Seek and ye shall find – part 2
Part two – management and maintenance of implants
In the last issue we reviewed the literature on the validity of the use of periodontal indices to predict peri-implantitis. The conclusions were that current diagnostic tools are ineffective at predicting peri-implant problems, and, moreover, if they are used as an indicator of treatment needs, many patients will receive treatment that is of no benefit1.
To recap:
- The majority of implants will bleed on probing
- Pocket depth of >4mm cannot be used as a sign of pathology
- Increasing pocket depth alone is not an accurate predictor of peri-implant bone loss
- A single episode of bone loss is not an indicator of future bone loss and does not call for treatment, unless associated with other signs of active infection (bleeding and profuse suppuration on palpation)
- Peri-implantitis cannot occur within a year of implant placement as this is the adaptive phase of integration
- Radiographic evaluation of crestal bone levels over time seems to be the most reliable tool to identify those implants undergoing continuous bone loss and therefore in need of treatment.
The above points are uncomfortable as they may challenge what we have previously been taught in the clinical management of dental implants.
The following obvious questions arise:
- Just when should we intervene?
- Which patients really are at risk?
The bottom line, unfortunately, is that we don’t know (Figs 1 and 2). With hindsight it is, of course, easy to look at a failing implant case and postulate as to the probable causes of failure playing the, so called, “blame game”.
Likely suspects
- The patient – poor oral hygiene smoker, diabetic, previous periodontitis, bruxist, aggressive foreign body reaction
- The surgeon – surgical trauma, implant selection, positioning, technique
- The restoring dentist – occlusion, misfit, material/component choice, poor treatment planning.
While all the above factors have, at one time or another, been highlighted in crestal bone loss and failure, in reality what is more likely is, as described by Albrektsson,
a combination of a number of these factors2.
In terms of prevention of peri-implant problems, the “ideal” would be that ALL clinicians involved are experienced and knowledgeable in ALL aspects of dental implant treatment and planning, and are respectful not only of the others’ role but of their own limitations.
For example, while restoring a single tooth implant may appear simple from a technique perspective, the restorative dentist taking on this treatment has as much a role in the long-term survival of the implant as the surgeon. A poorly constructed crown can result in implant failure3.
A multidisciplinary approach can be argued to be the most effective as not only should all potential compromising factors be managed to a higher level, but responsibility is shared. It is essential, however, that such an approach is openly collaborative with the restorative dentist or prosthodontist taking the lead, as it is they that are ultimately responsible for the long-term management and care of the patient.
- Poor oral hygiene
- Crestal bone stability over seven years
- Profuse suppuration
- A single radiograph cannot diagnose peri-implantitis
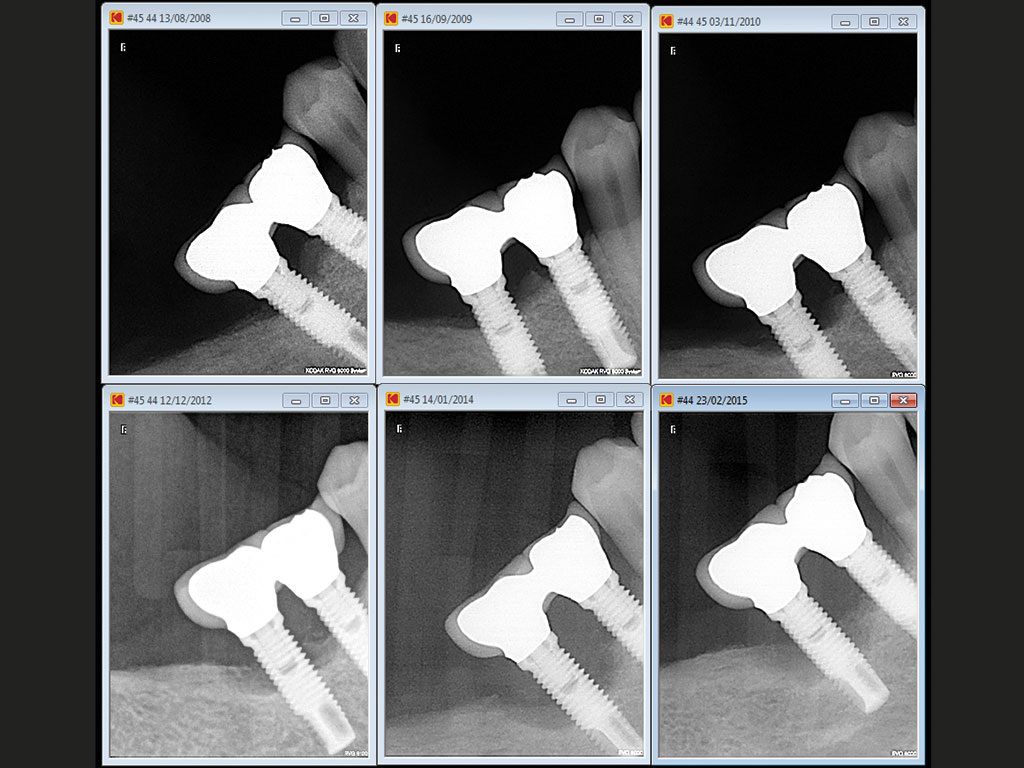
- Bone loss radiographic series after maturation phase 2008-9
- Progressive bone loss after maturation phase surgical debridement was carried out in 2009 bone loss continued
- Despite visible threading and poor oral hygiene this is not perimplantitis without progressive bone loss
Proposed guidelines for follow-up of implants
In current practice, clinicians are challenged to provide a high level of care often within the constraints of a system which does not recognise the time/effort and expense required in providing it.
What is needed are simple diagnostic tools which can be integrated into routine daily practice, taking a minimum of time and providing a high degree of accuracy. Current implant maintenance advice does the opposite of this. Bleeding on probing and pocket charts take time and, as we now see, have a very low level of predictive accuracy.
Based on the current degree of knowledge, the most reasonable approach is that implant patients should be examined annually for the presence of clinical problems. The clinical examination should cover three areas:
Observation – absence of redness and swelling in the soft tissues, assessment of adequate plaque control4 and assessment of the occlusal scheme (paying particular attention to the possibility of parafunction and the excessive loads this may transfer to the restorations and implants)
Palpation – pressure on the tissues surrounding the implant to ensure absence of discomfort, bleeding and suppuration (see Fig 3)
Radiation – radiographs should be taken once a year during the first two to three years of function and thereafter at regular intervals (every two or three years, depending on the findings of the clinical examination and on the individual patient’s oral hygiene and co-operation) to monitor the crestal bone level stability.
It should be kept in mind that a stand alone radiograph after baseline radiography is insufficient to diagnose “disease” (Fig 4). To diagnose peri-implant health or disease, a series of radiographs from different times of follow up is needed to decide whether a particular implant has progressive loss of marginal bone (Figs 5a and 5b). Furthermore the “series” of radiographs only starts after the maturation/ adaptive phase of one year5.
Only significant, progressive loss of marginal bone, as verified in the series of radiographs, in association with clinical signs of inflammation such as redness, swelling, bleeding and suppuration at palpation and pressure on the soft tissues (not at probing) should be considered indicative of an ongoing peri-implantitis process (Fig 5c).
- FIGURE 6 – Radiographic series showing progresssive bone loss around three out of four implants
- FIGURE 7 – Clinical picture at completion of treatment
- FIGURE 8 – Surgical debridement of granulation tissue to attempt to treat suppurative infection
- FIGURE 9 – Clinical picture after healing
- FIGURE 10 – At presentation
- FIGURE 11 – Radiographic series showing stability of bone despite significant loss round implant and adjacent tooth
- FIGURE – 12 Remaining teeth and ailing implant removed and replaced for fullarch restoration
- FIGURE 13 – New baseline radiograph
- FIGURE 14 – Implant removal tool in failed implant
- FIGURE 15 – Failed implant counter rotated out to break osseointegration
Clinical aspects of true peri-implantitis lesions
True peri-implantitis lesions do of course exist, all be it in a thankfully smaller number that some might think, with an incidence of only 2.7 per cent 5. Peri-implantitis constitutes a threat to the longevity of the implant due to rapid marginal bone loss. Characteristic symptoms are, as outlined above: swelling, redness, pain and suppuration when palpating the peri-implant soft tissues in addition to the presence of rapid marginal bone loss.
The pathology of the development of a peri-implantitis lesion is not well understood. A primary peri-implantitis lesion has yet to be recognised and treatment is usually of the secondary infection which presents clinically. It is postulated that marginal bone resorption, for any reason, may have provided the conditions for a secondary infection with anaerobic bacteria, which in turn accelerates the tissue damage 2,6.
Treatment therefore should be aimed at resolving the presenting infection. This can include the use of local antibacterial rinsing, general treatment with antibiotics and surgical exploration of the area (Figs 6, 7, 8, 9).
There are, in addition, a number of innovative approaches to the surgical management of peri-implantitis lesions proposed:
- Laser treatment of cleaned implant surface
- “Implantoplasty” to attempt smoothing of the implant surface
- Use of antibiotics mixed with biomaterials to promote healing and soft tissue reattachment to the implant
- Soaking of the implant with various solutions after mechanical cleaning.
- While all these techniques show occasional impressive results to justify their use, it should be remembered, in the context of this and the previous article, that:
The diagnostic tools dictating treatment are poor and may have resulted in treatment of implants that did not actually have true peri-implantitis lesions, in which case there is little to be learned
In such cases there are no controls or long-term outcomes – these are low evidence techniques and do not justify routine practice
Surgical treatment of peri-implantitis is unpredictable whatever the method7.
As stated before, the pathology of a true peri-implantitis lesion is poorly understood. Even if the secondary infection is managed effectively, the cause of the original bone loss may still be present and continue to affect marginal bone levels. It is important, therefore, that all the potential compromising factors are also addressed (patient/surgeon/restorative).
Occasionally, bone loss results in the exposure of a large portion of the implant, deeming it unaesthetic, impossible to clean and a constant irritation for the patient. In such situations, if it has not already lost integration, removal of the implant should be considered. Implant failure is no longer a terminal event, in contrast to losing a tooth, as a new implant can be placed if a sufficient amount of bone is present. The replacement implant does not seem to be significantly worse off than any new implant might be.
Osseointegrated implants can now be removed in an atraumatic way by using a so-called removal tool. With this new development, removal of “ailing” implants can be carried out and treatment started anew, rather than lengthy, unpredictable surgical “management” (Figs 10-15).
Conclusions
There is still a lot that we do not know about peri-implantitis and hopefully future research will provide us with accurate diagnostic indicators of health and treatment needs, together with predictable management techniques. Until such a time, we need to approach peri-implant problems with a measured and pragmatic approach, assessing each case on its clinical presentation and deciding on a course of action that is best for that patient at that time.
References
1. Coli P, Christiaensen V, Sennerby L, De Bruyn H. Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontology 2000 Vol 73, 2017, 203-217.
2. Qian J, Wennerberg A, Albrektsson T. Reasons for Marginal Bone loss around Oral Implants. Clin Implant Dent Relat res 2012:14: 792-807.
3. Bryant SR. Oral implant outcomes predicted by age and site specific aspects of bone condition. PhD Thesis Department of Prosthodontics, University of Toronto, Canada 2001.
4. Attard N. Zarb G. Long term treatment outcomes in edentulous patients with implant-fixed prostheses: the Toronto study. Int. Journal Pros 2004:17:4.
5. Albrektsson T, Buser D, Sennerby L. Crestalbone loss and oral implants. ClinImplant Dent Relat Res 2012: 14: 783–791.
Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? ClinImplant Dent Relat Res 2014: 16: 155–165.
Listl S. Tu Y. Assessment of endpoints in studies on peri-implantitis treatment – A systematic review. Journal of Dentistry 2010: 38: 443-450.
About the authors
Dr Kevin Lochhead is a specialist in prosthodontics and principal dentist at Edinburgh Dental Specialists. He qualified from Kings College London in 1987.
Dr Pierluigi Coli is a specialist in periodontics and prosthodontics at Edinburgh Dental Specialists. He graduated with honours in dentistry at the University of Genova, Italy in 1990. He was trained in periodontology, dental implantology and prosthodontics in the prestigious Departments of Periodontology, of Oral Rehabilitation/Branemark Clinic and of Prosthetic Dentistry/Oral Material Sciences, Faculty of Odontology, University of Gothenburg, Sweden, where he specialised
and worked during the years 1993-2007.
Professor Lars Sennerby is a visiting professor in implantology at Edinburgh Dental Specialists. He graduated from the Faculty of Dentistry, University of Gothenburg, Sweden in 1986. He joined the research group led by Prof P-I Branemark in 1982 and participated in studies on osseointegrated dental implants. In 1991 he was awarded a PhD for his thesis entitled “On the bone tissue response to titanium implants”. He was trained in oral surgery at the Branemark Clinic, Public Health Service and Faculty of Dentistry in Gothenburg and worked there part-time from 1989 to 2001.
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings















Comments are closed here.