in these patients, which for some reason is exaggerated 11.
The use of periodontal diagnostic techniques at implants
In analogy with teeth, the rationale for using a dental probe round implants is to identify “affected” implants based on the presence of any BoP and PPDs deeper than 4 mm, which in combination with any radiographic bone loss, would indicate disease. In reviewing the literature, it is evident that BoP may be detected in more than 90 per cent of well-functioning dental implants 17. Likewise, PPDs over 4 mm are frequent round healthy implants (Figure 8). The depth of the peri-implant pocket is not immediately pathological; it is, of course, dependant on the thickness of the mucosa and how deep the implant was placed.
As discussed earlier, literally all implants will show some bone loss over time as a result of many other factors than simply the “catch all” of biofilm-mediated resorption. A recent review of the literature, where studies on the use of periodontal probes to diagnose peri-implant health have been used, 17 concluded that:
- Probing pocket depth values of >4 mm at dental implants cannot be seen as a sign of pathology or an alarming signal regarding the conditions of the peri-implant tissues.
- An increase of probing pocket depth values over time is not necessarily associated with loss of supporting bone around dental implants. Therefore, probing does not appear to be a reliable tool for the assessment of peri-implant marginal soft- and hard-tissue conditions.
- From a biomaterials science point of view, osseointegration is a foreign-body reaction. As a consequence, bleeding on probing does not always indicate the presence of acute inflammation in the peri-implant mucosa, but may rather reflect the nature of the scar tissue–implant interface. Therefore, bleeding on probing does not appear to be a predictor for future loss of tissue support. Similarly, absence of bleeding on probing does not appear to be a predictor of future stability. Hence, probing pocket depth and bleeding on probing cannot be considered to be reliable tools for monitoring peri-implant health and disease.
- Radiographic evaluation of crestal bone levels over time seems to be the most reliable tool to identify those implants undergoing continuous bone loss and therefore in need of treatment.
- A single episode of bone loss does not necessarily call for treatment unless associated with clear signs of inflammation, such as profuse bleeding/suppuration and discomfort at pressure/palpation.
Conclusion
This first of a two-part paper has been written to address the possibility that using periodontal indices to monitor dental implant health may not only be unnecessary but in many circumstances may result in patients receiving treatment that they don’t need.
In part two, we will look at proposed guidelines for routine follow up of dental implants and how true peri-implantitis lesions may be managed.
- FIGURE 1: Failing crown and bridgework
- FIGURE 2: Fixed full arch bridge porcelain finish
- FIGURE 3: Appearance, function and dignity predictably returned
- Article from the Telegraph website (14 July 2014)
- Figure 5: A comparison of how a natural tooth and an implant attaches to the bone
- FIGURE 6: Bone remodelling is to be expected round healthy implants and is not necessarily due to biofilm mediated pathology
- FIGURE 7: Are periodontitis patients more susceptible to periimplantitis
- FIGURE 8: Perfectly healthy implant with more than 4mm pocket depth and BoP
- ADI maintenance algorithm
REFERENCES
- Lindhe J, Meyle J. Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J ClinPeriodontol 2008: 35: 282–285.
- Lang NP, Berglundh T. Peri-implant diseases: where are we now? Consensus of the Seventh European Workshop on periodontology. J ClinPeriodontol 2011: 38: 178–181.
- Ucer C, Wright S, Scher E, West N, Retzepi M, Simpson S, Slade K, Donos N. ADI guidelines. On peri-implant itoring and maintenance. 2013: http://www.adi.org.uk/resources/guidelines_and_papers/peri-implant/
- Giannobile WV, Lang NP. Are dental implants a panacea or should we betterstrive to save teeth? J Dent Res 2016: 95:5–6.
- Derks J, Håkansson J, WennströmJL, Klinge B, Berglundh T. Patient-reported outcomes of dental implant therapy in a large randomly selected sample. Clin Oral Implants Res 2015: 26: 586–591.
- Derks J, Håkansson J, WennströmJL, Tomasi C, Larsson M,Berglundh T. Effectiveness of implant therapy analyzed in a Swedish population: early and late implant loss. J Dent Res2015: 94(3 Suppl.): 44S–51S.
- Derks J, Schaller D, Håkansson J, WennströmJL, Tomasi C,Berglundh T. Effectiveness of implant therapy analyzed in a Swedish population:
prevalenceof peri-implantitis. J DentRes 2016: 95: 43–49. - Albrektsson T, Buser D, Sennerby L. Crestal bone loss and oral implants. ClinImplant Dent Relat Res 2012: 14: 783–791.
- Psaty BM, Weiss NS, Furberg CD, et al. (1999). “Surrogate end points, health outcomes, and the drug approval process for the treatment of risk factors for cardiovascular disease”.JAMA. 282 (8): 786–790.
- Fransson C, Lekholm U, Jemt T, Berglundh T. Prevalence of subjects with progressive bone loss at implants. Clin OralImplants Res 2005: 16: 440–446.
- Jemt T, Sundén Pikner S, K Gröndahl. Changes of marginal bone level in patients with ‘progressive bone loss’ at Brånemark System implants: a radiographic follow-up study over an average of 9 years. ClinImplant Dent Relat Res2015: 17: 619–628.
- Donath K. Pathogenesis of bony pocket formation around dental implants. J Dent Assoc S Afr 1992; 47:204–208.
- Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, WennerbergA. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? ClinImplantDent Relat Res 2014: 16: 155–165.
- Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science? J Periodontol 2002: 73:322–333.
- Laurell L, Lundgren D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. ClinImplant Dent Relat Res 2011: 13: 19–28.
- Pikner SS, Gröndahl K, Jemt T, Friberg B. Marginal bone loss at implants: a retrospective, long-term follow-up of turned Brånemark System implants. ClinImplant Dent Relat Res. 2009 Mar;11(1):11-23.
- Coli P, Christiaensen V, Sennerby L, De Bruyn H. Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontology 2000, in press
About the authors
- Dr Pierluigi Coli is a specialist in periodontics and prosthodontics at Edinburgh Dental Specialists.
- Dr Kevin Lochhead is a specialist in prosthodontics and principal dentist at Edinburgh Dental Specialists.
- Professor Lars Sennerby is a visiting professor in implantology at Edinburgh Dental Specialists.
When resin-based composite is cured it shrinks by a factor of between 2 to 4 per cent depending on the product. This polymerisation shrinkage causes stresses to be incorporated in the system, either within the surrounding tooth tissue, at the restoration/tooth interface or within the body of the restorative material. These stresses may lead to partial or total debond, recurrent caries, microleakage, pulpal inflammation, marginal staining, fracture or micro-fracture of the surrounding tooth or pain on chewing 1–5.
Furthermore, the depth of light cure of conventional resin composite products is limited 6,7. To achieve a full curing of the resin composite, sufficient light energy of the correct wavelength of light must be provided to all of the material. In an attempt to overcome these potential problems, an incremental placement technique has long been advocated 8,9
particularly when restoring posterior teeth.
Firstly, the shrinkage which occurs with the first increment may be compensated for by the subsequent increment and so on. Secondly, it permits the dentist to place each increment such that as few walls are bonded together as possible to reduce the configuration or C factor 10 in attempt to control the stresses. Lastly, each incremental of material may be fully cured as sufficient light may attenuate through the smaller bulk of material. This placement technique is therefore time consuming, tedious and requires meticulous technique6.
The so-called bulk-fill resin composite materials have been introduced to the market in recent years with the aim of reducing polymerisation shrinkage stresses as well as simplifying and quickening the clinical placement of the material. This case report describes the successful resolution of symptoms of pain when a conventional methacrylate based posterior resin composite material was replaced by a bulk-fill restorative material.
Case report
A 35-year-old female geotech engineer with a clear medical history presented for her routine dental examination. A debonded, but still in situ, disto-occlusal resin composite in 16 was diagnosed with no obvious caries present. An appointment was made so that the restoration could be replaced.
At the treatment appointment, a local anaesthetic was administered and rubber dam placed. The existing restoration was removed and cavity refined. As it was considered not to be deep, no lining was considered necessary. After a sectional matrix system (V Ring, Triodent) had been placed, the cavity was etched with Scotchbond Universal Etchant (3M ESPE) for 15 seconds, washed for 15 seconds and lightly air-dried leaving a glassy dentine surface.
Adper Scotchbond 1XT (3M ESPE) was then applied, air thinned and cured for 20 seconds. Filtek P60 Posterior Restorative (3M ESPE) was placed into the cavity using an incremental placement technique with each increment cured for 40 seconds. The matrix system was removed and gross finishing done using diamond finishing burs (Figure 1). Once the rubber dam had been removed and the occlusion checked, the restoration was polished using rubber points.
However, the patient returned two weeks later complaining of a tenderness on biting which necessitated her avoiding using the tooth. She had some sensitivity to cold stimuli but this had settled a few days before the unscheduled appointment. Clinical examination revealed nothing untoward and so the patient was reassured but advised to return if things did not settle. Unfortunately, as the same pain on biting was persisting, she returned a fortnight later. Clinical examination revealed that 16 was tender on application of a Tooth Slooth and when pressure was released when the tooth was squeezed. The diagnosis was therefore made of cracked cusp syndrome most likely precipitated by stresses caused by the polymerisation shrinkage of the resin composite. The patient was advised that the restoration should be replaced in an attempt to remove any stresses within the tooth tissue.
At a subsequent appointment, local anaesthetic was again administered, rubber dam placed and the restoration removed (Figure 2). A sectional matrix system (V Ring, Triodent) was placed, the cavity was etched with Scotchbond Universal Etchant (3M ESPE) for 15 seconds (Figure 3).
The etchant was washed using water from the three-in-one syringe for 15 seconds and lightly air dried leaving a glassy dentine surface. Adper Scotchbond 1XT (3M ESPE) was applied, air- thinned and cured for 20 seconds. As before,
no lining was considered necessary as the bonding agent would seal the dentinal tubules. Filtek Bulk Fill Posterior (3M ESPE) was placed into the cavity in a single increment, contoured before being light cured for 40 seconds (Figure 4).
The restoration was grossly finished using diamond finishing burs after the sectional matrix had been removed (Figures 5 and 6). The rubber dam was removed, the occlusion checked and the restoration finished and polished (Figure 7).
The patient was reviewed at her routine six-monthly dental examination four months later. She had no complaints as the symptoms of pain had resolved completely and very quickly after the appointment to replace the conventional posterior resin composite restoration with the bulk-fill product. The patient has been reviewed for
her routine dental examination six months subsequent to this and the tooth remains asymptomatic and signless.
Discussion
This case is interesting as, in many respects, direct comparison may be made between both the original appointment and the subsequent remedial appointment as the procedure performed was largely identical. The operator, the method of anaesthesia, timing and placement of rubber dam, burs, sectional matrix system, etch, bonding agent and method and instruments used to finish the restoration were the same at both appointments.
The only differences were that a bulk-fill product was used instead of a conventional posterior resin composite and the former product was placed in one increment by definition. The placement of the conventional resin composite could be viewed as a “control” and a direct means of comparison to the new bulk-fill product.
It is known that stresses may be incorporated into the system as a result of polymerisation shrinkage which occurs when the resin composite is cured1. In this case, these stresses had precipitated signs and symptoms of incomplete fracture of the tooth structure (cracked cusp syndrome) despite its meticulous placement in the first instance. Bulk-fill resin composites were developed in an attempt to reduce these stresses and simplify and so quicken their clinical placement. This has been made possible by the manufacturer making some modifications to the constituents of the material.
In the case of the product used in this case, BisGMA (the most commonly used monomer in resin composite products) has been omitted in favour of other monomers such as ERGP-DMA, urethane dimethacrylate (UDMA) or 1,12-Dodecane dimethacrylate (DDDMA) 11. UDMA is relatively low viscosity high-molecular weight monomer which means that there are fewer reactive groups and so the volumetric shrinkage is minimised. Furthermore, the stiffness of developing and final polymer matrix is decreased but a tough, highly cross-linked network is still created.
DDDMA provides a high modulus resin with good flexibility and impact resistance. This monomer cures quickly and exhibits a low exotherm and low shrinkage. The omission of BisGMA means that bisphenol A is, by definition, absent following concerns over its potentially oestrogenic side effects such as breast and prostatic carcinomas and male infertility. Two other monomers have been incorporated in the resin system which work in combination to reduce polymerisation stresses 11. One is a high molecular weight aromatic dimethacrylate (AUDMA) with a reduced number of reactive groups. This moderates the volumetric shrinkage and the stiffness of the developing and final polymer matrix.
Another class of compounds called addition-fragmentation monomers (AFM) work in combination with AUDMA to decrease the shrinkage stress. These methacrylate molecules react into the developing polymer by forming crosslinks between adjacent polymer chains. When stressed during polymerisation, these molecules may break or fragment so providing a means for relaxation of the developing polymer network and so stresses are relieved.
These fragments also react with each other or other nearby reactive sites in a less-stressed environment as the polymer develops. This process goes to completion maintaining the physical properties of the polymer as the conversation is the same but with greatly reduced polymerisation stress. This was well illustrated in the present case with almost immediate resolution of the patient’s symptoms of pain.
The bulk fill product was placed in one increment as the cavity was shallower than 4mm. To enable light to fully penetrate through the material to permit an increased depth of cure, the manufacturers may utilise three strategies to achieve this:
- Lower the filler content and/or increase the filler particle size
- Modify the resin to increase its translucency
- Use a different photoinitiator system.
The filler used in Filtek Bulk Fill Posterior (3M ESPE) is a silicon/zirconia nanofiller which conveys good wear resistance, increased strength, excellent polish retention and favourable handling. The total inorganic filler loading of approximately 76.5 per cent by weight (58.4 per cent by volume) 11. This may be compared to the filler loading of a flowable resin composite which is approximately 65 per cent by weight.
This means that the second generation of bulk fill products of which Filtek Bulk Fill Posterior (3M ESPE) is an example, can be used to restore the entire cavity without the need for a veneering layer using a resin composite indicated for use in the posterior region which is necessary with the lower viscosity products 12 as they have inferior mechanical properties due to their lower filler loading. Due to other modifications in the chemistry of the material discussed elsewhere in this paper, the higher filler load has been possible without any detrimental effect on light attenuation.
Bulk-fill materials tend to be more translucent to permit increased light attenuation through its mass. The manufacturer of the product used in the present case describes the material as semi-translucent 11. As can be seen in Figure 7, the aesthetics of the cured material are acceptable but a slight mismatch in shade is evident between the resin composite and tooth tissue. This is considered advantageous by many clinicians because, if the restoration requires to be subsequently removed, the tooth tissue may be more easily identifiable and so may be preserved6.
Many of the bulk-fill products available on the market use photoinitiators which have a higher visible light absorption rate which allows increased quantum efficiency. In simple terms, this means that a lower quantity of light (photons) is required to trigger the polymerisation free-radical chain reaction. This results in improved light-curing performance and an increase depth of cure.
These modifications to the chemistry of this product has allowed the placement of Filtek Bulk Fill Posterior (3M ESPE) in one increment which greatly simplified and quickened the clinical procedure.
Conclusion
This case illustrates that an alternative low-stress material (so-called bulk fill) may successfully resolve symptoms caused by polymerisation stresses when conventional resin composite is cured as it exhibits markedly reduced polymerisation stresses. Consideration should be given to selecting one of these bulk-fill materials in preference to a conventional posterior resin composite material when working in the posterior region of the mouth, not only in terms of stress reduction but the clinical procedure is simpler and quicker.
Conflict of interest/commercial interests
The author denies any commercial interest in any of the products or companies mentioned in this paper.
- FIGURE 1: 16 DO cavity restored with Filtek P60 Posterior Restorative (3M ESPE) after gross finishing but before the rubber dam had been removed
- FIGURE 2: The completed cavity after the restoration had been removed
- FIGURE 3: A V Ring (Triodent) sectional matrix placed and the cavity etched with Scotchbond Universal Etchant (3M ESPE)
- FIGURE 4: Filtek Bulk Fill Posterior (3M ESPE) after light curing
- FIGURE 5: The Filtek Bulk Fill Posterior (3M ESPE) restoration after gross finishing
- FIGURE 6: A higher magnification photograph, note the good contact area
- FIGURE 7: The completed 16DO Filtek™ Bulk Fill Posterior (3M ESPE)
References
- Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res 1984 Dec;63(12):1396-1399.
- Davidson CL, Feilzer AJ. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J Dent 1997 Nov;25(6):435-440.
- Letzel H. Survival rates and reasons for failure of posterior composite restorations in multicentre clinical trial. J Dent 1989;17 Suppl 1:S10-7; discussion S26-8.
- Tantbirojn D, Versluis A, Pintado MR, DeLong R, Douglas WH. Tooth deformation patterns in molars after composite restoration. Dent Mater 2004 Jul;20(6):535-542.
- Loguercio AD, Reis A, Schroeder M, Balducci I, Versluis A, Ballester RY. Polymerization shrinkage: effects of boundary conditions and filling technique of resin composite restorations. J Dent 2004 Aug;32(6):459-470.
- Bonsor SJ, Pearson GJ. A Clinical Guide to Applied Dental Materials. 1st ed. Edinburgh: Churchill Livingstone Elsevier; 2013.
- Yap AU. Effectiveness of polymerization in composite restoratives claiming bulk placement: impact of cavity depth and exposure time. Oper Dent 2000 Mar-Apr;25(2):113-120.
- Lee MR, Cho BH, Son HH, Um CM, Lee IB. Influence of cavity dimension and restoration methods on the cusp deflection of premolars in composite restoration. Dent Mater 2007 Mar;23(3):288-295.
- Poskus LT, Placido E, Cardoso PE. Influence of adhesive system and placement technique on microleakage of resin-based composite restorations. J Adhes Dent 2004 Autumn;6(3):227-232.
- Feilzer AJ, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res 1987 Nov;66(11):1636-1639.
- 3M ESPE. Filtek Bulk Fill Posterior Restorative Technical Product Profile.
- Burgess J, Cakir D. Comparative properties of low-shrinkage composite resins. Compend Contin Educ Dent 2010 May;31 Spec No 2:10-15.
According to the Oxford English Dictionary, one definition of revolution is: “a dramatic and wide-reaching change in attitude”. For decades the porcelain veneer has reigned supreme and the use of other materials for veneering teeth has received little support. Etching of enamel had been demonstrated by Buonocore in the late 1950s, but it was not until as recently as 1982 that Simonsen and Calamia demonstrated that, by etching porcelain with hydrofluoric acid, porcelain could be bonded to enamel with composite resin 1.
This discovery led to dentists suddenly being able to transform a patient’s appearance with a relatively minimally invasive technique. Initially there was a debate to whether tooth preparation was necessary but, over time, it was generally accepted that the tooth was prepared before construction of veneers, otherwise the tooth appeared a little over-contoured. Obviously, with a peg-shaped lateral incisor, tooth preparation might be minimal or not necessary. Direct composite veneers have always been part of the dentist’s armamentarium but have been provided as either a provisional restoration or on the grounds of economics.
The preparation of teeth has attracted some controversy. Incisal coverage or removal of contact points are two areas where dentists differ in their approach. In fact, there is a metaphorical fine dividing line between a veneer and a ‘veneer crown’, depending on one’s point of view, in teeth that have been prepared towards the palatal margin and where the contacts have been removed.
New manufacturing techniques have allowed porcelain veneers to be made extremely thin and so negating the need for tooth preparation in many cases (e.g. Lumineers). Whitening or dental bleaching has concomitantly developed over the past few decades, and has become more predictable. In a large number of cases this should mean that the need for full mouth veneers is reduced. Sadly, this is not the case and has led to the term “porcelain pornography” being coined by Professor Martin Kelleher 2 with regards to unnecessary restorative dentistry being performed to enhance a patient’s appearance.
Furthermore, while on the face of it veneers seem very simple to perform, they are extremely technique sensitive and demanding. Inappropriate case selection, over preparation, over contouring, shade errors and poor execution of bonding techniques are just a few of the problems that have plagued the provision of porcelain veneers.
Composites and bonding techniques have exponentially improved from the original materials developed in the 1960s and 70s. Microfills, hybrids, nano hybrids along with multi- generation bonding agents has meant that both longevity of restorations and aesthetics have improved dramatically. In the past year or so a template system for use with composites has been introduced to the market, the UVeneer (Ultradent). It was developed by dentist Dr Sigal Jacobson 3, and has given the clinician more choice when providing definitive veneer restorations. No longer should the automatic choice be porcelain and serious consideration should be given to the UVeneer as an alternative.
UVeneers are fully autoclaveable plastic templates that are available in two sizes, large and universal (Figure 1). They are arranged in racks, from first premolar to first premolar, for both arches. When used with composite they block out the oxygen inhibited layer, which gives a harder more colour stable surface with an unrivalled gloss. The advantages and disadvantages of the UVeneer are outlined below:
Advantages
- One visit
- Once mastered, technique is simple and repeatable
- No laboratory costs
- Shade changes easily made as necessary at time of visit
- Only necessary to trim margins and no need to polish
- Enhanced physical properties to outer surface and therefore potentially longer lasting than a direct restoration without a templates
- Easily repaired or renewed
- Time?
- Cost to the patients.
Disadvantages
- Multiple units are demanding
- Wear incisally and labially/buccally
- Staining
- Longevity less than porcelain/ceramics?
- Two sizes enough for all cases?
- Patient acceptance as opposed to conventional porcelain/ceramic.
The time element is variable but experience as well as the individual complexity of the case will determine this factor. Given that only one visit is required and there is no temporisation required, the time element may work in favour of the UVeneer when compared to porcelain. The physical properties of composite have improved dramatically since the 1970s, but it would be a bold statement to make that they rival porcelain in all aspects.
With exceptionally large or small teeth the UVeneer is not suitable, but suffice to say it can be used for the vast majority of cases. Multiple units can mean lengthy appointment times, which with porcelain is spread over two appointments. Wear due to abrasion or attrition may occur over prolonged periods and may be a deciding factor in the choice of material.
Clinical technique
A middle-aged female presented with a very white veneer, and wished to have it replaced (Figs 2 and 3). She had no desire to whiten the rest of her teeth but rather wanted the veneer to match her existing teeth. The veneer was removed and the preparation modified. It will be noticed that some veneer cement is still present adhered to the preparation (Fig 4). Air abrasion is utilised and, consequently, the necessity to completely eradicate every vestige of bonding material is negated (Fig 5).
The choice of template is easy to make as for every anterior tooth it is either universal or large. The tooth is etched and bonded in the usual fashion and either metal or clear matrix strips are used to prevent overhangs or bonding to the adjacent teeth (Fig 6). For optimal results, a small amount of flowable composite is placed onto the inner surface of the template chosen (Fig 7). Directly onto the flowable composite a small amount of enamel composite is placed and spread out thinly over the surface of the template, with a flat plastic instrument (Fig 8).
Dentine composite is then applied onto the tooth and spread over the surface, before placing the template directly onto it. The excess is removed with a probe, with care being taken not traumatise the gingiva and cause it to bleed. It is important to ensure excess material is removed, as this will mean quicker and easier finishing later (Fig 9). The tooth is subsequently light cured.
If in any doubt to the health of the gingiva, ideally delay the procedure until this has improved or, at the very least, cure the restoration first before finishing as the margins would be contaminated with blood or gingival exudate. There is also a vertical line on the outer surface of the template to aid the placement vertically on the long axis of the tooth.
There are many enamel and dentine composite systems on the market and, in this particular case, VOCO Amaris was used, with the added advantage that a highly translucent flowable is available with the system. It is possible to use any flowable composite, as the layer is so thin as to have very little influence on colour. Furthermore, it is possible to use a single shade composite rather than separate dentine and enamel shades as with conventional restorations, but for optimal aesthetics the latter method is preferred.
The template is pulled off the composite after curing (Fig 10) and, after careful cleaning, can be autoclaved and reused. There is no need to polish the facial surface of the finished restoration. A fine finishing diamond bur is all that is required to remove excess restorative material (Figs 11 and 12).
Conclusions
As with any new technique, there is a learning curve and the UVeneer is no different. The UVeneer can be used to provide “facings” for temporary or provisional restorations. If a tooth is lost whether from periodontal disease, trauma or an extraction, the UVeneer can provide aesthetic form to an immediate pontic. There are obviously many other scenarios where the Uveneer might prove useful. Once proficient with the technique, the question whether to use porcelain or a UVeneer and composite becomes a foremost consideration when providing veneers.
- Figure 1: U Veneer templates
- FIGURE 2: A middle-aged lady presented with a very white and unsightly porcelain veneer
- FIGURE 3: The patient requested to have the existing veneer replaced
- FIGURE 4: Old veneer is removed. Note that some veneer cement is still adhered to the labial surface of the tooth
- FIGURE 5: Air abrasion is used on the labial surface of the tooth
- FIGURE 6: Bonding agent is applied to the tooth surface
- FIGURE 7: Flowable composite is placed on the inner surface of the UVeneer template
- FIGURE 8: A thin layer of enamel composite is then laid upon the flowable composite
- FIGURE 9: After administering the dentine composite to the tooth surface, the template is carefully seated before removing any excess material
- FIGURE 10: After light curing, the template is removed and a finishing bur can then excise any flash at the margin. Care must be taken not to touch the facial surface of the restoration
- FIGURE 11: The completed restoration
- FIGURE 12: A more natural and aesthetically pleasing veneer
Socket preservation is a procedure that reduces bone and soft tissue loss after tooth extraction. It is performed immediately after tooth extraction. It has been found that ridge preservation procedures following tooth extraction result in greater orofacial dimension of bone when compared with cases where no ridge preservation procedures are completed 1.
Socket preservation is indicated as tooth extraction can have a significant impact on the facial bone height 2. After eight weeks of healing there is, on average, 20 per cent horizontal resorption and a 50 per cent reduction of vertical bone wall height 3.
Immediate implant placement does not counteract alveolar ridge modelling after tooth extraction 4. Socket preservation compensates for the biologic resorption of the facial bone wall. It aids implant placement and can reduce the need for later bone augmentation. By reducing marginal bone loss on adjacent teeth and accelerating bone formation it can increase implant survival and success 3.
Socket preservation should be considered when: 5
- Implant placement needs to be delayed for patient or site-related reasons
- In situations where implant placement for some reason needs to be postponed for more than months
- Future fixed partial denture pontic site is planned.
Post-extraction healing
The alveolar process resorbs after tooth extraction, significantly impacting oral rehabilitation with dental implants and other types of prosthesis. Following tooth extraction, the blood clot forms and defensive cells such as polymorphonucleocytes migrate into the socket to help fight infection. Bundle bone lines the socket with remnants of the periodontal ligament. Coagulate necrosis occurs and a provisional matrix is formed with newly formed blood vessels along with immature collagen fibres. By day seven the bundle bone begins to break down and osteoclastic activity creates gaps within this bone. New blood vessels access the socket and newly woven bone forms around angiogenesis. At day seven to 14 the bundle bone lining is removed 6. By day 14 the bone is more mature. The removal of bundle bone has significant implications for implant stability 2. Bundle bone resorption causes a loss of height and width of buccal bone. Over 12 months it has been shown that 50 per cent of horizontal width of the ridge disappears. Within the first three months two-thirds of that total reduction has already taken place 7.
Biomaterials for socket grafting 8
The choice of bone grafting material should assure the long-term stability of the bone volume and should be based on solid documentation in the literature. There is currently not enough data available to indicate superiority of one method or material over another 9. The complete regeneration of dehiscence and fenestration-type defects cannot be predictably accomplished regardless of which grafting protocol is implemented 1.
- Autograft: Bone from same individual which predictably accelerates new bone formation. Disadvantage is unpredictable resorption and donor site morbidity and resorptive tendency changes with harvesting technique 10.
- Allograft: Bone from same species but another individual. These include free frozen bone, freeze-dried bone allograft, demineralised freeze-dried bone allograft and deproteinised bone allograft. This is an osteoconductive material. Disease transmission has been reported in the past 11.
- Xenograft: Material of biologic origin but another species such as animal, corals or calcifying algae. No reports of disease transmission. Surface characteristics of xenografts are dependent on preparation method. This is an osteoconductive material as all proteins are removed so there is no osteoinductive potential of xenograft materials 12.
- Alloplast: Material from synthetic origin such as calcium phosphates, glassceramics and polymers. The biggest challenge for alloplastic materials has been reproducing the surface characteristics of biologically derived materials. The degradation, however, may be modified according to our clinical indications by changing the material’s chemical structure 12.
Dentists should strive to use a well-documented material with a low substitute rate which results in less horizontal and vertical bone resorption. The use of a barrier membrane is indicated whenever a particulate material is used as it encourages increased bone fill 1. Resorbable collagen membranes such as Jason Membrane demonstrate good cell occlusiveness, good handling properties and have a low susceptibility to complications 13.
- Figure 1 Appropriate asceptic handling of bone substitute materials
- Figure 2 Appropriate pre-planning of a flap design facilitates sufficient access for a socket preservation procedure
- Figure 3 Approximation of tissue with tension-free closure helps prevent infection of grafting materials
- Figure 4 Adequate ridge width, height and buccal contour aids successful osseointegration and patient satisfaction with the aesthetic outcome of dental implant treatment
Socket sealing 14
- Primary closure after elevating and mobilising a full-thickness mucoperiosteal flap
- Free gingival graft – autogenous
- Dermal allografts
- Collagen matrix xenografts.
Socket sealing has shown less horizontal and vertical bone resorption when used with Bio-Oss collagen 15. The ideal healing time before implant placement is reported as being six to nine months to allow for adequate healing of bone substitutes materials 16.
Treatment alternatives 5
Immediate implant placement if intact socket walls, thick facial bone wall, thick gingival biotype, no acute infection and good primary stability
- Early implant placement usually at six to eight weeks in the aesthetic zone
- Conventional implant placement at three months post-extraction
- Socket preservation – in cases where implant placement needs to be delayed due to patient or site related factors. This is beneficial in situations where implant placement needs to be postponed for more than six months.
| Table 1. Alveolar ridge preservation 17 | ||
|---|---|---|
| Horizontal | Vertical | |
| Socket Preservation | 1.31mm | 1.54mm |
| Unassisted socket healing | 1.54mm | 1.12mm |
Is it evidence-based? (Table 1)
Socket preservation does not increase implant survival or success. It has been shown that implant placement is always possible whether the socket has been preserved or not 5. Further bone augmentation has been shown to be needed in 9.9 per cent of socket preserved cases compared with 20.8 per cent unassisted socket healing cases 14. According to the study completed by Mardas socket preservation reduces the marginal bone loss by 0.039mm compared with unassisted socket healing. Autograft results in faster bone healing compared with any other bone substitute material such as Bio-Oss 18. Araujo et al showed significant preservation of the facial bone volume with Bio-Oss Collagen at six months 19. However, socket preservation does not accelerate bone formation.
A CBCT clinical study examining 28 patients with single tooth flapless extractions compared DBBM/collagen grafts versus a blood clot in sockets alone. It was shown that by placing a graft into a socket that the amount of horizontal resorption can be reduced but it will have no impact on the vertical change of the buccal bone wall. Bundle bone on the facial wall resorbs irrespective of ridge maintenance procedures which can have implications in the aesthetic zone. This necessitates a second bone grafting procedure at the time of implant placement 20.
Socket preservation in growing individuals 21
There is limited evidence concerning socket preservation in growing individuals. Sandor completed socket preservation in 21 patients with a mean age of 13 years old. The results of this study showed that 83 per cent of the post-traumatic cases also needed simultaneous grafting with implant placement. Also 6.5 per cent of sockets preserved after the extraction of ankylosed primary molars needed re-grafting.
Conclusions
Most of the resorptive changes of the buccal bone wall have already taken place at eight weeks. Clinical intervention is needed for ridge maintenance as ridge alteration occurs rapidly decreasing its bone volume. Socket preservation results in a greater orofacial dimension of the alveolar ridge that unassisted socket healing.
- Bone substitute materials and/or barrier membranes do not accelerate bone healing in extraction sockets. Implant placement must be delayed for a minimum of six months.
- Socket preservation may be indicated if implant placement has to be postponed for more than six months after tooth extraction.
- No superior technique or biomaterial has been identified. However, a bone substitute material with a low substitute rate is recommended.
About the author
Dr Laura Fee graduated with an honours degree in dentistry from Trinity College, Dublin. During her studies, she was awarded the Costello medal for undergraduate research on cross-infection control procedures. She is a member of the Faculty of Dentistry at the Royal College of Surgeons and, in 2013, she completed the Certificate in Implant Dentistry with the Northumberland Institute of Oral Medicine and has since been awarded the Diploma in Implant Dentistry with the Royal College of Surgeons, Edinburgh. Laura is currently completing the Certificate in Minor Oral Surgery with the Royal College of Surgeons, England. She has also been involved with undergraduate teaching in the School of Dentistry, Belfast where she has an honorary oral surgery contract.
References
1. Chen ST. Clinical and Esthetic Outcomes of Implants Placed in Postextraction Sites. Int J Oral Maxillofac Implants 2009; 24(Suppl):186-217
2. Araujo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 2005 Feb; 32(2): 212-8
3. Chappuis V, Engel O, Reyes M, Shahim K, Nolte LP, Buser D.Ridge alterations post-extraction in the esthetic zone: a 3D analysis with CBCT. J Dent Res 2013 Dec; 92(12 Suppl):195S-201S
4. Clementini M, Tiravia L, De Risi V, De Sanctis M. Dimensional Changes after immediate implant placement with or without simultaneous regenerative procedures: A systematic review and meta-analysis. J Clin Periodontol June 2015 42(7) 599-702
5. Martin WC, Morton D. The Influence of Restorative Procedures on Esthetic Outcomes in Implant Dentistry: A Systematic Review. Int J Oral Maxillofac Implants 2014; 29(Suppl):142-154
6. Cardoropoli G, Araujo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. J Clin Periodontol Sept 2003; 30(9): 809-818
7. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003 Aug; 23(4): 313-23
8. Chen et al. IJOMI 2014, Atieh et al. Ways of keeping enough jaw bone to allow for dental implants after teeth have been taken out. Cochrane Libr Published May 2015
9. ITI Group 1 Consensus Statements: Consensus Statements and Recommended Clinical Procedures Regarding Contemporary Surgical and Radiographic Techniques in Implant Dentistry. Bornstein MM et al. IJOMI 2014
10. Miron RJ, Hedbom N, Saulacic Y, Zhang A, Sculean D, Bosshardt E and Buser D. Osteogenic Potential of Autogenous Bone Grafts Harvested with Four Different Surgical Techniques. J Dent Res 2011 90:1428
11. Boyan BD, Ranly DM, Mc Millan J, Sunwoo M, Roche K et al. Osteoinductive ability of human allograft formulations. J Periodontol 2006;77:1555-1563
12. Jensen SS, Broggini N, Hjorting-Hansen E, Schenk R, Buser D. Bone healing and graft resorption of autograft, anorganic bovine bone and – ticalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clinical Oral Implants Research. 2006; 17(3):237-243
13. Von Arx T et al. Membrane Durabillity and Tissue Response of Different Bioresorbable Barrier Membranes: A Histologic Stucy in the Rabbit Calvarium. Int J Oral Maxillofac Implants 2005; 20:843-853
14. Thalmair T, Hinze M, Bolz W et al. The healing of free gingival autografts for socket-sea; surgery: a case report. Eur J Esthet Dent 2010; 5(4): 358-368
15. Jung RE, Hurzeler MB, Thoma DS, Khraisat A. Local tolerance and efficiency of two prototype collagen matrices to increase the width of keratinized tissue. Journal of Clinical Periodotology 2011; 38(2):173-179
16. Mardas N, Trullenque-Eriksson A, MacBeth N, Petrie A, Donos N. Does ridge preservation following tooth extraction improve implant treatment outcomes: a systematic review: Group 4: Therapeutic concepts and methods. Clin Oral Implants Res. 2015 Sep; 26 Suppl 11:180-201
17. Willenbacher et al. The Effects of Alveolar Ridge Preservation: A Meta-Analysis. Clinical Implant Dentistry and Related Research. Doi:10.111/cid.12364
18. Carmagnola D, Adriaens P, Berglundh T Clin. Healing of human extraction sockets filled with Bio-Oss. Clinical Oral Implants Research 14, 137-143
19. Araujo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clinical Oral Implants Research. 2009; 20(6): 545-549
20. Araujo MG, da Silva JC, de Mendonca AF, Lindhe J. Ridge alterations following grafting of fresh extraction sockets in man. A randomized clinical trial. Clin Oral Implants Res. 2015 Apr; 26(4):407-12
21. Sandor GK, Kainulainen VT, Queiroz JO, Carmichael RP, Oikarinen KS. Preservation of ridge dimensions following grafting with coral granules of 48 post-traumatic and post-extracction dento-alveolar defects. Dent Traumatol. 2003 Aug; 19(4): 221-7
The dental psychological interface
The risk of anti-fungal resistance in dentistry: lessons from a Japanese fungus
Globally since 2009, Candida auris, a fungal species closely related to Candida albicans, has been responsible for a number of… Read more
The anxious patient: Empathy, planning and a team-approach
[ Words: Ilyaas Rehman, BDS (Glas) ] Introduction Introduction This case report documents the treatment provided for a very anxious… Read more
Meaningful milestone
Consultation represents the next step on the journey towards achieving a more effective system of CPD Some dental professionals feel… Read more
Top tips for practicing evidence-based dentistry: Part 3
Introduction Implementing the best available evidence and enabling positive sustainable change in practice is an enviable goal for anyone providing… Read more
The management of a paediatric dental avulsion in general dental practice
Abstract A paediatric dental avulsion is not a clinical scenario that you will be faced with on a daily basis… Read more
Intraoral scanners In dentistry – an update on digital technology
With the introduction of the first intraoral scanner, CEREC (Chairside Economical Restoration of Esthetic Ceramics) by Dentsply Sirona in 1985,… Read more
CBCT and clinical decision-making
Arvind Sharma, BDS(Dund), MSc(Endo), MJDFRCS(Eng), MFDSRCPS(Glas) Arvind Sharma presents the second and final part of a structured critical review to… Read more
Problems of a phobic patient
Day One Ms B attends as a new patient at a local dental surgery complaining of sensitivity in a number… Read more
The power of regeneration
Due to its powerful regenerative properties, platelet rich growth factor Endoret (PRGF) is being increasingly used in many fields of… Read more
Suitability of patients for conscious sedation
Patients suitable to undergo conscious sedation (CS) include those with moderate-severe anxiety, a swallow/gag reflex or a mild learning/physical disability… Read more
Top tips for practicing evidence-based dentistry
In the first article, we explored how to establish a research question using the PICO (Population, Intervention, Comparator and Outcome) method… Read more
Quick, aesthetic restoration
A new patient in her early 30s attended for a check-up. A routine radiograph revealed caries under the amalgam filling… Read more