Evidence-based dentistry in practice
Niall McGoldrick and Derek Richards present the first part in a series of articles looking at how dental professionals can identify, use and maximise evidence-based dental research in their everyday practice
This article is the first in a series that aims to introduce the modern-day dental practitioner to evidence-based dentistry (EBD). After reading this series, you will be clearer about how to keep abreast of the ever-growing evidence base and the latest guidance. You will know where to look for evidence and learn how to maximise time spent searching for evidence to inform your practice.
In our day-to-day lives, we have become accustomed to using search engines such a Bing or Google to help answer simple questions, but, when it comes to our clinical work and professional life, we need to take a more formal approach in our search. There are a number of web-based scientific databases that catalogue evidence. The databases can be thought of as massive online libraries, but like any library, if you don’t know your way around it or the cataloguing system used, then you are likely to get lost and spend hours searching for what you need. Therefore, having an awareness of the different scientific databases available and understanding how to use them is a good starting point.
An example of a well-known database, and one you may have already used is PubMed. Simply typing the word ‘dental’ into the search box on PubMed results in more than half a million hits – 516,870 to be precise. These 516,000 hits are spread over 25,844 pages, which makes for a lot of reading. Clearly, we need a more focused approach. So, what then if we pick a subject within dentistry such as fluoride varnish? This search still returns 1,293 hits spread over 65 pages.
The point we are demonstrating here is that there is a wealth of information and publications that we can make use of, but there is some skill required to negotiate databases and identify quality evidence. A busy practitioner needs access to high-quality evidence quickly and easily.
Evidence-based dentistry
The American Dental Association describe EBD as “an approach to oral healthcare that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient’s oral and medical condition and history, with the dentist’s clinical expertise and the patient’s treatment needs and preferences.”[1]
As dentists we want to do our best for each and every patient we treat, and this is at the heart of EBD. Most dentists will be confident in their clinical skills and will listen to patients but not all will be confident in the strength of evidence behind how and what they practice. The evidence should be a constant go to for a modern-day dentist.
Developing an evidence-based approach can be thought of in five stages:
- Asking the right question
- Searching for the best available evidence
- Critically appraising the evidence
- Applying the evidence
- Evaluating the outcome.
In your life outside of the surgery, you will already be using this approach, whether you realise it or not. Take buying a new car, for example. Let’s say it is a used car; you may not want to rely solely on the sales person’s word that the shiny car on the forecourt really is the best one for you. You will need to think about what it is you really need from the car – is a sporty convertible with two seats and no boot space going to suit your lifestyle? Maybe it is.
Most people will search the internet comparing various cars on independent websites; they will look in magazines or speak to friends and family beforehand. So, when you arrive at the showroom you already have an idea of what you are looking for and what you need from a car. At this point, you have carried out the first stage of an evidence-based approach: Asking the right question. You have also begun the second stage: Searching for the best available evidence.
When you have identified a potential car, you will want to continue your search for evidence to support your decision to buy. You will want to know more details about the service history, you might inspect the paintwork, check how many miles it has done and ask about previous owners. You will combine this information with what you found out previously and check the quality of the evidence before you. This is stage three: Critically appraising the evidence.
Next comes the big decision; whether to go ahead with the purchase. After carefully considering all the evidence you have available, you may or may not decide to buy the car, this is stage four: Applying the evidence.
The final stage is evaluating the outcome. This will take place in the months and years to come when you will be driving the car. If the car keeps breaking down and needs multiple new parts, you might question your approach and the evidence upon which you based your decision.
In this article we will cover stages one and two of the evidence-based approach.
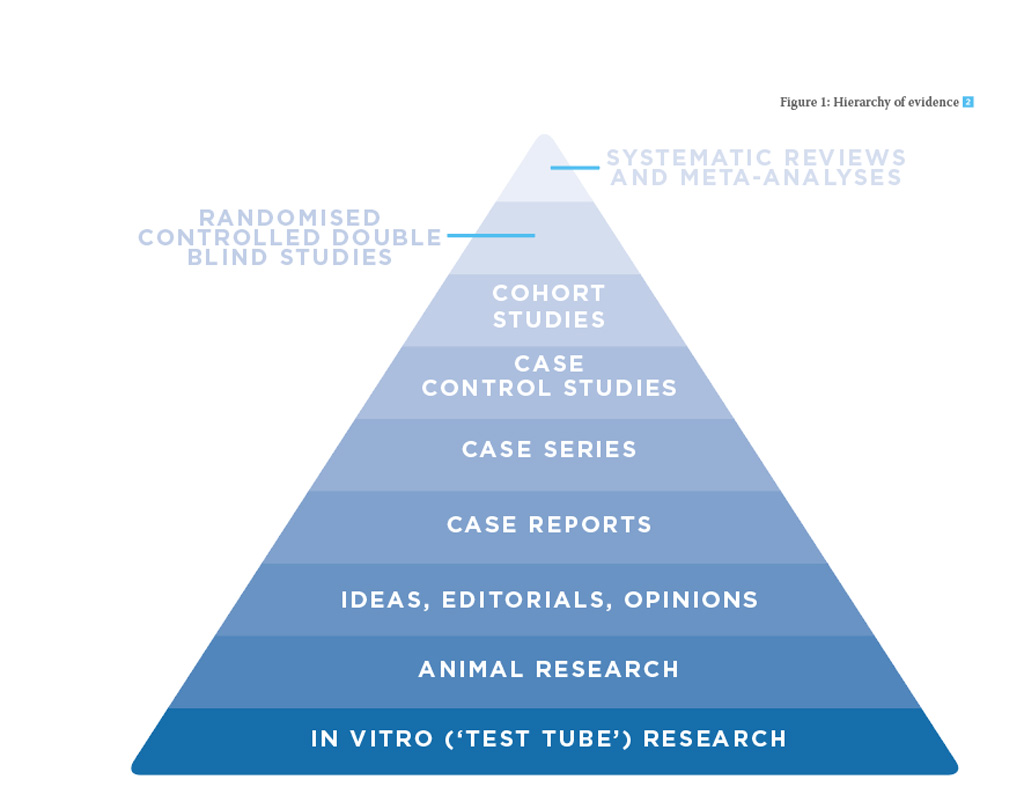
Figure 1: Hierarchy of evidence [2]
Asking the right question
Evidence-based dentistry starts with a clinical question. You need to be clear about what it is you are trying to find evidence for. A good technique to help develop your question is to use PICO.
What is PICO?
PICO is an acronym for Population, Intervention, Comparator and Outcome. It is used when developing a question regarding a clinical scenario. Say, for example, you are a general dental practitioner; you suggest that the five-year-old patient in your chair should have fluoride varnish applied to her teeth. The patient’s parent questions this; he asks you “what good will it do?”, and at this point, he does not provide consent.
Using the PICO approach, we can build our question and start our search for the evidence. First of all, we need to establish the key population group that we want to find evidence about. In this case, it is children.
Next, we need to think about what treatment we are proposing and what the alternative might be. Here, we are proposing fluoride varnish application and the comparison would be no fluoride varnish. You could also choose an active treatment for comparison, such as fluoride mouthwash or toothpaste. Having an alternative prevention option might help win over the parent in this scenario.
Having a clear idea about what outcome you want from the treatment is important. Here, our key outcome is the caries rate in the child.
As a result of this process, we now have a PICO question we can use in a database search:
- Population, patient or problem: Children
- Intervention or treatment: Fluoride varnish
- Comparison: No treatment
- Outcome: Caries.
Searching for the best available evidence (AQUIRE)
We now have a clear PICO question for moving forward with and have completed stage one. In the next stage, we need to think about the types of evidence there are and where we can find them.
This section will aid you in the search for the best available evidence. It has two parts. In the first part we will explore the hierarchy of evidence and the uses for each type, while the second part published in the next article, will take you through the practicalities of different databases.
Types of evidence
First let us think about the different types and levels of evidence available. The most common and easy way to think about evidence is as a pyramid or hierarchy as shown in Figure 1 on the previous page.
It is quite intuitive, with the highest levels of evidence found at the top of the pyramid. Each type of evidence has a role to play in shaping healthcare. We will work our way up the pyramid discussing each of the types of evidence in turn while exploring the pros and cons of each.
In vitro/animal research
Animal and in vitro research can be useful in the initial stages of developing treatment, for example when exploring causes behind disease or investigating an early idea or hypothesis.
The dental materials we use are initially tested in the lab. If they fail at this stage then there would be no point in testing the material in humans without overcoming the initial flaws identified.
With animal experiments there can be an issue when it comes to translating or replicating findings in humans. Some treatments may never work or they may actually be harmful to humans. The process of getting from the lab bench to chair side can take decades of refinement.
In this article, our focus is on what works best in the clinical situation and therefore this type of lab-based study is not immediately transferable into practice.
Ideas, editorials and opinions
Initially, most people think their own ideas are great but do they stand up to the scrutiny of others? As we mentioned above, ideas need testing. Personal opinions and written editorials often only provide one view point. Therefore, it would not be a good idea to change your practice based on a discussion over a cup of coffee or on a single editorial on a website, magazine or journal.
There are occasions when a combined opinion can be useful though. Sometimes professional groups come together to give an opinion or stance on a particular issue. This often involves bringing together a range of currently available evidence. The downside is that the opinion will include some of the group’s own biases.
A recent example of a professional group summarising evidence is the Scottish Consultants in Dental Public Health Group, Recommendations on the use of fluoride toothpaste and fluoride supplements in Scotland 2017[3]. The document is clearly referenced and has been produced in consultation with a renowned guideline development group. This type of opinion holds more weight and can be taken more seriously.
Case reports/Case series
A large number of articles published in dental journals tend to be case reports or case series. They are based on one or very few cases. Treatment is often provided by one practitioner with a particular special interest or expertise. It may be difficult to directly replicate the treatment situation. Also, the patient characteristics are unlikely to be exactly the same as your patient.
They are particular useful in the case of rare or serious events. A case series published in 2012 presented two cases of fatal anaphylaxis following irrigation of tooth extraction sockets with chlorhexidine[4]. Rare events such as this can change practice very rapidly.
Case-control studies
Case control studies are retrospective observational studies. They do not test an intervention but are used to help find out what might cause a disease or be associated with it. As the name suggests, they are made up of two different groups, cases and controls. Cases will have the particular disease of interest and will be compared to controls that do not have the disease of interest. Researchers will take extensive histories from both groups and compare factors such as lifestyle. They are useful for establishing risk factors that are associated with a disease.
Recently there has been a lot of interest in understanding the causes of dementia. With an ageing population, if we could find out how to prevent dementia then this could have a great impact on the health of the population. One hypothesis queries whether periodontitis has any association with dementia. A research group in Granada carried out a case control study to find out if there was such an association. They compared 180 people with cognitive impairment to 229 without any impairment. After controlling for known risk factors they found there was a statistically significant association between periodontitis and dementia[5].
As mentioned before, case control studies are useful for establishing if associations exist between risk factors and disease. A lot more evidence is required in order to prove causation and establish the sequence. In this example, one might question whether the periodontal disease came before the dementia or whether the patient developed dementia and then stopped brushing as well as before? If you want to learn more about causation, then a good starting point is to read about the work of Sir Austin Bradford Hill. Sir Bradford Hill was an epidemiologist during the 19th century, in an after dinner speech he set out a number of considerations that should be taken into account when trying to establish causation[6].
Cohort studies
Cohort studies are another form of observational study and are much more useful in establishing causes of disease. As the name suggests, they include a cohort of people with all the subjects included in the study initially free from the disease of interest. Detailed histories and in some cases examinations take place at the beginning of the study. The cohort is then followed up, often over a number of years, and observed for signs of the disease.
One of the most famous cohort studies took place in the US in a town called Framingham. The town in Massachusetts was to be the centre of a study that has now lasted 69 years. It focused on understanding the causes of cardiovascular disease as public health specialists recognised this as a major threat to the population of the US. People in the town who were free of cardiovascular disease were enrolled in the study and observed for many years. Detailed information on behaviour, lifestyle and other characteristics were recorded. Investigations including blood pressure monitoring and ECG’s were carried out as the study progressed. It took 10 years for the first key finding to emerge. The researchers were able to show that as blood pressure increased, the incidence of coronary heart disease also increased[7]. The study produced the foundations of preventative medicine and discovered many of the causes for heart disease that we aim to prevent today.
Randomised controlled trials
A randomised controlled trial is the study of choice for testing new interventions in dentistry. They are experimental in nature and use randomisation techniques to reduce risk of bias and confounding factors that may influence outcomes. Patients are selected against strict inclusion and exclusion criteria ensuring they have similar baseline characteristics. There are then randomised into two arms, treatment and control. In the treatment arm, the subjects receive the new treatment under investigation. This is compared to the subjects in the control arm who will receive either placebo or current standard therapy.
Using a randomisation process to allocate patients to the different arms of a trial reduces the risk of selection bias, which is present when there are systematic differences between baseline characteristics of the groups being compared. Randomisation is best done using a computer-generated sequence that is independent of influence from the investigators. A trial that conceals group allocation from both the patient and the investigator is described as double-blind, in that neither know if they are receiving the new treatment or the alternative be that a placebo or standard care. At the end of the trial, the outcomes from each arm are then compared for any differences and inferences drawn on whether the treatment is effective.
There have been many randomised controlled trials (RCT) in dentistry, all of varying standards. Although an RCT is high in the hierarchy of evidence, it is still important to critique how the research was carried out and to what standard. We will cover that in article two.
Systematic reviews
The highest level of evidence is a systematic review. They bring together all the existing evidence on a particular question. Systematic searches of the literature are initially broad and can result in thousands of hits on databases such as PubMed. The review team will set criteria to focus the review down to include studies that answer specific questions. They then carry out critical appraisal of the studies to assess quality. If the studies all measure similar outcomes then the results of the trials can be compared by extracting the data and using statistical techniques in a meta-analysis. This gives more weight to the studies.
Guideline development groups
Guidance documents aim to bring together the current best available evidence on a given topic and make recommendations. National Guidance Groups such as Scottish Dental Clinical Effectiveness Programme, Scottish Intercollegiate Network and the National Institute for Clinical Excellence comprise a team of expert researchers and clinicians. They have a formal methodical approach to appraising the evidence; they combine this with expert opinion to arrive at their recommendations. We will look more at guidance and the influence they have on practice in the next article, which will feature an interview with Dr Doug Stirling from SDCEP.
Conclusion
So now we have reached the top of the pyramid and it should be becoming clear that there is a wealth and variety of information out there. We should be mindful of what evidence exists for the treatment we are providing our patients. Each type of study or research has its own pros and cons. The next article will focus on the practicalities of where to find the evidence, how to get the most out of databases and, importantly, how to critique the evidence you find.
Get involved
General dental practitioners have opportunities to get involved in clinical trials, especially in Scotland. A number of trials have been run from the University of Dundee including the IQuad trial which is an acronym for Improving the Quality of Dentistry. This trial looked at the effectiveness of the simple scale and polish on periodontal disease with published results expected soon. Find out more here.
The FiCTION trial, again it is an acronym, which stands for Fillings in Children Teeth Indicated or Not. Find out more here.
Recruitment to the latest clinical trial called REFLECT is ongoing. The trial is focused on understanding more about the effectiveness of 5000ppmf toothpaste. Dr Carly Ross BDS (Gla) MJDF (RCSEng), clinical research fellow and honorary specialty registrar in special care dentistry at the University of Dundee Dental School, explains about the role of general dental practitioners in helping shape the evidence.
Why does evidence-based dentistry matter to a general dental practitioner?
General dental practitioners have an important role to play in evidence-based dentistry. Along with the current scientific evidence and the patient’s needs, a GDP’s own clinical expertise helps to shape the concept of evidence-based dentistry. From this, clinical guidelines can be produced which assist GDPs in providing high-quality clinical care using the best available evidence.
How can dentists get involved in trials and shaping of the evidence?
Ninety percent of dental care is provided in primary care so it is essential that research is conducted in this setting. Many clinical trials take place in primary care in Scotland so input from GDPs is important to allow high-quality research to be carried out. The REFLECT clinical trial is being carried out in general dental practices and aims to evaluate the effectiveness and cost benefit of prescribing high dose fluoride toothpaste in older adults. The trial is currently recruiting practices in Scotland to take part.
If you are interested in taking part, please email reflect@dundee.ac.uk or call 01382 381 213 for more information.
Editor’s view
The Cochrane Collaboration carry out systematic reviews that include evidence derived mainly from randomised controlled trials. They use strict methodology and techniques for carrying out reviews and they can be thought of as setting the standard of how reviews should be conducted.
Dr Thomas Lamont, clinical research fellow and honorary specialty registrar in restorative dentistry at Dundee Dental School, is a clinical editor with Cochrane. Below he tells us in some more detail about the methods used in a Cochrane review and what his role is.
Who is involved in a Cochrane systematic review?
What is the skill mix?
Cochrane systematic reviews will include multi-disciplinary teams including patient representatives, clinicians, clinical academics, methodologists, statisticians, health economists, editors and
copy editors.
You are a clinical editor, what is your role?
As clinical editor, I help the review groups by providing clinical and methodological advice to the teams. I also help to peer review Cochrane reviews to ensure they meet the required Cochrane standards. I also provide lectures/seminars on the Cochrane review methodology to clinicians and academics.
Why does reviewing the evidence matter?
It is important that we review and integrate the evidence to ensure that we provide the best possible care for our patients. This cannot be done in isolation and needs to be combined with our own clinical experience and the wishes/values of our patients.
What relevance do the results of a Cochrane review have to a general dental practitioner?
Cochrane reviews provide high-quality evidence for use in the field. They add to the evidence base and distil a large amount of information, therefore making it easier for clinicians to make sense of all the
available evidence.
Find out more about Cochrane here: oralhealth.cochrane.org
References
1. American Dental Association. [Online] American Dental Association, 2017.
2. SUNY Downstate Medical Center. Medical Research Library of Brooklyn. Evidence Based Medicine Course. A Guide to Research Methods: The Evidence Pyramid.
3. Scottish Consultants in Dental Public Health Group, read online 24 March 2017. Recommendations on the use of fluoride toothpaste and fluoride supplements in Scotland 2017.
4. Chlorhexidine and hypersensitivity reactions in dentistry. M.N. Pemberton, J. Gibson. s.l.: British Dental Journal, 2012, Vol. 213.
5. Is periodontitis a risk factor for cognitive impairment and dementia? A case-control study. Gil-Montoya JA, Sanchez-Lara, Carnero-Pardo C, Fornieles F, Montes J, Vilchez R et al. Granada: J Periodontaol, 2015, Vol. 86.
6. The Missed Lessons of Sir Austin Bradford Hill. Phillips CV, Goodman KJ. Texas: BioMed Central, 2004.
7. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Syed S mahmood, Daniel Levy, Ramachandran S Vasan, Thoma J Wang. 9921, s.l.: The Lancet, 2014, Vol. 383.
Bibliography
• Derek Richards, Jan Clarkson, Debora Matthews, Rick Niederman. Evidence based Dentistry: Managing Information for Better Practice. London: Quintessence Publishing; 2008.
• Jan Clarkson, Jayne E harrison, Amid I Ismail, Ian Needleman, Helen Worthington. Evidence-Based Dentistry For Effective Practice. London: Martin Dunitz; 2003.
About the authors
Derek Richards BDS, FDS, MSc, DDPH,FDS(DPH), is a consultant in dental public health, editor of the Evidence-based Dentistry Journal and director of the Centre for Evidence-based Dentistry now based at the Dental Health Service Research Unit in Dundee. He holds honorary senior lectureships at Dundee and Glasgow Dental Schools and is a specialist advisor to the Scottish Dental Clinical Effectiveness Programme (SDCEP). He has been involved with a wide range of evidence-based initiatives both nationally and internationally since 1994. He is co-author of the book, Evidence-Based Dentistry: Managing Information for Better Practice (Quintessential of Dental Practice) and the chief blogger for the Dental Elf website.
Niall McGoldrick BDS, MFDS RCPS(Glasg), is a specialty registrar in dental public health and is currently studying for his masters of dental public health at the University of Dundee. He graduated from Dundee Dental School in 2013 and then went onto complete longitudinal dental foundation training and dental core training in a range of specialities in Scotland including a placement with the SDCEP. He is a co-founder of the Scottish Charity, Let’s Talk About Mouth Cancer that is focused on the early detection of mouth cancer. He has received multiple awards for his work both inside and out of the NHS. Most recently, he received a National Award, NHS Young Achiever, from NHS Scotland and Scottish Government.
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings
Comments are closed here.