Periodontitis is a term that refers to a heterogeneous group of diseases characterised by loss of the tooth-supporting tissues. It is well established that periodontal diseases are of an infectious nature and the impact of dental plaque biofilms on the etiology of periodontal diseases has been studied in details. In fact, certain bacterial pathogens are considered to play a significant role in the pathogenesis of periodontitis, formation of the periodontal pocket, destruction of the connective tissue and resorption of the alveolar bone.
Therefore, the primary cause of periodontitis is bacteria, and when the quantitative and qualitative change in bacterial composition in the oral cavity is such that homeostasis cannot be maintained any longer, the host response appears to be impaired and the activity of the tissues become abnormal.
A publication from Hasturk et al. (2007) outstandingly defined the possible pathogenesis of the periodontal infections; in fact, Hasturk and co-workers suggested that while the etiology of periodontitis is bacteria, the pathogenesis is inflammatory.
In other words, the interaction between the pathogenic bacteria and the host’s defence system could lead to the development of an inflammatory process.
Once periodontitis is established, the inflammatory infiltration of periodontal tissues is composed of different immunological cell types. These cells produce a large repertoire of specific types of cytokines and chemokines, which could play a significant role in the pathogenesis of periodontitis. Some of these, together with the end products of periodontal tissue destruction, could act as possible biomarkers and eventually could have diagnostic value by identifying patients with enhanced disease susceptibility and sites with active disease. They could also serve as surrogate end points for the monitoring of the patient treatment effects and treatment status, to tailor the maintenance care based on the biological needs of the subjects.
These biological mediators could support the clinical measurements already used in the routine diagnosis of periodontal diseases such as probing pocket depth, bleeding on probing, clinical attachment levels, plaque index and radiographs quantifying alveolar bone level. Nevertheless, they are often of limited usefulness because they are indicators of previous periodontal disease rather than the present disease activity. In addition, current periodontal examination procedures performed at single visit cannot determine whether or not sites are currently undergoing additional attachment loss.
As various immunopathogenic mechanisms are involved in the disease process of periodontitis, a combination of indicators is needed to improve the specificity of periodontal disease diagnosis. On the basis of the current understanding of the complexity of periodontitis, the identification of one single diagnostic marker for all forms of periodontal disease seems illusionary.
Nevertheless, researchers have been searching actively for unequivocal markers of periodontitis in different biological sources such as blood or serum, subgingival plaque sample, gingival crevicular fluid (GCF) and saliva to develop a simple test, to be used as chairside test or home-use device, to determine whether a patient suffers from periodontitis and needs therapy, as opposed to another patient who needs no intervention even though he/she has gingivitis and/or to establish a “custom-made” frequency of recall appointments.
The aim of this literature review is to summarise data from the literature on periodontal disease markers with special focus on saliva.
Saliva and candidate biomarkers of periodontal diseases
Saliva is a mirror of the body that contains a large number of proteins and peptides that are responsible for maintaining the integrity of the oral cavity (see table opposite page).
Saliva also meets the demand for inexpensive and easy-to-use diagnostic aids due to the non-invasive and simple nature of its collection. It can be collected with or without stimulation. The collection of gland specific saliva (from parotid, submandibular and sublingual gland) can allow differences in the amount of fluid and constituents of each gland to be determined. Differently, whole saliva consists of a mixture of oral fluids, and includes secretions of the major and minor salivary glands and constituents of non-salivary origin, such as derivates from GCF, serum and blood cells in case of bleeding gingiva or oral wounds, and expectorated bronchial secretions. It might also contain bacteria, bacterial products, viruses, fungi, desquamated epithelial cells and food debris.
The use of saliva for diagnosis of periodontal disease activity has been the subject of considerable research activity; in fact, it contains locally and systemically derived markers of periodontitis, thus offering the basis for a specific test. Several potential markers have been investigated to produce an assay system suitable for use in dental practices.
The main candidates in the search for biomarkers of periodontal disease activity fall into different general categories:
- Inflammatory and immune products
- ost-derived enzymatic and non-enzymatic proteins
- 3 Connective tissue degradation products
- 4 Products of bone resorption
- 5 Human salivary proteome and transcriptome
- 6 Substances associated with putative pathogens.
Inflammatory and immune products
While the bacterial infection triggers the destructive process, the host immune response to the bacterial challenge is responsible for the molecular processes leading to periodontal tissue destruction. The interaction between the pathogenic bacteria and their (toxic) components and the host defence system could lead to the development of periodontal pockets, loss of connective tissue, and bone resorption. Once periodontitis is established, the inflammatory infiltration is composed of different cell types, such as neutrophils, T and B lymphocytes, and macrophages migrating into the perivascular connective tissue.
The substances released by the inflammatory immune cells as well as by resident fibroblasts endothelial cells and others during the disease process include a large repertoire of molecules, such as antibodies, complement proteins, acute phase proteins and a broad range of inflammatory mediators (i.e. cytokines, chemokines, arachidonic acid metabolites etc.).
A recent investigation found that salivary level of MIP-1α was significantly correlated with Aggregatibacter actinomycetemcomitans positive students who developed periodontal disease six to nine months before radiographic detection of bone loss. MIP-1α level was also significantly associated with increasing probing depth and the number of pockets > 6mm (Fine et al. 2009).
Host-derived enzymatic and non-enzymatic proteins
Non-enzymatic proteins have been examined in a number of studies to investigate whether or not there was a relation between periodontal disease and these proteins in saliva. For example, platelet-activating factor (PAF), a potent phospholipid inflammatory mediator, was identified in the mixed saliva of subjects with periodontal disease. Salivary PAF levels have been found to be significantly higher in untreated chronic periodontitis patients compared to controls (Garito et al. 1995). Its levels correlate with clinical indices of disease severity and extent of the disease. Furthermore, a longitudinal evaluation of the effect of periodontal therapy on salivary PAF levels in chronic adult periodontitis patients was studied and initial salivary PAF levels were found to be decreased following supragingival plaque control and further reduced following scaling and root planning (Rash et al. 1995).
Saliva contains also numerous enzymes that degrade proteins, proteoglycans, lipids and carbohydrates. Enzymes in saliva can originate from GCF, salivary glands, microorganisms, epithelial cells and polymorphonuclear leukocytes (PMNs). PMNs are an important cell type in host defense against periodontopathogenic bacteria. Their primary role of phagocytosis of microorganisms may promote local tissue destruction by the release of tissue-degrading enzymes. In fact, PMNs granules contain hydrolytic neutral enzymes, such as elestase, cathepsin B, cathepsin D, glucuronidase. Matrix metalloproteinases (MMPs), peroxidase, lysozyme, lactoferrin, and many other enzymes are also sheltered in PMNs granules. Some of these are now discussed below.
MMPs represent a neutrophil granule content, which are involved in many biological processes, including the tissue destruction in periodontitis. MMPs degrade mostly components of the extracellular matrix (ECM) and many non-ECM molecules. The major MMPs in neutrophils are MMP-8 and -9 and these are the main collagen-degrading enzymes in saliva. Since MMPs can potentially cause tissue damage, their activity is controlled by four members of the tissue inhibitor of metallo-proteinase family (TIMP). The presence of MMPs in saliva has been studied comprehensively with ELISA techniques. The levels of MMP-1, -3, -8 and -9 and their endogenous inhibitor, TIMP-1, in saliva of patients with adult periodontitis were compared to localised juvenile periodontitis and controls. Both MMP-1 and TIMP-1 were detected in all studied saliva samples, but interestingly no significant differences were detected between adult periodontitis and healthy control groups (Ingman et al. 1996).
Antioxidant activity and capacity
PMNs and macrophages produce reactive oxygen species (ROS) within their phagolysosomes and these may spill over into the tissues during phagocytosis or when they degenerate. This may cause bystander tissue damage around these cells. ROS have a great capacity to damage cells and tissues and are scavenged for within the tissues by antioxidants.
The antioxidant capacity of saliva has been investigated in healthy and chronic periodontitis patients. The major aqueous antioxidant component of whole saliva was found to be uric acid with lesser contributions from ascorbic acid and albumin. Using biochemical methods, the antioxidant capacity of the saliva was not found to be compromised in chronic periodontitis patients, and this was attributed to increased salivary flow and antioxidant flow from GCF.
Another research group investigated pheripheral (serum) and local (saliva) total antioxidant (TAO) capacities of chronic periodontitis and healthy patients using an enhanced chemiluminescent assay (Chapple et al. 1997). There were no differences in the serum TAO capacities but the salivary TAO capacities were significantly lower in the chronic periodontitis group compared with the healthy group. Thus the saliva of chronic periodontitis patients may have reduced TAO capacity, which could result from increased ROS production by inflammatory cells. The enhanced chemiluminescent assay provides a rapid simple method of measuring the total antioxidant defense in small volumes of biological fluid and hence could have diagnostic use. More work on its relationship to the progression of periodontal disease, and its capacity as biomarker needs to be done before this could be properly assessed.
Another enzymatic category, which has received the attention of periodontal researchers, is represented by enzymes released by dead cells (cytosolic enzymes). Aspartate amino transferase (AST) and lactate dehydrogenase (LHD) are soluble cytoplasmic enzymes that are confined to the cell cytoplasmic enzymes, and they can be released by dead or dying cells. Since cell death is an integral and essential component of periodontal tissue destruction, these enzymes should be released during this process and should pass with the inflammatory exudates into GCF and saliva.
While we do not have relevant studies on AST in saliva, a recent report demonstrated an increased LDH salivary activity in association with periodontal disease, specifically with the presence of calculus and pockets greater than 5mm (de La Peña et al. 2007). Clearly these markers are yet to be further investigated for their potential as salivary biomarkers for periodontitis.
Of the potential markers, PMNs-derived enzymes appear to be worthy of further study. The concentrations of host-derived elastase, chitinase and -glucuronidase are increased in patients with periodontitis and decrease following therapy (Lamster et al. 2003).
However, at the present state of knowledge, their salivary levels are not predictive of disease activity, which is the basic requirement of a diagnostic test.
About the author
Dr Fabiano Galassi D.D.S. M.Sc. (ACTA) Periodontology and Implant Dentistry. Practice limited to periodontology and implant dentistry. He received his Dental Degree from “La Sapienza” University of Rome. After two years general practice, he moved to Dublin where he continued working as a general practitioner until 2008.
Dr Galassi graduated with Honours from the MSc programme in Periodontology and Implant Dentistry at the Academic Center for Dentistry in Amsterdam (ACTA), in 2011. Has great interest in dental research, and he has published in peer-reviewed journals and written some chapters for periodontology textbooks.
As a member of the European Federation of Periodontology (EFP) and the Italian Federation of Periodontology (SIdP) Dr Galassi is now working at the Seapoint Clinic and Gleville Dental and his focus is on the treatment of periodontal disease, bone regeneration, cosmetic periodontal plastic surgery and implant dentistry.
References
Chapple, I.L., Mason, G.I., Garner, I., Matthews, J.B., Thorpe, H.G., Maxwell, S.R., & Whitehead, T.P. (1997). Enhanced chemiluminescent assay for measuring the antioxidant capacity serum, saliva, and crevicular fluid. Annals of Clinical Biochemistry 34, 412-421.
- de La Peña, V.A., Diz Dios, P. & Tojo Sierra, R. (2007). The relationship between lactate dehydrogenase activity in saliva and oral health status. Archive of Oral Biology. 52, 911-915.
- Fine, D.H., Markowitz, K., Furgang, D., Fairlie, K., Ferrandiz, J., Nasri, C., McKieran, M., Donnelly, R. & Gunsolley J. (2009). Macrophage inflammatory protein-1α: a salivary biomarker of bone loss in a longitudinal cohort study of children at risk for aggressive periodontal disease? Journal of Periodontology 80, 106-113.
- Garito, M.L., Prihoda, T.J. & McManus, L.M. (1995). Salivary PAF levels correlate with the severity of periodontal inflammation. Journal of Dental Research 74, 1048–1056.
- Hasturk, H., Kantarci, A., Goguet-Surmenian, E., Blackwood, A., Andry, C., Serhan, C.N. & Van Dyke, T.E. (2007). Resolvin E1 regulates inflammation at the cellular and tissue level and restores tissue homeostasis in vivo. Journal of Immunology 179, 7021-7029.
- Ingman,T., Tervahartiala, T., Ding, Y., Tschesche, H., Haerian, A., Kinane, D.F., et al. (1996). Matrix metalloproteinases and their inhibitors in gingival crevicular fluid and saliva of periodontitis patients. Journal of Clinical Periodontology 23, 1127-1132.
- Lamster, I.B., Kaufman, E., Grbic, J.T., Winston, L.J. & Singer, R.E. (2003). Beta-glucuronidase activity in saliva: relationship to clinical periodontal parameters. Journal of Periodontology 74, 353–359.
- Rasch, M.S., Mealey, B.L., Prihoda, T.J., Woodards, D.S. & McManus, L.M. (1995). The effect of initial periodontal therapy on salivary platelet-activating factor levels in chronic adult periodontitis. Journal of Periodontology 66, 613–623.
Patients suitable to undergo conscious sedation (CS) include those with moderate-severe anxiety, a swallow/gag reflex or a mild learning/physical disability such as cerebral palsy. Well-controlled medical conditions such as asthma, epilepsy, gastro-oesophageal reflux and mild hypertension are exacerbated by stress, making CS hugely beneficial. 1
Hospital-based intravenous (IV) CS helps patients with severe systemic disease or disability to avoid unnecessary general anaesthesia (GA). However, a small percentage of patients will still simply not tolerate dental treatment without being ‘knocked out’, making GA essential to facilitate dental treatment.
An in-depth medical, dental and social history is mandatory at a visit before treatment. It is important to ascertain the patient’s degree of dental anxiety. This helps determine the most suitable sedation technique as some patients with severe needle phobia are unable to tolerate cannulation making inhalation sedation the best option for them.2
General health considerations
ASA Physical Status Classification3
- ASA 1 – Heathy person – suitable for IV/inhalation sedation
- ASA 2 –Patient with mild systemic condition – mild disease with minimum functional limitation – generally suitable for IV/inhalation sedation in primary care
- ASA 3 – Patient with severe systemic condition – significant functional limitations such as with COPD – may be suitable for inhalation sedation in primary care, but otherwise careful evaluation for hospital-based sedation
- ASA 4 – severe systemic disease constantly threatening life – myocardial infarction or stroke <six months ago – anaesthetist-led team
- ASA 5 – Moribund.
Age
Age is not an absolute contraindication to sedation but older patients are more sensitive
to sedatives.4 The incidence of delirium following treatment with midazolam was 10 per cent higher in the elderly.5 Elderly patients also tend to have poorly tethered, friable veins, which may be more susceptible to cannulation damage. IV sedative agents in children <12 is not recommended unless provided by a paediatric specialist. Disinhibition in adolescents is common and even slight over-sedation can lead to rapidly deteriorating respiratory depression.6
Cardiovascular System
There should be no elective surgery if the diastolic value is >110 mmHg. However, when measuring blood pressure always consider the risk of “white coat hypertension”.
Patients with controlled/uncontrolled hypertension have a more labile haemodynamic profile during CS making hypotensive swings more likely.7
It has been shown that there is little evidence that a BP < 180mmHg/110mmHg causes perioperative complications. However, a BP>180/110mmHg is linked to perioperative ischaemia, arrhythmias and cardiovascular lability. There is no clear evidence that deferring anesthesia lowers perioperative risk. The intraoperative BP should be within 20 per cent of best BP estimate.8
Dentists must evaluate pre-operatively for the presence of target organ damage such as coronary artery disease. Target organ damage lowers the treatment thresholds for raised BP.9
A study examining the cardiovascular effects of epinephrine with IV midazolam examined 75 patients with heart disease treated in two groups.The rate-pressure product (RPP) was used to indicate myocardial ischemia. This is the systolic BP x heart rate = RPP, which is a reliable indicator of myocardial oxygen consumption. Ischemic changes were demonstrated in patients with an RPP of >12,000, increasing their CS risk. The pressure rate quotient, which is mean BP divided by heart rate, also assesses a patient’s suitability for CS. The results of this study indicated that treatment with midazolam and epinephrine does not generate significant ischemic risk. It is important that the lowest effective dose of local anaesthetic containing epinephrine is used and that intravascular injections are avoided.10
| Cardiovascular system ASA According to Blood Pressure (BP): |
||
|---|---|---|
| <140 systolic and <90 diastolic | ASA I | Primary care suitable |
| 140-160/90-94mmHg | ASA II | Primary care suitable |
| 160-199/95-115mmHg | ASA III | Specialist unit |
| 200 systolic and >115 diastolic | ASA IV | In-patient services |
NYHA classification of angina
0 Healthy
1 No hindrance to normal physical exertion
2 Slight limitation, angina with fast walking, ascending stairs, excitement
3 Significant limitation of regular movement. Angina on climbing a normal staircase
4 Angina with minimal activity/rest.
Increased stress levels exacerbate angina, making sedation and good local anaesthesia important in reducing heart rate. Unstable angina contraindicates elective treatment. Patients with angina that affects normal daily activity such as NYHA 3 are unsuitable for sedation in primary care. If the GP/cardiologist confirms stability of angina then NYHA 2 patients can progress with elective sedation.11
Post MI
At six months post-infarctiona patient is classed as ASA 3. The risk of re-infarction is 16 per cent. Elective sedation in well-controlled patients reduces stress, helping to lower risk.
Post-percutaneous coronary intervention (PCI)
Patients must wait three months after stenting before elective sedation. Angina must always be successfully controlled before treatment.1
Classification of cardiac functional reserve capacity
- Class 1: Able to climb a normal flight of stairs without stopping. Can continue walking with no rests – safest for IV CS
- Class 2: Climbs without rest. Rests on top – safest for IV CS
- Class 3: Climbs with rest during ascent – outpatient CS unsuitable
- Class 4: Unable to climb stairs.
Patients with palpitations
Patients with benign palpitations benefit from the stress reduction produced by CS. A patient with malignant palpitations, however, must be treated in hospital. Any individual with an automated implantable cardioverter-defibrillator is unsuitable for treatment in primary care. A hospital setting is mandatory for patients with a pacemaker or those following AV node/conduction pathway ablation surgery. Wolff-Parkinson-White syndrome is an absolute contraindication to sedation.1
Respiratory disease
Midazolam has a greater effect on the respiratory system compared to the cardiovascular system. Healthy patients who present with respiratory infections on the day of treatment should be rescheduled. Careful assessment of the patient’s disease and functional reserve will indicate the most suitable setting for CS. It must be remembered that opioids act synergistically with sedation with regards to respiratory depression.12
Dyspnoea grading system12
0 Healthy
1 Mild dyspnoea
2 Moderate – limited outdoor movement – hospital management safest
3 Marked dyspnoea on minimal exertion indoors – unsuitable for outpatient sedation
4 Dyspnoea while resting – unsuitable for outpatient sedation.
Asthma
The dentist must ensure the asthmatic is well controlled. A mild asthmatic is considered ASA 2; however, an untreated Grade 2 is unsuitable for treatment in primary care. Hospital management is necessary for ASA 3 patients who have frequent episodes/attacks. It must be borne in mind that theophylline can interact unfavourably with IV midazolam. Inhalation sedation can be a safer option due to guaranteed oxygen levels.13
COPD
Extreme caution is needed with COPD patients who suffer with emphysema or bronchitis. A patient with chronic bronchitis is ASA 3. Midazolam results in dose-related respiratory depression, which is more exaggerated in COPD patients. Hospital treatment of the patient in an upright position with supplemental oxygen is required due to the increased risk of hypoxia.
If a patient needs supplemental oxygen at home or has severe orthopnoea or a productive cough then sedation is contraindicated.12
Renal system impairment
Hepatic microsomal oxidation is responsible for midazolam’s biotransformation. This is susceptible to factors such as old age, hepatic cirrhosis and drugs (cimetidine) as they reduce the oxidative capacity. A high regular intake of alcohol increases midazolam clearance.
Renal failure causes a build-up of metabolites which prolongs sedation. CS is contraindicated in cases of advanced liver disease.1
Patients undergoing haemodialysis or continuous ambulatory peritoneal dialysis are unsuitable for sedation.
Haemodialysis patients swing from being centrally underfilled where they are at risk of hypotension to centrally overfilled. Day 2 is considered the safest time to treat but outpatient CS is still best avoided. Post-renal transplant patients with good renal function may be suitable for hospital-based CS.11
Methadone and midazolam are both metabolised by the cytochrome P450 3A pathway. Chronic methadone use leads to the induction of this pathway with more rapid midazolam metabolism and higher dosage requirements.14
Neurological disease
IV midazolam helps to reduce involuntary movement in patients with multiple sclerosis and Parkinson’s disease making dental treatment more comfortable. Many patients will have reduced swallowing capacity so sitting the patient upright with adequate suction is vital. Controlled epileptics are suitable for CS although more research is needed to develop clearer guidelines. Liaising with the GP/neurologist confirms if the patient has a driving licence and when the last three seizures occurred. Anti-epileptic drugs such as phenytoin can increase or decrease plasma concentration of sedatives.11
Recovered stroke victims may experience a re-emergence of symptoms when benzodiazepines are administered. Light sedation can trigger a re-occurrence of symptoms such as right-sided paralysis and dysphasia. Sedation is contraindicated for one year after a stroke.15
Haematological disorders
Sedation should be avoided in patients with sickle cell anaemia and thalassaemia. This cohort are high risk for reduced oxygen tension with respiratory depression or over-sedation. Inhalation sedation is preferred.16
Pregnancy
The second trimester is the safest time to treat, but the mother’s metabolism is altered due to the increased demands of the baby. This makes sedation unpredictable. There are also foetal teratogenic risks.12
Intellectual or physical impairment
Patients with mild learning disabilities are suitable for sedation. Severe learning or physical difficulties require management by an anaesthetist-led team.17
Endocrine diseases
Diabetes
HbA1c helps identify pre-diabetic patients. It also helps recognise diabetics at risk of complications. A BM check of >5mmol/l pre-treatment is advisable.18
Pre-operative starvation can upset blood sugar levels. The evidence for fasting is low so a degree of clinical judgement required.19 Well-controlled diabetics are best treated in the morning to avoid interference with their insulin routine. Poorly controlled diabetics requires hospital management. Inhalation sedation can be a safer option as it is easily reversible.16
Adrenal insufficiency
Patients on long-term steroids must be treated in an anaesthetist-led facility to avoid an adrenal crisis.13
Thyroid disease
Hyperthyroidism can cause tachycardia and atrial fibrillation. Hypothyroidism can cause bradycardia, making CS unpredictable.12
Specific drug considerations
Cardiac medication: Ace inhibitors, beta blockers, calcium channel blockers and nitrates enhance the hypotensive effect of midazolam20
Erythromycin effects metabolism of midazolam21
Midazolam interacts with herbal medicine potentiating CNS depression22
Opioids such as heroin can cause significant respiratory depression with midazolam. Veins are often unusable1
Cocaine adversely effects respiratory/cardiovascular control with sedation1
Cannabis makes oxygen saturation levels unpredictable during sedation1
Central nervous system depressants for mental health conditions can act synergistically with benzodiazepines. Tolerance may have developed in these patients similar to recreational drug users.20
Assessment of vital signs
Blood pressure, oxygen saturation, BMI, heart and respiratory rate must provide a satisfactory baseline indicating fitness for sedation. Sometimes a screening may reveal an unknown condition requiring further investigation by a GP before sedation can be performed.16 It is important to predict a patient’s risk for conscious sedation. Hospital-based sedation is advisable in the following instances:
- Baseline SaO2 is <95 per cent
- Patients with respiratory disease such as COPD
- Patients classified as ASA 3-4
Patients with a history of more than one attempt for previous intubation.23
BMI
A patient with a BMI of <35kg/m2 is suitable for primary care CS. Caution is advised with a BMI of 35-40kg/m2 especially if the patient has co-morbidities such as hypertension and diabetes.
The standard dental chair has an upper weight limit of 140kg making referral to hospital sometimes necessary for the use of a DIACO chair which can hold 500kg. Successful cannulation can be difficult due to the effects of increased adipose tissue on vein morphology.24
Sleep apnoea is more common in individuals with a BMI of >35. Sedation is an absolute contraindication in patients with obstructive sleep apnoea(OSA). The pharyngeal airway dilator muscles are highly sensitive to benzodiazepines.25 The STOP-BANG questionnaire is a useful screening tool for identifying potential cases of OSA.26
Malampatti system
This is a visual assessment of the distance from the base of the tongue to the soft palate. A Class 3 or 4 patient is at increased risk of airway obstruction. The patient must be asked to protrude their tongue. It is important to document the level of visibility of the back of the mouth.27
A difficult airway can also be judged if the thyromental distance is <6.5cm. A short, fat neck and receding jaw is an airway risk. Males are more susceptible to airway obstruction.28
Indications for inhalation sedation (IS)
IS can be used from the age of three. 29 Patients who are allergic to benzodiazepines or those tolerant to them due to treatment for anxiety/insomnia are suitable for IS. In patients previously addicted to benzodiazepines IV, CS can reactivate dependence making inhalation sedation safer.30
Contraindications to IS
IV sedation suits mouth-breathers, anyone taking methotrexate due to the anti-folate effects of IS and also someone who had vitreoretinal surgery within 12 weeks. Severe autism or ADHD patients are unsuitable for IS due to compliance difficulties. A hearing impediment reduces the hypnotic suggestion aspect of IS treatment making CS more effective.16
Non-titratable sedation techniques
If titratable techniques are deemed inappropriate then oral or intranasal sedation may be considered. Special care dental patients with challenging behaviour benefit greatly from these advanced techniques.31
Conclusion
A treatment plan is devised by combining the information gathered during history-taking and the clinical exam. The patient must be of sound mind to give their valid written consent at a visit separate to treatment. If needed, the presence of a responsible adult escort must be possible.32 Careful consideration regarding the nature of the patient’s disease and functional capacity is essential. The dentist has a duty of care to predict patients at risk of complications with CS such as cardiac, respiratory or neurological deterioration. After risk stratification, the optimum timing and setting for treatment must be decided to ensure patient safety.
There will always be a place in dentistry for general anaesthesia, especially for treatment plans involving extensive work on multiple teeth that make multiple sedation visits impractical and overall more expensive. Also in certain sedation cases, patients can move unpredictably, compromising the quality of the dentistry performed, which may necessitate the use of general anaesthesia.
References
- Stoelting, R.K. (2015) Pharmacology and Physiology in Anesthetic Practice. 5th edn. Philadelphia, Lippincott Williams & Wilkins.
- Standards for Conscious Sedation in the Provision of Dental Care; Report of the Intercollegiate Advisory Committee for Sedation in Dentistry. (IACSD). 2015.
- ASA http://www.asahq.org/ accessed 19/12/17.
- Yano H, Iishi H, Tatsuta M, Sakai N, Narahara H, Omori M. Oxygen desaturation during sedation for colonscopy in elderly patients. Hepatogastroenerology 1998 Nov-Dec; 45(24): 2138-41
- Weinbroum AA, Szold O, Ogorek D, Flaishon R. The midazolam-induced paradox phenomenon is reversible by flumazenil. Epidemiology, patient characteristics and review of the literature. Eur J Anaesthesiol 2001 Dec; 18(12): 789-97.
- Wilson KE, Thorpe RJ, Mc Cabe JF, Girdler NM. Complications Associated with IV Midazolam Sedation in Anxious Dental Patients.Primary Dental Care 2011:18(4):161-166
- European Society of Hypertension(ESH) and of the European Society of Cardiology(ESC).Guidelines for the management of arterial hypertension. Journal of Hypertension 2013, 31(7), 1281-1357.
- Fleisher LA et al. AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Non-cardiac Surgery. Journal of American College of Cardiology 2007 Volume 50, Issue 17: e242.
- Howell SJ, Sear JW, Foex P. Hypertension, hypertensive heart disease and perioperative cardiac risk. British Journal of Anaesth 2004 92(4): 570-83
- Middlehurst R, Coulthard P. The effect of midazolam sedation on indicators for myocardial ischemia. Oral Surg Oral Med Oral Pathol, Oral Radiol-Endod Oct 1999;88(4):400-5.
- Malamed S.F. (2010) Sedation: A Guide to Patient Management. St Louis, Mosby.
- Hines RL, Marschall KE. Stoelting’s Anesthesia and Co-existing disease. 7th edition Elsevier.
- Royal College of Surgeons of England (2013) Safe Sedation Practice for Healthcare Procedures: Standards and Guidance. London, The Academy of Medical Royal Colleges.
- Rab-Khan A, MacLeod D, Prichard JS. Marked increase in benzodiazepine requirements during bronchoscopy in HIV positive intravenous drug abusers. Ir Med J. 1992 Mar; 85(1): 37-8.
- Lazer RM, Fitzsimmons BF, Marshall RS, Mohr JP, Berman MF. Midazolam challenge re-induces neurological deficits after transient ischemic attack. Re-emergence of stroke deficits after Midazolam challenge. Stroke 2003 Mar; 34(3): 794-6.
- N.M. Girdler, C.M.Hill, K.E.Wilson. Conscious Sedation for Dentistry. Wiley Blackwell. Second Edition.
- Scottish Government(2000) Adults with Incapacity(Scotland) Act 2000. Online at: www.legislation.gov.uk (accessed Dec 15, 2017).
- www.diabetes.co.uk accessed 22nd Dec 2017
- Conscious Sedation in Dentistry. Dental Clinical Guidance. Scottish Dental Clinical Effectiveness Programme. June 2017.
- Tang DM, Simmons K, Friedenberg FK. Anti-hypertensive therapy and risk factors associated with hypotension during colonoscopy under conscious sedation. J Gastrointestin Liver Dis. 2012 Jun; 21(2): 165-170.
- Drugwise.org.uk accessed 02/01/2018.
- Tweddell P, Boyle C. Potential Interactions with herbal medicines and midazolam.Dental Update April 2009 Apr; 36(3): 175-8.
- Lazzaroni M, Bianchi-Porro G. Premedication, preparation and surveillance. Endoscopy 1999 Jan; 31(1): 2-8.
- WHO http://apps.who.int/bmi/index.isp?introPage=intro 3.html accessed 28/12/17.
- Reilly D, Boyle CA, Craig DC. Obesity and dentistry: a growing problem. Br Dental J 2009 Aug 22: 207(4):171-5.
- Chung F, Abdullah HR, Liao P. STOP-BANG Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Anesthesiology 2008;108: 812-21.
- Mallampati S.R., Gatt S.P., Gugino, L.D., Desai, S.P., Waraksa, B., Freiberger, D. and Liu, P.L. A clinical sign to predict difficult tracheal intubation: a prospective study. Canadian Anaesthetists’ Society Journal 1985; 32(4). 429-434.
- Samsoon GLT, Young TRB(1987). Difficult tracheal intubation: a retrospective study. Anaesthesia 42: 487-490.
- Wilson, K.E.(2013) Overview of paediatric dental sedation: 2. Nitrous oxide/oxygen inhalation sedation. Dental Update. 40, 822-829.
- Blain K.M.& Hill, F.J.(1998) The use of inhalation sedation and local anaesthesia as an alternative to general anaesthesia for extractions in children. British Dental Journal, 184(12), 608-611.
- Manley, M.C., Ransford, N.J., Lewis, D.A., Thompson, S.A. & Forbes, M. Retrospective audit of the efficacy and safety of the combined intranasal/intravenous sedation technique for the dental treatment of adults with learning disability. British Dental Journal 2008 205(2): E3; 84-85.
- Johnston C&Liddle, J. The Mental Capacity Act 2005: a new framework for healthcare decision making. Journal of Medical Ethics 2007; 33(2), 94-97.
About the author
Dr Laura Fee graduated with an honours degree in dentistry from Trinity College, Dublin, where she was awarded the Costello medal for undergraduate research on cross-infection control procedures. She is a member of the Faculty of Dentistry at the Royal College of Surgeons. She has a Certificate in Implant Dentistry from Northumberland Institute of Oral Medicine and has been awarded the Diploma in Implant Dentistry with the Royal College of Surgeons Edinburgh.
In the first article, we explored how to establish a research question using the PICO (Population, Intervention, Comparator and Outcome) method and discussed the hierarchy of evidence. At this point in the search for evidence to support our practice, we know the question we need answered and also understand how different types of research can help to answer our questions.
We now need to think about where to find the evidence and how to assess the quality of what we find.
First let’s revisit the five steps to an evidence-based approach.
Establishing an evidence-based approach has five steps
- Asking answerable questions (ASK)
- Searching for the best evidence (AQUIRE)
- Critically appraising the evidence (APPRAISE)
- Applying the evidence (APPLY)
- Evaluating the outcome (ASSESS).
This article will explore points 2 and 3 of establishing an evidence-based approach to healthcare.
Question 2: Searching for the best evidence (AQUIRE)
The search for evidence
There are a number of databases that can be used to find the evidence. Which database you choose to search depends on what type of resource or evidence you require. In this section, we will introduce and explore the use of databases that host most of the information required in day-to-day practice. Three of the most commonly used databases are included in Table 1.
There are other databases available for searches of more specific topics that can be accessed through the knowledge network; for example, PsychINFO is a good database to search for psychology and behavioural science-related topics. You can see the full list of databases on offer here: www.knowledge.scot.nhs.uk
| Database | Type of evidence | Key features |
|---|---|---|
| PubMed | Systematic Reviews, Primary Research | Ability to create an account and save search results for later use |
| Cochrane Library | Systematic Reviews | Includes plain language summaries of reviews; useful for translating evidence for use at chair side |
| TRIP | Guidelines, Systematic Reviews, Primary Research | Displays results in the style of hierarchy of evidence, reducing search time |
Searching for systematic reviews and guidelines
It is always a good idea to start your search for evidence at the top of the evidence pyramid. As we discussed previously, systematic reviews and randomised control trials are the level of evidence we would require in order to think about changing our practice. At the end of our first article, we briefly discussed guidance documents. The guidance produced by SDCEP, NICE and SIGN are all evidence-based and the groups will have come to their recommendations after a thorough process.
SDCEP methods
Dr Doug Stirling is Programme Manager of the Guidance Development Group, Scottish Dental Clinical Effectiveness Programme, NHS Education for Scotland. Here he tells us more about the work of the SDCEP team and the methods they use.
Who is involved in guidance development? What is the skill mix in a guidance team?
The SDCEP team operates within NHS Education for Scotland’s Dental Directorate. Each guidance project is assigned an SDCEP project lead, who manages the project and is responsible for the methodology employed, and an administrator who helps to co-ordinate the project. For each project we also convene a Guidance Development Group comprising external individuals who are representatives of groups with a particular interest in the topic. Typically this will include various relevant branches of the dental profession and patients, and may also include other healthcare discipline relevant to the topic.
How rigorous is the process of appraising the evidence?
Each guidance project aims to answer a number of questions. SDCEP identifies the latest evidence that is relevant to these questions, focusing on systematic reviews and other evidence-based guidelines. To assess the quality of evidence in systematic reviews, SDCEP now uses GRADE (Grading of Recommendations, Assessment, Development and Evaluation), which is a widely accepted system for grading both evidence and recommendations in clinical guidelines. More information on the GRADE system can be found at www.gradeworkinggroup.org
We appraise guidelines using the AGREE II checklist, again an internationally recognised tool for assessing guideline quality and reliability. Find out more at www.agreetrust.org
Recommendations in SDCEP guidance result from a rigorous consideration of not only relevant research evidence, but also other factors, including, the balance of risks and benefits, patient’s views and preferences, practitioner perspectives and the practicalities.
The process SDCEP uses to develop its guidance has now been accredited by NICE (the National Institute for Health and Care Excellence), which should give users added confidence in the reliability of the guidance as an aid to their decision-making.
How does the SDCEP guidance apply to a general dental practitioner?
The vast majority of dental care is delivered in primary care practice. Recognising this, most SDCEP guidance is primarily directed towards dentists and their teams working in general dental practice. However, the guidance is also likely to be of interest to those in training, dental educators, and secondary care and public health practitioners.
Do we always need to follow the guidance?
Healthcare staff have the right, and indeed the duty, to make decisions that are in the best interests of their patients with their consent. SDCEP guidance is provided to inform some of these decisions. There is no obligation to follow a recommendation in the guidance if a health professional feels that it is in the best interests of an individual patient not to do so.
However, it would be advisable to document a departure from recommended practice in the patient’s clinical notes, including the reason for this.
Further information about SDCEP guidance development: www.sdcep.org.uk/how-we-work/ or to find out more about GRADE
TRIP database

TRIP (Translating Research Into Practice) is a useful resource for searching for the results of systematic reviews, randomised controlled trials and guidelines. You might think of it as a high-quality Google for health-care research. It is an online database that has a few very useful search tools. You can do a single-word search, which is similar to a Google search, but you can be more specific and use the search function established around a PICO question. Shown in Figure 1 below. The database displays results and categorises the level of evidence in a hierarchy. It is similar to the hierarchy of evidence discussed in the first article. This makes it easy to identify what type of evidence the study is before you spend time reading it.
Searching for journal articles
TRIP will also produce results from primary research but another useful database that you should understand how to use is PubMed.
PubMed is a search engine that searches the online database MEDLINE. It includes more than 27 million records. Here you will find a range of evidence. As we demonstrated in the first article, the results can be confusing at first and the searches can result in a lot of irrelevant material. We will discuss how best to use the search function later but will first look at the fundamentals of searching scientific databases.
PubMed can be accessed by typing ‘pubmed’ into any search engine or by visiting www.ncbi.nlm.nih.gov/pubmed
Free text searching and Boolean connectors
Having a systematic approach to your search will make finding relevant papers a lot easier and quicker. Most of the pointers demonstrated in this section can be broadly applied in other online searches.
You could decide to free text the search tab as you might use a search engine such as Google. This approach can often result in a large amount of unfiltered results, similar to a search for a hotel room without any information on location, standard or length of stay.
If you know the title of the exact paper you are looking for, then you could simply type this into the search box at the top of the page. You can tailor the search; for example, if you only have some of the information about a specific paper, such as the author.
A better way to search, and the best way to get the most out of the search engines, is to use Boolean search methods.
This approach still uses free text in the search but introduces AND, OR and NOT. The AND, OR and NOT are known as Boolean connectors. They all have specific functions and can help to widen or narrow your search.
Let’s use our example in article 1 to explore the Boolean connectors. Our original question was about whether or not fluoride varnish has an effect on caries rate in children. The formulation of a PICO question resulted in this:
- Population, patient or problem: Children
- Intervention or treatment: Fluoride varnish
- Comparison: No treatment
- Outcome: Caries.
Using AND
To construct a search for Pubmed we could use the following:
- Children AND “Fluoride varnish” AND Caries
This would produce results from papers that contain all three search terms. This is a method for narrowing a search.
Phrase searching and using speech marks
You may also have noticed that the words “fluoride varnish” have speech marks either side of them. This is another useful way of narrowing a search for a specific phrase. The speech marks instruct the search engine to only include studies that have the entire phrase. If we had searched without the speech marks then we would have papers returned that include fluoride as a standalone word from varnish and not specific to our question
Using OR
Using OR can help to widen a search. For example, if we were interested in fluoride treatments other than fluoride varnish we might search the following:
- Children AND (“Fluoride varnish” or “Fluoride mouthwash”) and Caries
This would produce results from papers that contain all our original three search terms but also include studies that look at fluoride mouthwash. Again, note the use of the speech marks to search for the entire phrase.
Truncation
Truncation is useful when you want to expand a search. An example might be in periodontics. By using the trunk of the word Periodont and then adding * to the end will return results for Periodontist, Periodontal, etc.
Controlled language searches
A more advanced way of searching the database is to use controlled language searches. MEDLINE uses Medical Subject Heading, known as MeSH. Those studying for higher level degrees may wish to use this method in their searches. Speaking to the university librarian or doing a short course would be the best way to learn more on this topic. A useful tip about PubMed is that you can register for a free account and save your searches as you go. You can also access the free online tutorials that will help you understand how to get the most out of the database.
Subscriptions/access to resources
Guidelines produced in the UK by groups such as SDCEP, SIGN and NICE are free and open access. They are readily available online. The Cochrane library is also free and open access in the UK and other countries who contribute to it, while it is also available in some developing countries. Some journal articles may be free but most will be only be available through subscription to the journal itself or via an institution of which you are a member.
All NHS employees are entitled to free registration on OpenAthens, which will give you access to The Knowledge Network that is maintained by NHS Education for Scotland. That includes general dental practitioners with an NHS contract. It is a gateway platform to accessing full text articles. If you register then you can access most articles that are returned in searches on PubMed; then you simply enter you username and password once the pay wall appears.
You can register at the address here: www.athensregistration.scot.nhs.uk
Royal College Library
If you are a member of a royal college then you have an entire library service at your disposal. Royal colleges offer members the services of a librarian who can help with literature searches and also source books that may be relevant to your search. Be sure to explore this service that is part of your membership subscription.
Specialist societies and unions
Many specialist societies have subscription services for their members. The BDA also has an extensive library and journal service for use by members which can be accessed remotely through their website.
Question 3: Critically appraising the evidence (APPRAISE)
Not every article published in a journal is a game changer. Sometimes this is easy to spot when reading an article, but other times it may be less clear as authors try to convince you about their work. Understanding the hierarchy of evidence and having some basic skills in critical appraisal will help you when trying to decide how seriously to take a new recommendation or proposed change in practice. Having critical appraisal skills can have wide-reaching benefits beyond the surgery.
At this point, we have defined our search question and found the papers we think are relevant. We know about the hierarchy of evidence, but how do we decide which ones to use? Do they all meet the same standard? Are the results valid? Do they apply to the patients I see on a day-to-day basis? Do the results include the negative outcomes of the treatment?
These questions are important to consider, how we act on the evidence will affect our patients.
Using a systematic approach to appraising the evidence in front of you is always the best way. There are a range of appraisal tools available and some are available for free download from the Centre of Evidence-based Dentistry website: www.cebd.org
The best way to understand critical appraisal is to practice it. If you are brand new to it, then there are a number of ways you can get help to get started. This could be by attending face-to-face or online courses, reading a book or attending a journal club.
Online e-modules and tutorial videos
Terry Shaneyfelt is a teacher of evidence-based medicine; he has produced a number of YouTube videos that are useful when trying to get your head around critical appraisal. Simply search YouTube for ‘Terry Shaneyfelt’ and click on his playlists where you will see the critical appraisal section.
If you wanted to spend some time and do an online e-module then you can access one provided by the Critical Appraisal Company. There is a cost associated and the course takes six to eight hours, but it gets good reviews.
Journal clubs
Most dentists in core or specialist training will have access to a journal club in their place of work. If there isn’t one, why not take the lead and get one started over a lunchtime once a month? There are other journal clubs that anyone can attend, such as the Edinburgh Dental Journal club that meets regularly at the Royal College of Surgeons of Edinburgh. Search for them on Facebook© to find out when the next meeting is.
Conclusion
Hopefully, after reading these first two articles you now have a basic understanding of the skills needed to practice evidence-based dentistry. We have introduced you to a range of resources that can help you to further develop your skill and knowledge. The best way to get better at using databases for searching and critical appraisal is to get on and do it. Look out for your local journal club or go online and make the most of the many free resources there are to hand.
The next and final article will focus on applying the evidence and evaluating outcomes in your practice.
About the authors
 Niall McGoldrick BDS, MFDS RCPS(Glasg)
Niall McGoldrick BDS, MFDS RCPS(Glasg)
Neil is a specialty registrar in dental public health and is currently studying for his masters of dental public health at the University of Dundee. He graduated from Dundee Dental School in 2013 and then went onto complete longitudinal dental foundation training and dental core training in a range of specialities in Scotland including a placement with the SDCEP. He is a co-founder of the Scottish Charity, Let’s Talk About Mouth Cancer that is focused on the early detection of mouth cancer. He has received multiple awards for his work both inside and out of the NHS. Most recently, he received a National Award, NHS Young Achiever, from NHS Scotland and Scottish Government.
 Derek Richards BDS, FDS, MSc, DDPH,FDS(DPH)
Derek Richards BDS, FDS, MSc, DDPH,FDS(DPH)
Derek is a consultant in dental public health, editor of the Evidence-based Dentistry Journal and director of the Centre for Evidence-based Dentistry now based at the Dental Health Service Research Unit in Dundee. He holds honorary senior lectureships at Dundee and Glasgow Dental Schools and is a specialist advisor to the Scottish Dental Clinical Effectiveness Programme (SDCEP). He has been involved with a wide range of evidence-based initiatives both nationally and internationally since 1994. He is a co-author of the book, Evidence-Based Dentistry: Managing Information for Better Practice (Quintessential of Dental Practice) and the chief blogger for the Dental Elf website.
Bibliography
Derek Richards, Jan Clarkson, Debora Matthews, Rick Niederman. Evidence-based Dentistry: managing Information for Better Practice. London: Quintessence Publishing; 2008
Jan Clarkson, Jayne E Harrison, Amid I Ismail, Ian Needleman, Helen Worthington. Evidence Based Dentistry For Effective Practice. London: Martin Dunitz; 2003
| Database | Type of evidence | Key feature |
| PubMed | Systematic Reviews, Primary Research | Ability to create an account and save search results for later use |
| Cochrane Library | Systematic Reviews | Includes plain language summaries of reviews; useful for translating evidence for use at chair side |
| TRIP | Guidelines, Systematic Reviews, Primary Research | Displays results in the style of the hierarchy of evidence, reducing search time |
FIGURE 1: A screenshot of the PICO input section on TRIP. It can be accessed by typing TRIP database into any search engine or via www.tripdatabase.com
A new patient in her early 30s attended for a check-up. A routine radiograph revealed caries under the amalgam filling on the upper right second premolar (UR5). When advised the tooth needed treatment, the patient revealed she had been unhappy with how it looked. The filling was very visible and shiny when she smiled. The dark appearance of the tooth also made her self-conscious. The patient had thought treatment would be long and expensive, so she hadn’t bothered to ask.
The options were to have another amalgam filling or a composite restoration. The patient was advised that further composite treatment could be needed buccally to mask any remaining grey discolouration, if she was not satisfied with the outcome. As she was concerned about the appearance of the tooth, the patient did not want an amalgam filling and decided to have the composite restoration.
Preparation
After a local anaesthetic was given, rubber dam was placed, with a clamp on the UR6, exposing the UR 4, 5 and 6. This was secured in place with floss ties. The old amalgam and caries were removed. The final portion of discoloured dentine was left behind as it was very deep, but the pulp was not exposed and it was still firm.
A sectional matrix band was then positioned mesially on the UR5, with a wedge and separation ring (V-ring). Initially, the enamel periphery alone was etched with 37 per cent phosphoric acid for 15 seconds. Etch was applied to the rest of the cavity for a further 15 seconds, before rinsing. A cotton pledget was used to protect the dentine during the drying process, to ensure dry enamel and moist dentine.
A two-bottle adhesive, with separate primer and adhesive, was used to complete the preparation. The dentine was primed and left for 30 seconds. The adhesive was placed on both the enamel and dentine, and allowed to sit for
30 seconds before curing.
Restoration
In this case, Venus Pearl composite was used. This material exhibits good levels of opacity to block out discolouration and excellent handling for posteriors, making it a very easy-to-use product.
In this restoration, a small amount of Venus Flow base liner was placed and cured. This was to mask the greyness and dark discolouration from the base of the cavity. Next a thin layer of Venus Pearl A2 shade was applied to build up the mesial wall against the matrix. The height was built up to the level of the adjacent marginal ridge. The material was then manipulated with a sharp probe at a 45 degree angle. This ensured the edge of the wall was not straight and the natural curved shape of the marginal ridge was maintained. The dentine mass was built up in increments with Venus Pearl ODC shade.
Enamel A2 shade was placed over the occlusal surfaces cusp by cusp. Complete separation of the masses was achieved by creating fissures down to the dentine layer, using a sharp probe. Secondary anatomy was manipulated into the unset material before light curing.
A mix of Venus Color ‘corn’ and ‘choco’ stains was applied to the fissures using a probe, and pressed in with a long- bristle brush. The excess was wiped away with a conventional micro-brush and the stain was cured. Highlights were placed on the ridges using Venus Color ‘white’ mixed with a little ‘corn’, to give a milky colour. Final adjustments were carried out before rough, dry polishing. The restoration was then sealed with a protective clear coating, covered with glycerine and cured.
Outcome
In this case, the clinical outcome was good. The tooth is regularly monitored for vitality and the patient has had no problems with it. As the caries was so deep, in the long term the tooth may require root canal treatment, but it is currently sound. The patient was delighted with the result after having endured an unsightly amalgam filling for years.
 FIGURE 1: A routine X-ray revealed caries under the amalgam filling in the upper right 5
FIGURE 1: A routine X-ray revealed caries under the amalgam filling in the upper right 5

FIGURE 2: The UR5 filling was very visible when she smiled and the dark appearance made her self-conscious

FIGURE 3: The old amalgam and caries were removed following rubber dam placement

FIGURE 4: Kulzer Venus Pearl A2 shade was applied to build up the mesial wall

FIGURE 5: Separation of the masses was achieved by creating fissures down to the dentine layer and then stain was applied

FIGURE 6: The patient was delighted with the result after having endured an unsightly amalgam filling for years
About the author
Dr Monik Vasant BChD MSc is a highly experienced clinician with a special interest in minimally invasive aesthetic dentistry. He has trained under many of the world’s leading clinicians and has an MSc in aesthetic and restorative dentistry.

He is the director of Freshdental,with sites in Central London and Greater Manchester.
Monik lectures globally on minimally invasive and adhesive dentistry. His highly regarded direct composite course “Totally composite” is held throughout the UK and internationally. He also runs a year long minimally invasive aesthetic dentistry course entitled ‘Totally Aesthetics’.
Monik is a global key opinion leader for several dental companies and has co-authored several books on various aspects of general practice.
Contact monik@freshdental.co.uk or for course information and bookings, visit www.monikvasant.co.uk
Follow Monik on Instagram @drmonik
Monik is the keynote speaker at the Scottish Dental Show 2018, to be held at Braehead Arena on 27 and 28 April. He will be presenting two lectures on Friday 27 April, ‘Composite artistry’ and ‘Composites and digital dentistry’.
To find out more and to register for your FREE delegate pass that will get you access to 140 exhibition stands and more than 50 lecture and workshops sessions, with up to NINE hours of vCPD, visit www.sdshow.co.uk
Mrs M attends her dentist, Mr A, complaining of pain in an upper tooth. They discuss treatment options and she agrees to undergo private treatment, including root filling and the fitting of a new crown. She signs a treatment plan which shows the cost of the work will amount to around £500.
The treatment is carried out without incident and Mrs M pays part of the bill before leaving that day. The practice sends out an account detailing the remaining total but, three months later, no further payments have been made. Mr A issues another written account to Mrs M but is then contacted by Mr M who says he is assuming responsibility, with his wife’s consent, for the bill. He asks why the cost is so high but Mr A explains the treatment given and that the price was agreed in advance.
Five months after the initial appointment, still no further payment has been made. Mr A phones Mr M at home to discuss the matter. There is no answer but the phone switches to an answering machine, identified as belonging to Mr and Mrs M. He leaves a message asking Mr M to contact the practice about the unpaid bill.
One week later, Mr A receives a cheque for £150 from Mr M along with a promise that more money will follow soon. It is also accompanied by a letter of complaint from Mr M who is angry that the dentist disclosed information about the unpaid bill in the answering machine message. His daughter had dropped by while he was out and heard it, causing him considerable embarrassment.
Mr A sends a written apology to Mr M and agrees to let him pay the bill off over the next two months.
A short time later, however, Mr A is notified by the General Dental Council that a complaint has been made against him alleging a breach of confidentiality and claiming the cost of treatment was unfair and had not been
clearly discussed.
Analysis/outcome
Mr A calls MDDUS for advice. It is recommended he writes a further letter of apology to Mr M. Mr A accepts that sensitive information about the unpaid bill should not have been disclosed in the phone message and that practice procedures have been changed to avoid a repeat of this error. It is also advised that Mr A waives the outstanding sum owed to the practice in recognition of the distress caused by the confidentiality breach.
Regarding the disputed fee, Mr A is confident that this was fully discussed with the patient in advance and he has the treatment plan signed by Mrs M to support this.
The GDC case is eventually closed with no action taken against Mr A.
Key points
- Never disclose sensitive patient information in telephone messages
- Be aware of the potential for third parties to intercept messages, even on personal mobile phones
- Always ensure costs are discussed and agreed upon, in writing, before treatment is carried out.
About the author
Aubrey Craig is head of dental division at MDDUS. For more information, go to www.mddus.com
Imaging is essential in endodontics. Traditionally, X-rays (radiographs) have been used and more recently cone beam computed tomography (CBCT) is used to give the clinician more detailed tooth information as part of a clinical examination.
Radiographs have been an invaluable tool in the dentist’s armamentarium in the diagnosis and management of dental problems, (Grondahl and Huumonen, 2004), since their introduction in 1865. Radiographs may be taken as single parallel images or two images applying the parallax technique. Radiographs fundamentally represent a two-dimensional representation of a three-dimensional spatial relationship. The shortcomings and limitations of radiographs are; a degree of magnification – 5 per cent or more (Voorde and Bjorndahl, 1969), superimposition, geometric distortion and lack standardization or reproducibility.
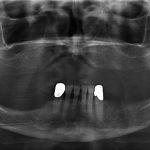
Aria et al 1999 and Mozzo et al, 1998 independently developed a new tomographic scanner known as CBCT and this was specifically for maxillofacial and dental use. CBCT (Fig 1) is a modern three-dimensional imaging system which produces high-quality images using relatively low doses of radiation (see Table 1).
TABLE 1: Comparisons of scans reproduced from Essentials of Dental Radiography and Radiology, 4th edition 2007

CBCT differs from ‘medical’ multi-slice CT (MSCT), as the whole volume of data is acquired in a single sweep with rotations varying between 180-360 degrees. The scanning time is reduced, typically 10-20 seconds, and radiation dose to the patient is less since the cone shaped (not fan shaped as MSCT) beam is pulsed, reducing exposure times to only 3.5 seconds. Approximately 580 images are produced and the field of view (FOV) can be as small as 40mm x 40mm, which can be useful in endodontics (SEDENTEXCT 2012) (Fig 2).
FIG 1: An Accuitomo small volume CBCT scanning machine (Image reproduced from J.Morita USA Inc)

Application of CBCT in endodontics
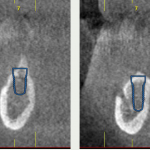
Limited volume (small FOV) CBCT scanners capture small volumes of data that can include just two or three individual teeth. CBCT allows the operator to view data in three planes: sagittal, axial and coronal (Fig 3). As all the information is obtained in a single rotation, it is very important that the patient is stationary throughout the exposure.
Spatial resolution is a drawback with CBCT since there is only approximately a tenth of the resolution that is currently available with digital and conventional radiographic films. “Increased resolution usually comes at the expense of an increased dose to the patient, as a result of longer exposure times to acquire more 2D projections to a more detailed reconstruction,” (Christiansen et al 2009).
Another limitation of CBCT scans are their vulnerability to beam hardening and streak artefact, which can reduce the image quality even further by producing dark bands or streaks in the image.
FIG 2: Basic concept of CBCT

FIG 3: CBCT image planes

Notwithstanding the above limitations, there are a number of applications for CBCT in endodontics which may overcome the limitations of conventional and digital radiographs and ultimately improve patient management. CBCT with a limited FOV may be considered in the below situations as recommended by the European Society of Endodontology (ESE) position statement 2014:
The use of CBCT in endodontics:
- Diagnosis of radiographic signs of periapical pathosis when there are contradictory (non-specific) signs and/
or symptoms - Confirmation of non-odontogenic causes of pathosis
- Assessment and/or management of complex dento-alveolar trauma, which may not be readily evaluated form conventional radiographic views
- Appreciation of extremely complex root canal systems prior to endodontic management
- Assessment of extremely complex root canal anatomy in teeth planned for non-surgical endodontic re-treatment
- Assessment of endodontic treatment complications (for example, [post] perforations) for treatment planning purposes when existing conventional radiographic views have yielded insufficient information
- Assessment and/or management of root resorption
- Pre-surgical assessment prior to complex peri-radicular surgery.
As stated by Rosen et al 2015: “A web-based survey emailed to 3,844 active members of the American Association of Endodontists in the United States and Canada reported a significant increase in the use of cone-beam computed tomographic (CBCT) imaging; 34.2 per cent of 1,369 respondents indicated that they were using CBCT imaging for diagnosis and treatment planning purposes,” (Dailey et al 2010).
Implications of CBCT in endodontics
There are a number of implications of CBCT in its application in endodontics, some of which have been discussed earlier, such as radiation dose and treatment outcome.
CBCT still uses ionising radiation and is not without risk. Radiation dose and ‘stochastic effects’ are important considerations. As discussed earlier, CBCT does expose patients to an increased radiation dosage. The principles of ‘As Low As Reasonably Achievable’ (ALARA) should always be applied to limit patient dose.
Every radiation exposure a patient has must be justified and optimised ideally with strict selection criteria as stated by the FGDP guidelines, 2013. The FOV must be reported on in its entirety since the clinician has a legal obligation to read and comment on the whole view. This highlights the training the operator must undergo before taking scans and the clinician must engage the advice of a suitably qualified radiologist if further advice/information is sought (Brown et al 2014).
The cost of CBCT scanners must not be allowed to motivate clinicians to take scans without first justifying the exposure. Ethical scanning is paramount.
Another implication may be the potential removal of metallic coronal restorations to avoid ‘beam hardening’, which would increase procedural time and patient cost.
Wu et al 2009 recommended that: “The outcome of root canal treatment should be re-evaluated in the long term using CBCT and stricter evaluation criteria”, for the reasons as discussed earlier. This has led many researchers to argue and debate a very crucial question: What constitutes endodontic success? An asymptomatic patient or a ‘healed’ scan or periapical?
“This has a huge implication on clinical decision making and selection criteria when considering (re-) placing coronal restorations on teeth which have previously been endodontically treated and appear to have successfully healed on the radiograph,” (FGDP 2013).
Some have asked for more clarification from the European Society of Endoontology (ESE), which has recently published a position statement: ‘The use of CBCT in Endodontics’, in 2014. The guidelines advise that “every image involving ionizing radiation, including CBCT, must be justified and optimised. A record of the justification process must
be maintained.”
“Clinical studies with a primary outcome measure of detecting the presence or absence of apical periodontitis and epidemiological studies assessing the prevalence of apical periodontitis in different populations may have to be re-evaluated,” (Ng 2010).
The question, therefore, may be posed as to how much relevance a CBCT has in clinical decision-making in endodontics? If a clinician has not obtained enough relevant information from a radiograph and has made the clinical judgement to expose the patient to a CBCT scan, does the information provided by the CBCT image have an effect on the clinician’s clinical management of that patient? Does the exposure of the patient to a CBCT image have a net positive benefit to the patient? Is this justified following the guidelines discussed earlier?
The scoping searches showed a number of papers important to this review in the existing literature:
- Balasundaram et al 2012. Comparison of Cone-Beam Computed Tomography and Periapical Radiography in Predicting Treatment Decision for Periapical Lesions: A Clinical Study.
- Cheung et al 2013. Agreement between periapical radiographs and cone-beam computed tomography for assessment of periapical status of root filled molar teeth.
- Mota de Almeida et al 2014. The impact of CBCT on the choice of endodontic diagnosis.
- Estrela et al 2014. Characterization of successful root canal treatment.
- Mota de Almeida et al 2014. The effect of CBCT on therapeutic decision-making in endodontics.
- Rosen et al 2015. The diagnostic efficacy of CBCT in endodontics: A systematic review and analysis by a Hierarchical Model of Efficacy.
- Ee et al 2014. Comparison of endodontic diagnosis and treatment planning decisions using CBCT vs periapical rads.
- Hashem et al 2015. Clinical and radiographic assessment of the efficacy of calcium silicate indirect pulp capping: a randomised controlled clinical trial.
- SEDENTEXCT Project. Radiation Protection 172. Evidence-Based Guidelines on Cone Beam CT for Dental and Maxillofacial Radiology [Internet]. 2011 [cited 2012 Dec 10]. Available at: http://www.sedentexct.eu/content/guidelines-cbctdental-and-maxillofacial-radiology. Accessed August 6, 2012.
Scoping searches to formulate an idea of the current state of knowledge of the topic literature showed limited studies in this area. Studies that were found appear mainly to be in-vitro with few in vivo studies. This, of course, highlights the justification of performing in vivo studies in humans where ethical issues are paramount in the 21st century. Scoping searches were performed using the PROSPERO, PubMed and Google Scholar databases. Scoping searches also identified a number of well-published authors who appear to be leaders in the field of CBCT: S Patel, C Durack, F Abella, M Roig, H Shemesh, P Lambrechts and K Lemberg.
CBCT can overcome some of the limitations of intra-oral radiographs, which are the primary imaging method in endodontics (Lofthag-Hansen et al, 2007 and Scarfe et al, 2009).Therefore, the usefulness of CBCT imaging can no longer be disputed, since they can complement radiographs. It is an important imaging tool in contemporary endodontics and “has been shown to be superior to conventional periapical and panoramic radiography in its accuracy and sensitivity in detecting endodontic related pathology” (Stavropoulos and Wenzel, 2007, Tsai et al, 2012, Liang et al, 2014).
As scanners become more affordable and radiation dose to the patient possibly reducing, more endodontic disease may be detected in the future, which inevitably means better patient management. However, Pope et al 2014 have discussed that more sensitive technology may cause over-diagnosis, which could potentially harm
healthy patients.
Presently, academic opinion (ESE position statement, 2014) advises that “CBCT should only be considered in situations where diagnostic information from clinical examination and conventional radiographs does not yield an adequate amount of information to allow appropriate management of the patient. A case-by-case approach is recommended and a CBCT scan should have a net benefit to the management of a patient’s endodontic problem”.
Clinical decision-making in endodontics
Clinical decision-making in endodontics is a process which involves the clinician’s diagnostic skills and the patient’s presenting signs and symptoms. It is a conclusion reached only after assessment of signs, symptoms, examination, special tests, consideration of expected outcome and, most importantly, the patient’s wishes. Therefore, “decision-making depends on the skill and experience of the clinician and the treatment options available which is termed as evidence-based practice” (Sackett et al, 1996).
However, “the needs and preferences of the patient are what drives the treatment decision since only the patient is truly the expert as to how he/she feels about maintaining a tooth, what symptoms are tolerable, what risks are worth taking and of course what costs are acceptable” (Bergenholtz and Kvist, 2014). Therefore, a patient-centred outcome is ideal. “Diagnosis is seen as only one part of the medical decision process” (Ledley and Lusted, 1959). Once a clinical decision has been reached, only then should treatment be executed with the patient’s informed consent.
TABLE 2: A Hierarchical Model of Efficacy: Typical Measures of Analysis (Fryback and Thornbury 1991)

Radiographs have been used as an imaging tool to base clinical decisions on and Strindberg developed a system in 1956. His system was based on biology and can be perceived as being dogmatic and inflexible. In the Strindberg system, a normal periradicular situation on periapical image with no patient symptoms was identified as endodontic success and a periradicular lesion apparent on a periapical radiograph was identified as endodontic failure. This has been discussed by Kvist 1994 and in a series of papers (Papers I-V, 1998, 1999 and 2000) where he proposed an alternative theory based on Praxis Concept (Jensen 1985). Praxis, which is Greek for process, is the process by which a theory or skill is enacted, embodied or realised. This theory states that personal values influence endodontic treatment and that clinicians use ‘cut-off’ points in their decision-making process.
Fryback and Thornbury (1991) have discussed the assessment of the contribution of diagnostic imaging to the patient management process in their seminal paper, The Efficacy of Diagnostic Imaging. In their study, they propose a ‘Hierarchical Model of Efficacy’, which is an organising structure for appraisal of the literature on the efficacy of imaging. There are six levels as listed in Figure 4:
- Technical quality of image
- Diagnostic accuracy, sensitivity and specificity of image interpretation
- Change in clinician’s diagnostic thinking?
- Effect on patient management
- Effect on patient outcomes
- Societal costs and benefits of a diagnostic imaging technology.
According to Fryback and Thornbury (1991), with level three “the imaging information may change the differential diagnosis, strengthen an existing hypothesis, or simply reassure the physician”. With level four, ‘Therapeutic Efficacy’, “an imaging examination result may influence the physician’s diagnostic thinking and yet have no impact on patient treatment”. With level five, ‘Patient Outcome Efficacy’, “is concerned with whether there is measurable effect of the image on the outcome experienced by the patient” since the ultimate goal of dental care is to improve, or return to normal, the health of the patient.
Therefore, this structured critical review will focus on levels three, four and five in the ‘Hierarchical Model’ (Table 2) since the question posed is the use of an imaging modality (CBCT) and how it influences clinical decision-making in endodontics.
So, with regards to the use of CBCT in clinical decision-making in endodontics, what does the current literature say? Evidence appears to be sparse. Mota de Almeida et al (2014) have concluded that “CBCT has a substantial impact on diagnostic thinking in endodontics when used in accordance with the European Commission guidelines”. In their clinical study, Balsundaram et al (2012) concluded that “Lesion size and choice of treatment of periapical lesions based on CBCT radiographs do not change significantly from those made on the basis of 2D radiographs”. Cheung et al (2013), concluded that “there were substantial disagreements between PA and CBCT for assessing the periapical status of molar teeth, especially for the maxillary arch”.
It is clear that there is not an agreement of opinion and whether there is a clear benefit to the clinician and to the patient in taking a CBCT scan. An investigation of available evidence as it relates to levels three, four and five, may clarify the role of CBCT in endodontic decision-making.
The research question for this study: Does CBCT influence clinical decision making in endodontics?, arose from the author’s interest in the imaging modalities used in endodontics. In the author’s almost 20 years clinical experience, it has been noted that many Scottish patients wish to keep their teeth and avoid extractions. People’s attitudes to dentistry, which may be media and culturally led, appear to be changing. The limitations within the National Health Service (NHS) in Scotland, may have led patients to look at private options to restore their teeth with a view to avoiding costly dental implants.
In the author’s opinion, root canal treatments are being considered more by patients, not only on the NHS but also privately. The author has found that since patient expectations are sometimes high, the diagnostic process must give the clinician and patient as much information as possible so the patient is able to make the correct informed decision. CBCT may offer more information, as discussed earlier, but does this information make a difference in the decision-making process? CBCT, being a relatively new and exciting diagnostic tool in endodontics, is used by some general dental practitioners and specialists in the UK but its use should be only when radiographs do not prove diagnostically beneficial. The question arises, when is this?
As discussed earlier, ESE guidelines are quite specific. CBCT should not be taken routinely in the diagnostic process but only when there is a net benefit to the patient. Clinically, a patient may present to a clinician with symptoms which cannot be diagnosed either upon clinical examination or with a radiograph. In this scenario is a CBCT useful?
The aim of this study is to perform a structured critical review on the current published research and to draw a conclusion as to the influence of CBCT in clinical decision making in endodontics.
The objectives of this review are based on nine basic steps, as suggested by Boland et al (2014):
- Performing scoping searches, identifying the review question and writing the protocol
- Literature searching including the search strategy
- Screening titles and abstracts
- Obtaining papers
- Selecting full-text papers
- Quality assessment
- Data extraction
- Analysis and synthesis
- Writing up and editing.
 About the author
About the author
Arvind Sharma, BDS(Dund), MSc(Endo), MJDFRCS(Eng), MFDSRCPS(Glas), work in practice limited to endodontics and takes referrals at New Life Teeth in Edinburgh and Philip Friel Advanced Dentistry in Glasgow.
This article is based on the submitted dissertation in partial fulfilment of the requirements for the Degree of Master of Science in Endodontology, 2016. The author appreciates that much of the in-depth analysis has been omitted for the purposes of the current publication and readers are welcome to contact the author for more detail if they so wish – visit asendodontics.com for info.
References will be provided in full in the second part of the article, which will be published in the next issue of Scottish Dental.
This article is the first in a series that aims to introduce the modern-day dental practitioner to evidence-based dentistry (EBD). After reading this series, you will be clearer about how to keep abreast of the ever-growing evidence base and the latest guidance. You will know where to look for evidence and learn how to maximise time spent searching for evidence to inform your practice.
In our day-to-day lives, we have become accustomed to using search engines such a Bing or Google to help answer simple questions, but, when it comes to our clinical work and professional life, we need to take a more formal approach in our search. There are a number of web-based scientific databases that catalogue evidence. The databases can be thought of as massive online libraries, but like any library, if you don’t know your way around it or the cataloguing system used, then you are likely to get lost and spend hours searching for what you need. Therefore, having an awareness of the different scientific databases available and understanding how to use them is a good starting point.
An example of a well-known database, and one you may have already used is PubMed. Simply typing the word ‘dental’ into the search box on PubMed results in more than half a million hits – 516,870 to be precise. These 516,000 hits are spread over 25,844 pages, which makes for a lot of reading. Clearly, we need a more focused approach. So, what then if we pick a subject within dentistry such as fluoride varnish? This search still returns 1,293 hits spread over 65 pages.
The point we are demonstrating here is that there is a wealth of information and publications that we can make use of, but there is some skill required to negotiate databases and identify quality evidence. A busy practitioner needs access to high-quality evidence quickly and easily.
Evidence-based dentistry
The American Dental Association describe EBD as “an approach to oral healthcare that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient’s oral and medical condition and history, with the dentist’s clinical expertise and the patient’s treatment needs and preferences.”[1]
As dentists we want to do our best for each and every patient we treat, and this is at the heart of EBD. Most dentists will be confident in their clinical skills and will listen to patients but not all will be confident in the strength of evidence behind how and what they practice. The evidence should be a constant go to for a modern-day dentist.
Developing an evidence-based approach can be thought of in five stages:
- Asking the right question
- Searching for the best available evidence
- Critically appraising the evidence
- Applying the evidence
- Evaluating the outcome.
In your life outside of the surgery, you will already be using this approach, whether you realise it or not. Take buying a new car, for example. Let’s say it is a used car; you may not want to rely solely on the sales person’s word that the shiny car on the forecourt really is the best one for you. You will need to think about what it is you really need from the car – is a sporty convertible with two seats and no boot space going to suit your lifestyle? Maybe it is.
Most people will search the internet comparing various cars on independent websites; they will look in magazines or speak to friends and family beforehand. So, when you arrive at the showroom you already have an idea of what you are looking for and what you need from a car. At this point, you have carried out the first stage of an evidence-based approach: Asking the right question. You have also begun the second stage: Searching for the best available evidence.
When you have identified a potential car, you will want to continue your search for evidence to support your decision to buy. You will want to know more details about the service history, you might inspect the paintwork, check how many miles it has done and ask about previous owners. You will combine this information with what you found out previously and check the quality of the evidence before you. This is stage three: Critically appraising the evidence.
Next comes the big decision; whether to go ahead with the purchase. After carefully considering all the evidence you have available, you may or may not decide to buy the car, this is stage four: Applying the evidence.
The final stage is evaluating the outcome. This will take place in the months and years to come when you will be driving the car. If the car keeps breaking down and needs multiple new parts, you might question your approach and the evidence upon which you based your decision.
In this article we will cover stages one and two of the evidence-based approach.
Figure 1: Hierarchy of evidence [2]
Asking the right question
Evidence-based dentistry starts with a clinical question. You need to be clear about what it is you are trying to find evidence for. A good technique to help develop your question is to use PICO.
What is PICO?
PICO is an acronym for Population, Intervention, Comparator and Outcome. It is used when developing a question regarding a clinical scenario. Say, for example, you are a general dental practitioner; you suggest that the five-year-old patient in your chair should have fluoride varnish applied to her teeth. The patient’s parent questions this; he asks you “what good will it do?”, and at this point, he does not provide consent.
Using the PICO approach, we can build our question and start our search for the evidence. First of all, we need to establish the key population group that we want to find evidence about. In this case, it is children.
Next, we need to think about what treatment we are proposing and what the alternative might be. Here, we are proposing fluoride varnish application and the comparison would be no fluoride varnish. You could also choose an active treatment for comparison, such as fluoride mouthwash or toothpaste. Having an alternative prevention option might help win over the parent in this scenario.
Having a clear idea about what outcome you want from the treatment is important. Here, our key outcome is the caries rate in the child.
As a result of this process, we now have a PICO question we can use in a database search:
- Population, patient or problem: Children
- Intervention or treatment: Fluoride varnish
- Comparison: No treatment
- Outcome: Caries.
Searching for the best available evidence (AQUIRE)
We now have a clear PICO question for moving forward with and have completed stage one. In the next stage, we need to think about the types of evidence there are and where we can find them.
This section will aid you in the search for the best available evidence. It has two parts. In the first part we will explore the hierarchy of evidence and the uses for each type, while the second part published in the next article, will take you through the practicalities of different databases.
Types of evidence
First let us think about the different types and levels of evidence available. The most common and easy way to think about evidence is as a pyramid or hierarchy as shown in Figure 1 on the previous page.
It is quite intuitive, with the highest levels of evidence found at the top of the pyramid. Each type of evidence has a role to play in shaping healthcare. We will work our way up the pyramid discussing each of the types of evidence in turn while exploring the pros and cons of each.
In vitro/animal research
Animal and in vitro research can be useful in the initial stages of developing treatment, for example when exploring causes behind disease or investigating an early idea or hypothesis.
The dental materials we use are initially tested in the lab. If they fail at this stage then there would be no point in testing the material in humans without overcoming the initial flaws identified.
With animal experiments there can be an issue when it comes to translating or replicating findings in humans. Some treatments may never work or they may actually be harmful to humans. The process of getting from the lab bench to chair side can take decades of refinement.
In this article, our focus is on what works best in the clinical situation and therefore this type of lab-based study is not immediately transferable into practice.
Ideas, editorials and opinions
Initially, most people think their own ideas are great but do they stand up to the scrutiny of others? As we mentioned above, ideas need testing. Personal opinions and written editorials often only provide one view point. Therefore, it would not be a good idea to change your practice based on a discussion over a cup of coffee or on a single editorial on a website, magazine or journal.
There are occasions when a combined opinion can be useful though. Sometimes professional groups come together to give an opinion or stance on a particular issue. This often involves bringing together a range of currently available evidence. The downside is that the opinion will include some of the group’s own biases.
A recent example of a professional group summarising evidence is the Scottish Consultants in Dental Public Health Group, Recommendations on the use of fluoride toothpaste and fluoride supplements in Scotland 2017[3]. The document is clearly referenced and has been produced in consultation with a renowned guideline development group. This type of opinion holds more weight and can be taken more seriously.
Case reports/Case series
A large number of articles published in dental journals tend to be case reports or case series. They are based on one or very few cases. Treatment is often provided by one practitioner with a particular special interest or expertise. It may be difficult to directly replicate the treatment situation. Also, the patient characteristics are unlikely to be exactly the same as your patient.
They are particular useful in the case of rare or serious events. A case series published in 2012 presented two cases of fatal anaphylaxis following irrigation of tooth extraction sockets with chlorhexidine[4]. Rare events such as this can change practice very rapidly.
Case-control studies
Case control studies are retrospective observational studies. They do not test an intervention but are used to help find out what might cause a disease or be associated with it. As the name suggests, they are made up of two different groups, cases and controls. Cases will have the particular disease of interest and will be compared to controls that do not have the disease of interest. Researchers will take extensive histories from both groups and compare factors such as lifestyle. They are useful for establishing risk factors that are associated with a disease.
Recently there has been a lot of interest in understanding the causes of dementia. With an ageing population, if we could find out how to prevent dementia then this could have a great impact on the health of the population. One hypothesis queries whether periodontitis has any association with dementia. A research group in Granada carried out a case control study to find out if there was such an association. They compared 180 people with cognitive impairment to 229 without any impairment. After controlling for known risk factors they found there was a statistically significant association between periodontitis and dementia[5].
As mentioned before, case control studies are useful for establishing if associations exist between risk factors and disease. A lot more evidence is required in order to prove causation and establish the sequence. In this example, one might question whether the periodontal disease came before the dementia or whether the patient developed dementia and then stopped brushing as well as before? If you want to learn more about causation, then a good starting point is to read about the work of Sir Austin Bradford Hill. Sir Bradford Hill was an epidemiologist during the 19th century, in an after dinner speech he set out a number of considerations that should be taken into account when trying to establish causation[6].
Cohort studies
Cohort studies are another form of observational study and are much more useful in establishing causes of disease. As the name suggests, they include a cohort of people with all the subjects included in the study initially free from the disease of interest. Detailed histories and in some cases examinations take place at the beginning of the study. The cohort is then followed up, often over a number of years, and observed for signs of the disease.
One of the most famous cohort studies took place in the US in a town called Framingham. The town in Massachusetts was to be the centre of a study that has now lasted 69 years. It focused on understanding the causes of cardiovascular disease as public health specialists recognised this as a major threat to the population of the US. People in the town who were free of cardiovascular disease were enrolled in the study and observed for many years. Detailed information on behaviour, lifestyle and other characteristics were recorded. Investigations including blood pressure monitoring and ECG’s were carried out as the study progressed. It took 10 years for the first key finding to emerge. The researchers were able to show that as blood pressure increased, the incidence of coronary heart disease also increased[7]. The study produced the foundations of preventative medicine and discovered many of the causes for heart disease that we aim to prevent today.
Randomised controlled trials
A randomised controlled trial is the study of choice for testing new interventions in dentistry. They are experimental in nature and use randomisation techniques to reduce risk of bias and confounding factors that may influence outcomes. Patients are selected against strict inclusion and exclusion criteria ensuring they have similar baseline characteristics. There are then randomised into two arms, treatment and control. In the treatment arm, the subjects receive the new treatment under investigation. This is compared to the subjects in the control arm who will receive either placebo or current standard therapy.
Using a randomisation process to allocate patients to the different arms of a trial reduces the risk of selection bias, which is present when there are systematic differences between baseline characteristics of the groups being compared. Randomisation is best done using a computer-generated sequence that is independent of influence from the investigators. A trial that conceals group allocation from both the patient and the investigator is described as double-blind, in that neither know if they are receiving the new treatment or the alternative be that a placebo or standard care. At the end of the trial, the outcomes from each arm are then compared for any differences and inferences drawn on whether the treatment is effective.
There have been many randomised controlled trials (RCT) in dentistry, all of varying standards. Although an RCT is high in the hierarchy of evidence, it is still important to critique how the research was carried out and to what standard. We will cover that in article two.
Systematic reviews
The highest level of evidence is a systematic review. They bring together all the existing evidence on a particular question. Systematic searches of the literature are initially broad and can result in thousands of hits on databases such as PubMed. The review team will set criteria to focus the review down to include studies that answer specific questions. They then carry out critical appraisal of the studies to assess quality. If the studies all measure similar outcomes then the results of the trials can be compared by extracting the data and using statistical techniques in a meta-analysis. This gives more weight to the studies.
Guideline development groups
Guidance documents aim to bring together the current best available evidence on a given topic and make recommendations. National Guidance Groups such as Scottish Dental Clinical Effectiveness Programme, Scottish Intercollegiate Network and the National Institute for Clinical Excellence comprise a team of expert researchers and clinicians. They have a formal methodical approach to appraising the evidence; they combine this with expert opinion to arrive at their recommendations. We will look more at guidance and the influence they have on practice in the next article, which will feature an interview with Dr Doug Stirling from SDCEP.
Conclusion
So now we have reached the top of the pyramid and it should be becoming clear that there is a wealth and variety of information out there. We should be mindful of what evidence exists for the treatment we are providing our patients. Each type of study or research has its own pros and cons. The next article will focus on the practicalities of where to find the evidence, how to get the most out of databases and, importantly, how to critique the evidence you find.
Get involved
General dental practitioners have opportunities to get involved in clinical trials, especially in Scotland. A number of trials have been run from the University of Dundee including the IQuad trial which is an acronym for Improving the Quality of Dentistry. This trial looked at the effectiveness of the simple scale and polish on periodontal disease with published results expected soon. Find out more here.
The FiCTION trial, again it is an acronym, which stands for Fillings in Children Teeth Indicated or Not. Find out more here.
Recruitment to the latest clinical trial called REFLECT is ongoing. The trial is focused on understanding more about the effectiveness of 5000ppmf toothpaste. Dr Carly Ross BDS (Gla) MJDF (RCSEng), clinical research fellow and honorary specialty registrar in special care dentistry at the University of Dundee Dental School, explains about the role of general dental practitioners in helping shape the evidence.
Why does evidence-based dentistry matter to a general dental practitioner?
General dental practitioners have an important role to play in evidence-based dentistry. Along with the current scientific evidence and the patient’s needs, a GDP’s own clinical expertise helps to shape the concept of evidence-based dentistry. From this, clinical guidelines can be produced which assist GDPs in providing high-quality clinical care using the best available evidence.
How can dentists get involved in trials and shaping of the evidence?
Ninety percent of dental care is provided in primary care so it is essential that research is conducted in this setting. Many clinical trials take place in primary care in Scotland so input from GDPs is important to allow high-quality research to be carried out. The REFLECT clinical trial is being carried out in general dental practices and aims to evaluate the effectiveness and cost benefit of prescribing high dose fluoride toothpaste in older adults. The trial is currently recruiting practices in Scotland to take part.
If you are interested in taking part, please email reflect@dundee.ac.uk or call 01382 381 213 for more information.
Editor’s view
The Cochrane Collaboration carry out systematic reviews that include evidence derived mainly from randomised controlled trials. They use strict methodology and techniques for carrying out reviews and they can be thought of as setting the standard of how reviews should be conducted.
Dr Thomas Lamont, clinical research fellow and honorary specialty registrar in restorative dentistry at Dundee Dental School, is a clinical editor with Cochrane. Below he tells us in some more detail about the methods used in a Cochrane review and what his role is.
Who is involved in a Cochrane systematic review?
What is the skill mix?
Cochrane systematic reviews will include multi-disciplinary teams including patient representatives, clinicians, clinical academics, methodologists, statisticians, health economists, editors and
copy editors.
You are a clinical editor, what is your role?
As clinical editor, I help the review groups by providing clinical and methodological advice to the teams. I also help to peer review Cochrane reviews to ensure they meet the required Cochrane standards. I also provide lectures/seminars on the Cochrane review methodology to clinicians and academics.
Why does reviewing the evidence matter?
It is important that we review and integrate the evidence to ensure that we provide the best possible care for our patients. This cannot be done in isolation and needs to be combined with our own clinical experience and the wishes/values of our patients.
What relevance do the results of a Cochrane review have to a general dental practitioner?
Cochrane reviews provide high-quality evidence for use in the field. They add to the evidence base and distil a large amount of information, therefore making it easier for clinicians to make sense of all the
available evidence.
Find out more about Cochrane here: oralhealth.cochrane.org
References
1. American Dental Association. [Online] American Dental Association, 2017.
2. SUNY Downstate Medical Center. Medical Research Library of Brooklyn. Evidence Based Medicine Course. A Guide to Research Methods: The Evidence Pyramid.
3. Scottish Consultants in Dental Public Health Group, read online 24 March 2017. Recommendations on the use of fluoride toothpaste and fluoride supplements in Scotland 2017.
4. Chlorhexidine and hypersensitivity reactions in dentistry. M.N. Pemberton, J. Gibson. s.l.: British Dental Journal, 2012, Vol. 213.
5. Is periodontitis a risk factor for cognitive impairment and dementia? A case-control study. Gil-Montoya JA, Sanchez-Lara, Carnero-Pardo C, Fornieles F, Montes J, Vilchez R et al. Granada: J Periodontaol, 2015, Vol. 86.
6. The Missed Lessons of Sir Austin Bradford Hill. Phillips CV, Goodman KJ. Texas: BioMed Central, 2004.
7. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Syed S mahmood, Daniel Levy, Ramachandran S Vasan, Thoma J Wang. 9921, s.l.: The Lancet, 2014, Vol. 383.
Bibliography
• Derek Richards, Jan Clarkson, Debora Matthews, Rick Niederman. Evidence based Dentistry: Managing Information for Better Practice. London: Quintessence Publishing; 2008.
• Jan Clarkson, Jayne E harrison, Amid I Ismail, Ian Needleman, Helen Worthington. Evidence-Based Dentistry For Effective Practice. London: Martin Dunitz; 2003.
About the authors
Derek Richards BDS, FDS, MSc, DDPH,FDS(DPH), is a consultant in dental public health, editor of the Evidence-based Dentistry Journal and director of the Centre for Evidence-based Dentistry now based at the Dental Health Service Research Unit in Dundee. He holds honorary senior lectureships at Dundee and Glasgow Dental Schools and is a specialist advisor to the Scottish Dental Clinical Effectiveness Programme (SDCEP). He has been involved with a wide range of evidence-based initiatives both nationally and internationally since 1994. He is co-author of the book, Evidence-Based Dentistry: Managing Information for Better Practice (Quintessential of Dental Practice) and the chief blogger for the Dental Elf website.
Niall McGoldrick BDS, MFDS RCPS(Glasg), is a specialty registrar in dental public health and is currently studying for his masters of dental public health at the University of Dundee. He graduated from Dundee Dental School in 2013 and then went onto complete longitudinal dental foundation training and dental core training in a range of specialities in Scotland including a placement with the SDCEP. He is a co-founder of the Scottish Charity, Let’s Talk About Mouth Cancer that is focused on the early detection of mouth cancer. He has received multiple awards for his work both inside and out of the NHS. Most recently, he received a National Award, NHS Young Achiever, from NHS Scotland and Scottish Government.
Gingival swellings are one of the most frequently encountered lesions in the oral cavity 1. Many different conditions can present as swellings, which in some cases can make diagnosis difficult. These can range from the benign un-concerning fibro-epithelial polyps to potentially life threatening malignant lesions such as squamous cell carcinomas.
Peripheral odontogenic tumours are a group of benign rare neoplasms that occur in the mouth 2. Peripheral odontogenic fibroma is the most common type of peripheral odontogenic tumour 3,4 and presents as a benign, slow-growing, exophytic growth of soft tissue usually involving the gingiva.
We present a case of a peripheral odontogenic fibroma mimicking common gingival swellings. The article aims to discuss a systematic approach to managing this case as well as highlighting other possible differential diagnoses. Table 1 provides an overview of swellings affecting the oral mucosa that may aid diagnosis.
Clinical case
A 62-year-old woman presented with a rapid increase in size of a long-standing swelling (Fig 1) affecting the lower left alveolus, which had been present for approximately six months. There was no associated pain or paraesthesia. Medically she had a diagnosis of atrial fibrillation, valvular heart disease and vertigo, which were managed appropriately. This included warfarin for her atrial fibrillation.
She was an ex-smoker of approximately 15 years and had occasional alcohol.
Extra oral examination revealed asymmetry of the left mandible. There was no lymphadenopathy. Intraorally the patient was partially dentate, had poor oral hygiene and clinical and radiological evidence of periodontal disease (Fig 2).
A large 2-3cm swelling was noted involving the lower left alveolus in the premolar region. Both the lower left first and second premolar were grade II mobile. The swelling was firm to palpate, fixed and with normal overlying mucosa.
Differential diagnosis
There are many causes of intraoral swellings and use of a surgical sieve approach provides a structured list of aetiological groups for systematically identifying potential causes of a presentation. These have been summarised in Table 1.
Management and outcome
Due to the sudden increase in the size of the swelling, urgent mapping biopsies of the lesion were taken. This confirmed an initial diagnosis of fibro-epithelial hyperplasia with no evidence of malignancy.
The patient was referred to the oral surgery department for removal of the residual swelling and the periodontal involved lower left premolar teeth. This was undertaken in the day procedure unit under local anaesthesia. Prior to undertaking surgery a pre-operative INR (2.12) test was carried out. The swelling and lower left premolar teeth were successfully removed under local anaesthetic. Haemostasis was achieved with cautery and the surgical site was dressed with both BIP (bismuth subnitrate, iodoform and paraffin paste impregnated gauze) packing and a suck-down vacuum splint for the first 24 to 48 hours.
At review one month post-surgery, the excision site was healing satisfactorily (See Fig 3). The final histopathology confirmed a diagnosis of a peripheral odontogenic fibroma. The patient will be reviewed on a three to six-month basis to monitor for recurrence. Further surgery may be required in the future.
- FIGURE 2: Image one month following excision
- FIGURE 3 : Orthopantomogram
Discussion
Peripheral odontogenic fibroma is the most common peripheral odontogenic tumour followed by the ameloblastoma and calcifying odontogenic tumour 3, 4. The most common location is the attached gingiva, usually in the molar/premolar area with even distribution between the jaws 5.
Peripheral odontogenic fibroma is an uncommon, benign, focal unencapsulated exophytic gingival mass, composed of fibrous connective tissue derived from mesenchymal origin 6. It may be pedunculated or sessile, red or pink, usually with a smooth surface and in some cases the overlying mucosa may be ulcerated. The lesion is usually firm to palpation, non-tender and could be mistaken for other more common exophytic gingival lesions, such as fibrous hyperplasia, pyogenic granuloma, or peripheral giant cell granuloma.
In the case above, the patient had been referred with a suspected oral cancer due to the rapid increase in size of a pre-existing swelling. During examination and periodontal probing, poor oral hygiene and periodontal disease could be justified for the possible cause of mobility of the premolars. An orthopantomogram radiograph did confirm bone loss consistent with periodontal disease. However, there was no periapical or bony pathology suggestive of a possible cystic, giant cell or aggressive lesion.
Due to the history of a rapid increase in swelling urgent mapping incisional biopsies were undertaken to give a better histological representation of the swelling. On the basis of this malignancy was excluded. A planned excision was arranged due to the size of the swelling and the patient’s complex medical history.
| Normal Anatomy |
|
| Developmental |
|
| Inflammatory |
|
| Traumatic |
|
| Neoplasms |
|
| Fibro-osseous |
|
| Hormonal |
|
| Metabolic |
|
| Drugs |
|
| Allergies |
|
| Viral |
|
Table 1: Main conditions which may present as swellings or lumps in the mouth
Conclusion
An open mind should always be advised when managing many oral medicine/surgery cases. Many gingival lumps and swellings have similar clinical presentations and may mimic that of something more sinister. The oral cavity is a dynamic environment. This, alongside ever more complex medical histories, presents the general dental practitioner with a puzzle of information.
Despite a myriad of aetiologies, gingival swellings and lumps can often be diagnosed by a careful history. Simple factors such as presence of local irritants such as calculus could be a primary cause. By carrying out routine full head, neck and intraoral examinations and managing plaque control potential development of lesions
may be prevented.
Should further management such as biopsy, biochemistry or histological examination be required, it is important that the clinician makes an appropriate referral, providing all the essential information to enable effective, efficient and safe management of the patient.
About the author
Colm Hicks, BcHD, MFDS RCSEd; Amanda Willis, BDS, BMedSci (Hons), MMedSci PHD, MJDF RCSEng, PGCE, FDS (OM) RCPS(Glasg); John Marley, BSc BDS, PhD, FDS (OS)RCS Eng, FFDRCSI.
The authors would like to acknowledge Dr Seamus Napier, consultant oral pathology for carrying out the histopathology for this case.
References
1. Kannan S, Thapasum A, Suresh N, Muthusamy S, Chandrasekaran B. Localised Gingival Overgrowth – Differential Diagnosis for Dental Practitioners. Dental Update 2014; 41: 698–706.
2. Manor Y, Mardinger O, Katz J, Taicher S, Hirshberg A. Peripheral odontogenic tumours – differential diagnosis in gingival lesions. International Journal Oral Maxillofacial Surgery. 2004; 33: 268–273.
3. Ide F, Obara K, Mishima K, et al. Peripheral odontogenic tumor: A clinicopathologic study of 30 cases. General features and hamartomatous lesions. Journal Oral Pathology Medicine 2005; 34:552.
4. Buchner A, Merrell PW, Carpenter WM. Relative frequency of peripheral odontogenic tumors: A study of 45 new cases and comparison with studies from the literature. Journal Oral Pathology Medicine 2006; 35:385.
5. Kenny JN, Kaugars GE, Abbey LM. Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibroma. Journal of Oral and Maxillofacial Surgery 1989; 47(4): 378-382.
6. Savage N W, Daly C G. Gingival enlargements and localised gingival overgrowths. Australian Dental Journal 2010; 55: 55-60.
7. Felix H D, Luker J, Scully C Prof. Oral Medicine:11. Lumps and Swellings: Mouth. Dental Update 2013; 40: 683 – 687.
8. Saravana GHL. Oral pyogenic granuloma: a review of 137 cases. British Journal of Maxillofacial surgery 2009; 47:318 -319.
9. Motamedi MH, Eshghyar N, Jafari SM, et al. Peripheral and giant cell granulomas of the jaws: a demographic study. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontolgy 2007; 103: 39-43.
10. Walsh T, Liu JLY, Brocklehurst P, Glenny AM, Lingen M, Kerr AR, Ogden G, Warnakulasuriya S, Scully C. Clinical assessment to screen for the detection
of oral cavity cancer and potentially malignant disorders in apparently healthy adults. Cochrane Database of Systematic Reviews 2013, Issue 11.
11. Smittenaar CR, Petersen KA, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer. 2016 Oct 25; 115(9): 1147–1155.
12. National Institute for health care and excellence. Suspected cancer: recognition and referral – NICE Guideline NG12. 2015 (last updated July 2017) available online www.nice.org.uk/guidance/ng12/resources/suspected-cancer-recognition-and-referral-pdf-1837268071621 [last accessed January 18, 2018]
.
13. Healthcare improvement Scotland. Scottish referral guidelines for suspected cancer 2013 (updated in August 2014) available online www.healthcareimprovementscotland.org/our_work/cancer_care_ improvement/programme_resources/scottish_referral_guidelines.aspx [last accessed 18 January, 2018].
14. Agrawal AA: Gingival enlargements. Differential diagnosis and review of literature. World Journal of Clinical Cases 2015; 16: 3(9): 779-788.
15. Hallimon WW, Rossmann JA. The role of drugs in the pathogenesis of gingival overgrowth. A collective review of current concepts. Periodontology 2000; 21: 176-196.
16. Sculley C, Porter S. Orofacial Disease. Update for the Dental Clinical Team: 5. Lumps and Swellings. Dental Update 1999; 26: 214-217.
Short and extra-short implants are a powerful tool in oral implantology these days 1. The use of these implants facilitates the rehabilitation of very resorbed edentulous ridges with a simple approach. The principal problem with the short implants, and most commonly with extra-short implants, is the crown-to-implant (CI) ratio. The high space to rehabilitate and the longitude of these implants creates an unfavourable prosthesis on the basis of the CI ratio.
The CI ratio is a term imported by the general odontology, and the use of these parameters in implants is used in a similar way. The use of the concept in general odontology translates to the use of implant prosthesis, and while they have similar points they also have some big differences. The most important difference is the biomechanical behaviour of the implant-prosthesis conjunct and the way to convey the stress to the crestal bone. The absence of periodontal ligament and the anchylotic union between the bone and the implant may generate a great force in the crestal bone and we can think how this increase produces a major bone resorption.
In relation to these differences between the length of the restorations and implants it would appear to indicate a bad biomechanical behaviour of the assembly with impact on the marginal bone loss and increasing the rate of failure. To analyse the studies published in relation to this topic, they do not show how a greater bone loss in high crown-implant ratios and ratios higher than two has been considered a safe and predictable therapeutic option 2–5.
The aim of this study was to evaluate the effect of the CI ratio on the marginal bone stability around extra-short implants supporting a fixed-partial prosthesis in posterior mandible. The secondary outcome was to the
implant survival.
Material and methods
This manuscript was written according to the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines 6. All described data and treatments were obtained from a single dental clinic in Vitoria, Spain. Patients’ records were retrospectively reviewed to identify patients that fulfilled the following inclusion criteria:
Aged over 18 years old
Placement of extra-short (length ≤ 6.5 mm) implants before December, 2010
Placed in posterior mandible.
The principal outcome was the marginal bone loss and the secondary outcome was the implant survival rate.
Patients or implants that did not meet any of these criteria were excluded from the study. Prior to surgery, and in order to make a proper treatment plan, all patients underwent standard diagnostic protocol consisting of reviewing the medical and dental history, diagnostic casts, and radiographic evaluation.
To assess the principal and secondary outcomes, implants were followed clinically and radiographically to identify the crestal bone loss and implant failure (failure to achieve osseointegration or loss of acquired osseointegration).
The measurement of the marginal bone loss was performed on the most recent radiograph. To do that, known implant length was used to calibrate the linear measurements on the radiograph. Then, the distance between the uppermost point of the implant platform and the most coronal bone-implant contact was measured mesial and distal to the implant by computer software (Sidexis, Sirona, USA). The bone level recorded just after the placement of the provisional prosthesis served as a reference for the measurement of the marginal bone loss. The bone loss was measured mesially and distally to the implant. Finally, a mean of the two measurements were reported due to the absence of statistically
significant differences.
The crown-implant ratio was determined by two measurements: the crown was measured from the tip of the highest cusp to the platform of the implant, along a perpendicular line. The implant was then measured at the centre, from the platform to the end of the apex (Figure 1).
In all patients, the same surgical protocol was followed. Before surgery, patients underwent a routine dental scaling to start the implant treatment with adequate periodontal health. Radiographic evaluation was also performed to establish the treatment plan. All patients received prophylactic antibiotic medication before and after surgery. An infiltrative anaesthesia was applied and incisions were made to elevate a full-
thickness flap.
Implant sites were prepared using a low-speed drilling procedure (125 rpm) without irrigation 7,8. Before installation, implants were carefully embedded in liquid Plasma Rich in Growth Factors (PRGF) prepared from patient’s blood according to a protocol developed by the manufacturer (PRGF-Endoret, Biotechnology Institute BTI, Vitoria, Spain) to bioactivate the implant surface.
For placing the dental implant, the surgical motor was set at 25 Ncm and the implants were finally seated manually by a calibrated torque wrench. The final insertion torque was annotated in the patient’s record.
A prosthodontist performed the prosthetic rehabilitation of the patients. Impression copings were placed and an impression was made with polyether impression material (Impregum Penta; 3M ESPE) and the open-tray technique at three months after implant insertion.
The follow-up visits were scheduled for a series of periodic evaluations, consisting normally of visits at one week after intervention, at one month, at three months, at six months, and from this moment ahead, once a year.
- Figure 2. Location, diameter and length of the implants included in the study
- Figure 3a. Intraoral pictures of the patient. In these images we can see the partial edentulism in mandible and total edentulism in the maxillae. A) front view B) lateral view
- Figure 3b. Intraoral pictures of the patient. In these images we can see the partial edentulism in mandible and total edentulism in the maxillae. A) front view B) lateral view
- Figure 4. Initial panoramic X-Ray
- Figure 5. Planification of dental implants in the cone-beam with the software BTI-Scan III
- Figure 6. Image of the implant surgery where we can see the insertion of an implant extra-short in the most distal area of the fourth quadrant. The extreme bone resorption at this level requires the implementation of a technique of vertical growth
- Figure 7. Post-operative Rx. In the area of the extra-short implant we can see the bone volume used for the vertical growth
- Figure 8. Panoramic X-Ray at one year follow-up post loading. In the fourth quadrant we can observe the crown-implant ratio of the extra-short implant
- FIGURE 9 X-ray of the follow-up to seven years. We can see the stability of the bone at crestal level
Statistical analysis
Data collection and analysis was performed by two independent examiners. The patient was the statistical unit for the statistical description of demographic data, social habits and medical history. The implant served as the statistical unit for the descriptions of implant length, diameter, location, insertion torque, marginal bone loss and survival of the implants. Absolute and relative frequency distributions were calculated for qualitative variables and mean values and standard deviations for quantitative variables. The Shapiro-Wilk test was selected to check the normal distribution of the data.
The cumulative survival rate of implants were analysed using a life-table analysis (Actuarial method). SPSS v15.0 for Windows statistical software package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
In this study, 32 patients participated with 46 implants with a Crown-implant ratio higher than 1. The patients’ mean age was 68 ± six years (range: 55 to 74 years) at the time of surgery and 78.3 per cent of the patients were females.
Three patients were smokers (4.8 per cent), and none of them referred alcohol habits. One of the patients was diabetic (1.6 per cent), seven patients had previous periodontal disease (11.1 per cent), one patient had previous radiation (1.6 per cent).
The diameter, length and position of the implants included in the study are shown in Figure two. The mean of the follow-up was 23 ± eight months (range 14 to 43). The mean crown-implant ratio was 2.4 ± 0.47 (range 1.50-3.64).
Regarding the type of prosthesis, all patients were rehabilitated using fixed-partial prosthesis. In total, 67.4 per cent of the restorations were screw-retained prosthesis and the rest were cemented.
The measurement of marginal bone loss (MBL) was performed at 12 and 24 months of loading. The mean of mesial bone loss was 1.04 ±0.70 mm and the mean distal bone loss was 0.94 ± 0.71 mm. There was no statistically significant difference between the MBL measurements at different follow-up times (p > .05), indicating that bone level around implants under functional loading was stable over time. No significant influence was found between the CI ratio and MBL, even considering separately CI < 2 and CI ≥ 2.
The overall survival rates of short implants and prosthesis were 100 per cent for the implant and patient-based analysis, respectively, at the end of the follow-up time. In figures three to 10 we show a case of the patients included in the study.
Discussion
The prosthetic rehabilitations in which short implants are involved often lead to imbalances between the lengths of the crowns and the implants. It has been suggested that disproportionate prosthetic restorations could induce poor biomechanical behaviour with a potential impact on MBL and reduced implaent survival rate 9. In this study, no associations between CI ratio of implant-supported prostheses in extra-short implants and MBL were found. Previous studies in which short implants were used have evaluated the influence of CI ratio on marginal bone loss (MBL) 10–12. In general, most of these studies concluded that no relation may be established between an unfavourable CI ratio and MBL, independently of the type of prosthetic rehabilitation 10–12.
All the implants included in this study were splinted restorations. Short and extra-short implants have shown better biomechanical behaviour when the prosthesis have been splinted. An additional rationale for splinting implant crowns together is to favourably distribute the non-axial loads, minimising their transfer to the restoration and supporting bone, and increasing the total load area 13,14. Splinting the crowns reduced the peri-implant bone stress under horizontal load in a finite element analysis model especially recommended for implants surrounded by poor-quality bone 13,15.
When placing extra-short implants, it is necessary to carry out adequate planning and the splinting implants are a correct protocol in these cases 16,17.
Conclusions
Within the limitations of this study, the results show that an increased crown-to-implant ratio in extra-short implants has no significant influence on crestal bone loss and implant survival. The limitations of this study include its retrospective design, the small sample size and short follow-up time. Further studies with more extra-short implants followed for a longer period of time are necessary to establish sound conclusions about the effect of increased crown-to-implant ratio on implant survival.
About the author
Eduardo Anitua DDS, MD, PhD graduated with a degree in medicine and surgery from the University of Salamanca and gained his PhD in medicine from the University of Valencia. He holds a specialism in stomatology from the University of the Basque Country (UPV/EHU) and a diploma in prostheses and occlusion from the Pankey Institute (Florida, USA). He is a visiting professor at more than 20 universities in the USA (Harvard, Boston, Tufts, Pennsylvania, New Orleans), Germany (Berlin), England (Bristol), Italy (Milan, Turin), India, Mexico, Brazil, Portugal, Argentina, Colombia, Venezuela, Uruguay and Spain (Seville, Madrid, Barcelona, Murcia). Dr Anitua has published more than 200 papers in national and international journals, is the author of eight books and co-author of seven books and chapters translated into various languages. He has 37 international patents developed in regenerative therapy and oral implantology.
References
1. Gonçalves TM, Bortolini S, Martinolli M, Alfenas BF, Peruzzo DC, Natali A, Berzaghi A, Garcia RC. Long-term Short Implants Performance: Systematic Review and Meta-Analysis of the Essential Assessment Parameters. Braz Dent J. 2015;26:325-36.
2. Rokni S, Todescan R, Warson P, Pharoah M, Adegbembo AO, Deporter D. An assessment of crown-to-root ratios with short sintered porous-surfaced Implants supporting prostheses in partially edentulous patients. INT J ORAL MAXILLOFAC IMPLANTS 2005;20:69–76
3. Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin. Oral Impl. Res. 18, 2007; 707–714
4. Schneider D, Witt L, Ha ̈mmerle CHF. Influence of the crown-to-implant length ratio on the clinical performance of implants supporting single crown restorations: a cross- sectional retrospective 5-year investigation. Clin. Oral Impl. Res. 23, 2012;169–174.
5. Sanz M, Naert I; Working Group 2. Biomechanics/risk management (Working Group 2). Clin Oral Implants Res. 2009;20(suppl 4):107-111.
6. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-1457.
7. Anitua E, Alkhraisat MH, Pinas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat.
8. Anitua E, Carda C, Andia I. A novel drilling procedure and subsequent bone autograft preparation: a technical note. Int J Oral Maxillofac Implants 2007; 22: 138-145.
9. Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the pos- terior region. II: influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin Oral Implants Res 2007; 18:707–714.
10. Rokni S, Todescan R, Watson P, Pharoah M, Adegbembo AO, Deporter D. An assessment of crown-to- root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants 2005; 20:69–76.
11. Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006; 21:275–282.
12. Birdi H, Schulte J, Kovacs A, Weed M, Chuang SK. Crown- to-implant ratios of short-length implants. J Oral Implantol 2010; 36:425–433.
13. Nissan J, Ghelfan O, Gross O, Priel I, Gross M, Chaushu G. The effect of crown/implant ratio and crown height space on stress distribution in unsplinted implant supporting restorations. J Oral Maxillofac Surg 69:1934-1939, 2011
14. Nissan J, Ghelfan O, Gross O, Priel I, Gross M, Chaushu G. The effect of splinting implant-supported restorations on stress distribution of different crown-implant ratios and crown height spaces. J Oral Maxillofac Surg 69:2990-2994, 2011
15. Grossmann Y, Finger IM, and Block MS. Indications for Splinting Implant Restorations. J Oral Maxillofac Surg 2005; 63:1642-1652.
16. Anitua E, Piñas L, Orive G. Retrospective study of short and extra-short implants placed in posterior regions: influence of crown-to-implant ratio on marginal bone loss. Clin Implant Dent Relat Res. 2015;17:102-10.
17. Anitua E, Alkhraist MH, Piñas L, Begoña L, Orive G. Implant survival and crestal bone loss around extra-short implants supporting a fixed denture: the effect of crown height space, crown-to-implant ratio, and offset placement of the prosthesis. Int J Oral Maxillofac Implants. 2014;29:682-9.
A narrow diameter implant is an implant with a diameter less than 3.75mm and is clinically indicated to replace maxillary lateral incisors and mandibular incisors1. The availability of interdental space less than 6mm and/or residual bone width less than 5mm are also indicative for the use of narrow diameter implant (NDIs)1.
NDIs have significantly reduced the need for bone grafting among completely edentulous patients2. This would permit the avoidance of complications associated with alveolar bone augmentation such as prolonged healing time, additional costs and increased surgical morbidity2, 4. In a recent study, Pommer et al. conclude that, while little evidence on patients’ preferences towards minimally invasive treatment alternatives as opposed to bone augmentation surgery could be identified from within-study comparison, patient satisfaction with graftless solutions for implant rehabilitation of completely edentulous jaws is generally high5.
Long-term survival of the narrow implants in posterior areas of the maxilla and mandible is not well documented. A recent study with this type of implants in areas with combination of split crest technique seems to indicate a successful implant survival rate (97 per cent)6.
Ortega-Oller et al. in a meta-analysis have shown that narrower implants (<3.3mm) have significantly higher failure rates than wider implants (≥ 3.3mm)7. This could be influenced by other variables such as type of prosthesis, implant surface, and timing of prosthetic loading7. Klein et al. in a recent systematic review reported that the survival rate of implants with a diameter < 3mm were higher than 90 per cent with a follow-up time of between one and three years8. For implants with a diameter between 3.0 and 3.25mm the survival rate was higher than 93.8 per cent (follow-up of one to five years). Those implants with a diameter ≥ 3.3mm had a survival rate of 88.9 per cent to
100 per cent with a follow-up time of one to 12 years. The most common causes of implant failure have been lack/loss of osseointegration and infection1, 9, 10.
From the above, NDIs have a comparable success rate as wider implants not only in the anterior region but also in the posterior regions.
For that, this study was conducted to analyse the long-term outcomes of using 2.5mm NDIs as definitive implant for rehabilitation of missing teeth in posterior areas.
Material and methods
This article was written following the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines11 and included patients treated at a single dental clinic in Vitoria, Spain. Patients included in the study fulfilled the following criteria:
- Both genders and over 18 years old
- Patients with totally or partially edentulous jaws who were treated by one or more 2.5mm narrow-diameter implants due to insufficient bone ridge thickness (< 5mm) and/or reduced mesio-distal space (< 6mm)
- Implants inserted before July 2005
- Implants inserted in posterior areas (premolar
and molar) - A retrospective cohort study design was used.
Data collection
Patient records were analysed to derive demographic data (gender, age), social habits (smoking, alcohol intake), relevant medical conditions, and history of periodontal disease. Then a database was conformed with implants data (length, diameter, and insertion torque) and localisation.
For implant survival assessment, implant failure was considered any implant lost due to biological (failure to achieve osseointegration or loss of acquired osseointegration) or biomechanical causes.
For Marginal Bone Loss (MBL) quantifications, marginal bone levels were measured on the periapical radiograph made just after the surgery and the last available periapical radiograph. The radiographs were obtained using paralleling technique with a film holder (Superbite, KerrHawe, Barcelona, Spain).
Measurements of MBL on the periapical radiographs were performed by computer software (Digora, Soredex, USA), a calibration of the periapical radiograph by a known length (implant length) was performed. Once the radiograph was calibrated to a 1:1 measure, eliminating the possible presence of magnification, measurements were made mesially and distally to the implants, calculating the distance between the uppermost point of the implant platform and the most coronal contact between the bone and the implant. The bone level recorded just after the surgical insertion of the implant was the basal value to compare with subsequent measurements over time.
For prostheses survival assessment, prostheses failure was considered as any complication that led to prosthesis removal (screw loosening/ fracture abutment/ implant fracture/ceramic chipping and prosthesis fracture).
Surgical procedures
All surgeries were made by two experienced surgeons. Before surgery, patients underwent a routine dental scaling to start the implant treatment with an adequate periodontal health. Radiographic evaluation was also performed to establish the treatment plan.
Patients received 2g of amoxicillin (600mg of clindamycin for allergic patients) 60 minutes before surgery and 1g of acetaminophen, 30 minutes preoperatively. Local anesthesia was achieved by the administration of articaine hydrochloride with epinephrine (1:100,000).
Implant sites were prepared using a low-speed drilling procedure (125 rpm) without irrigation12,13. Before installation, implants were carefully embedded in liquid Plasma Rich in Growth Factors prepared from patient’s blood according to a protocol developed by the manufacturer (PRGF-Endoret, Biotechnology Institute BTI, Vitoria, Spain) to bioactivate the implant surface.
Rehabilitations were made by the restorative dentist. In general, healing was allowed for a minimum of three months, after which the healing abutments were fixed. Shortly thereafter, the suprastructure was placed. Immediate loading protocol was applied in four patients (eight NDIs). Implants were loaded immediately only if they achieved an insertion torque of at least 45Ncm.
Post-surgical clinical assessments
Once the surgical phase was conducted, patients were scheduled for a series of periodic evaluations, consisting normally of: one evaluation five to 10 days after intervention, at one month, at three months, at six months, and from this moment ahead, once a year. The post-implant assessment included, at each follow-up visit, different clinical assessments to verify the status of the implant (gingival health, prosthesis mobility, pain, infection, alveolar ridge resorption and any complications).
Moreover, periodic panoramic and periapical radiographs were carried out to verify the implant clinical status in the follow-up period.
Statistical analysis
Data collection and analysis was performed by two independent examiners (other than restorative dentist and surgeon). The patient was the statistical unit for the statistical description of demographic data, social habits, medical history and history of periodontal disease. Mean values, standard deviations, and ranges were calculated for age, while relative frequency was calculated for the remaining patient-related variables.
The implant served as the statistical unit for the descriptions of implant length, diameter, location, insertion torque, marginal bone loss, survival an prosthetic parameters. Absolute and relative frequency distributions were calculated for qualitative variables and mean values and standard deviations for quantitative variables. The survival of implants and prostheses were evaluated with Kaplan-Meier method. SPSS v15.0 for Windows statistical software package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
In this study, a total of 25, 2.5mm narrow-diameter implants placed in 15 patients were included and evaluated. Eighty per cent of the patients were female and the mean age at surgery was 53 ± 9.2 years. Four patients were smokers (20 per cent). The length of the implants ranged between 11.5mm and 15mm. The implants mean follow-up time since insertion was 6.5 ± 3.9 years (range 0 to 9.5 years).
The mean follow-up time of the prostheses was 5.67 years (SD = 36.06). Figure 1 shows the anatomical locations of implants. Fifteen implants (60 per cent) were placed in the maxilla, whereas 10 were placed in the mandible (40 per cent).
Delayed implant loading was performed for 17 implants (68 per cent). The implant loading was performed after eight ± four months since insertion (range: five to 21 months). Five implants (32 per cent) were submitted to immediate loading protocol.
Regarding the type of the prosthesis, 12 implants (48 per cent) were involved in a fixed partial bridges, whereas 12 implants were involved in four screwed complete prostheses (48 per cent), and the one remaining implant was restored with a cemented single crown (4 per cent).
For the assessment of long-term MBL, only those cases where the last available periapical radiograph was performed after at least seven years of insertion were taken into account. Twenty one implants (mean follow-up time of 8.9 ± 0.5 years) that satisfied this requirement were analysed. The mean MBL was 0.64mm at the mesial side (SD = 0.64, range between 0 and 1.95mm), and 0.66mm (SD = 0.62, range between 0.00 and 2.19mm) at the distal side.
The survival rate was 100 per cent for implants. Two prostheses failed during the observation period. The prosthetic complications were porcelain fracture in another patient and connector fracture in other patient. This resulted in prostheses survival rate of 92.0 per cent (Figure 2).
Figure 3 illustrates the clinical situation of a patient involved in the study before and after 10 years of treatment with narrow diameter implants.
- Figure 1. Anatomical location of the narrow diameter implants included in this study
- Figure 2. Cumulative survival rate of the prostheses
- Fig 3a. Post-operative X-ray at the moment of the insertion of the implants
- Fig 3b. Planning in the diagnostic software of the implant insertion
- Fig 3c. Planning in the diagnostic software of the implant insertion
- Fig 3d. X-ray with the final prosthesis at two years
Discussion
Eighty seven per cent of the implants were followed for more than three years and 60 per cent for more than seven years. During the follow-up period, no implants have failed resulting in a survival rate of 100 per cent. In a review, Renouard and Nisand reported an implant survival rate higher than 90 per cent for 3mm and 3.3mm implants14. Sohrabi et al. have similarly concluded that the survival rate of NDIs is generally higher than 90 per cent and that the failure rate appeared to be higher in small-diameter implants less than 13mm in length15. Klein et al. have reported that available studies on dental implants <2.5mm in diameter reported a survival rates between 90 and 100 per cent8.
In a recent meta-analysis by Ortega-Oller et al. the majority of the analysed studies (implants less than 3.3mm in diameter) have also reported a survival/success rate higher than 90 per cent7. However, the results of the meta-analysis have shown higher failure rates for implants with a diameter <3.3mm when compared to implants with a diameter ≥3.3mm. The authors have related this outcome with the fact that NDIs are usually placed in complicated clinical scenario and they have higher possibility of fracture7. Interestingly, according to that review, the failure rate will be more probable if the implants are loaded in a period less than three months since insertion and/or have a smooth implant surface7.
In the present study, the survival rate of NDIs was comparable to standard implants. The high survival rate of the NDIs could be related to the fact that the implants placed in this study had a roughened surface. Furthermore, 26 implants were loaded after eight months (± four months) since implant insertion and no one of these had failed.
Abutment screw loosening is one of the most common prosthetic complications that was being reported by clinical studies on NDIs8. This complication could be the result of different factors such as component misfit, inadequate tightening, settling of the screw, inadequate screw design and excessive loading16. The absence of screw loosening in this long-term follow-up could related to the fact that all implants (except one) were splinted by a fixed prostheses.
Splinting multiple implants has been reported to minimise the lateral force on the prosthesis, to enhance force distribution, and to reduce the stress on the implants17,18. Thus, splinting of 2.5-diameter implants would protect the implants from excessive loading and prevent implant/abutment screw fracture.
In this study, all the implants were inserted in posterior areas. In this type of rehabilitation, the risk of ‘fatigue’ fractures of the implants exists19,20. Freitas-Junior et al. have concluded in a biomechanical study that a single NDI is less reliable than a standard implant or two NDIs to support single crown in the molar region21. In our study, the survival of implants were 100 per cent and there were no biomechanical complications with the implants.
The measurement of marginal bone loss around the NDIs had a mean value below 1mm for the implants with follow-up time more than seven years since insertion. This would indicate the absence of excessive mechanical loading on the 2.5mm diameter implants. Similar results have been reported by Wang et al.22.
This study suffers from the limitation of a retrospective study design and the small sample size. The retrospective study provides evidence of lesser strength than the evidence derived from prospective or randomised clinical trial. There is also a dependency on the availability and accuracy of medical/dental records.
Conclusions
The use of narrow diameter implants in narrow alveolar ridges in posterior areas could constitute a minimally invasive alternative to bone augmentation surgery. NDIs of 2.5mm have resulted in a high survival rate in a long-term follow-up. This outcome could be related to the fact that these implants have all been splinted to other implants by a fixed prosthesis. This prosthetic configuration may have minimised the probability of implant and prosthesis failure.
References
1. Andersen E, Saxegaard E, Knutsen BM, Haanaes HR. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int J Oral Maxillofac Implants 2001; 16: 217-224.
2. Papadimitriou DE, Friedland B, Gannam C, Salari S, Gallucci GO. Narrow-Diameter versus Standard-Diameter Implants and their Effect on the Need for Guided Bone Regeneration: A Virtual Three-Dimensional Study. Clin Implant Dent Relat Res.
3. Anitua E, Alkhraisat MH, Orive G. Novel technique for the treatment of the severely atrophied posterior mandible. Int J Oral Maxillofac Implants 2013; 28: 1338-1346.
4. Esposito M, Cannizzaro G, Soardi E, Pellegrino G, Pistilli R, Felice P. A 3-year post-loading report of a randomised controlled trial on the rehabilitation of posterior atrophic mandibles: short implants or longer implants in vertically augmented bone? Eur J Oral Implantol 2011; 4: 301-311.
5. Pommer B, Mailath-Pokorny G, Haas R, Busenlechner D, Furhauser R, Watzek G. Patients’ preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. Eur J Oral Implantol 2014; 7 Suppl 2: S91-109.
6. Garcez-Filho J, Tolentino L, Sukekava F, Seabra M, Cesar-Neto JB, Araújo MG. Long-term outcomes from implants installed by using split-crest technique in posterior maxillae: 10 years of follow-up. Clin Oral Implants Res. 2015 Mar;26(3):326-31.
7. Ortega-Oller I, Suarez F, Galindo-Moreno P, Torrecillas-Martinez L, Monje A, Catena A, Wang HL. The influence of implant diameter on its survival: a meta-analysis based on prospective clinical trials. J Periodontol 2014; 85: 569-580.
8. Klein MO, Schiegnitz E, Al-Nawas B. Systematic review on success of narrow-diameter dental implants. Int J Oral Maxillofac Implants 2014; 29 Suppl: 43-54.
9. Polizzi G, Fabbro S, Furri M, Herrmann I, Squarzoni S. Clinical application of narrow Branemark System implants for single-tooth restorations. Int J Oral Maxillofac Implants 1999; 14: 496-503.
10. Zinsli B, Sagesser T, Mericske E, Mericske-Stern R. Clinical evaluation of small-diameter ITI implants: a prospective study. Int J Oral Maxillofac Implants 2004; 19: 92-99.
11. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453-1457.
12. Anitua E, Alkhraisat MH, Pinas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat.
13. Anitua E, Carda C, Andia I. A novel drilling procedure and subsequent bone autograft preparation: a technical note. Int J Oral Maxillofac Implants 2007; 22: 138-145.
14. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res 2006; 17 Suppl 2: 35-51.
15. Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res 2012; 23: 515-525.
16. Patil PG. A technique for repairing a loosening abutment screw for a cement-retained implant prosthesis. J Prosthodont 2011; 20: 652-655.
17. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent 2010; 30: 89-95.
18. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res 2003; 5: 254-262.
19. Chiapasco M, Casentini P, Zaniboni M, Corsi E, Anello T. Titanium-zirconium alloy narrow-diameter implants (Straumann Roxolid) for the rehabilitation of horizontally deficient edentulous ridges: prospective study on 18 consecutive patients. Clin Oral Implants Res 2012; 23: 1136-1141.
20. Davarpanah M, Martinez H, Tecucianu JF, Celletti R, Lazzara R. Small-diameter implants: indications and contraindications. J Esthet Dent 2000; 12: 186-194.
21. Freitas-Junior AC, Bonfante EA, Martins LM, Silva NR, Marotta L, Coelho PG. Effect of implant diameter on reliability and failure modes of molar crowns. Int J Prosthodont 2011; 24: 557-561.
22. Wang HL, Okayasu K, Fu JH, Hamerink HA, Layher MG, Rudek IE. The success rate of narrow body implants used for supporting immediate provisional restorations: a pilot feasibility study. Implant Dent 2012; 21: 467-473.
About the author
Eduardo Anitua DDS, MD, PhD graduated with a degree in medicine and surgery from the University of Salamanca and gained his PhD in medicine from the University of Valencia.
He holds a specialism in stomatology from the University of the Basque Country (UPV/EHU) and a diploma in prostheses and occlusion from the Pankey Institute (Florida, USA).
He is a visiting professor at more than 20 universities in the USA (Harvard, Boston, Tufts, Pennsylvania, New Orleans), Germany (Berlin), England (Bristol), Italy (Milan, Turin), India, Mexico, Brazil, Portugal, Argentina, Colombia, Venezuela, Uruguay and Spain (Seville, Madrid, Barcelona, Murcia).
Dr Anitua has published more than 200 papers in national and international journals, is the author of eight books and co-author of seven books and chapters translated into various languages. He has 37 international patents developed in regenerative therapy and oral implantology.
Salivary diagnostic tests of periodontal diseases
The risk of anti-fungal resistance in dentistry: lessons from a Japanese fungus
Globally since 2009, Candida auris, a fungal species closely related to Candida albicans, has been responsible for a number of… Read more
The anxious patient: Empathy, planning and a team-approach
[ Words: Ilyaas Rehman, BDS (Glas) ] Introduction Introduction This case report documents the treatment provided for a very anxious… Read more
Meaningful milestone
Consultation represents the next step on the journey towards achieving a more effective system of CPD Some dental professionals feel… Read more
Top tips for practicing evidence-based dentistry: Part 3
Introduction Implementing the best available evidence and enabling positive sustainable change in practice is an enviable goal for anyone providing… Read more
The management of a paediatric dental avulsion in general dental practice
Abstract A paediatric dental avulsion is not a clinical scenario that you will be faced with on a daily basis… Read more
Intraoral scanners In dentistry – an update on digital technology
With the introduction of the first intraoral scanner, CEREC (Chairside Economical Restoration of Esthetic Ceramics) by Dentsply Sirona in 1985,… Read more
CBCT and clinical decision-making
Arvind Sharma, BDS(Dund), MSc(Endo), MJDFRCS(Eng), MFDSRCPS(Glas) Arvind Sharma presents the second and final part of a structured critical review to… Read more
Problems of a phobic patient
Day One Ms B attends as a new patient at a local dental surgery complaining of sensitivity in a number… Read more
The power of regeneration
Due to its powerful regenerative properties, platelet rich growth factor Endoret (PRGF) is being increasingly used in many fields of… Read more
Suitability of patients for conscious sedation
Patients suitable to undergo conscious sedation (CS) include those with moderate-severe anxiety, a swallow/gag reflex or a mild learning/physical disability… Read more
Top tips for practicing evidence-based dentistry
In the first article, we explored how to establish a research question using the PICO (Population, Intervention, Comparator and Outcome) method… Read more
Quick, aesthetic restoration
A new patient in her early 30s attended for a check-up. A routine radiograph revealed caries under the amalgam filling… Read more