Narrowing down the options
Long-term follow-up of 2.5mm narrow diameter implants in premolar and molar areas supporting a fixed prostheses by Eduardo Anitua
A narrow diameter implant is an implant with a diameter less than 3.75mm and is clinically indicated to replace maxillary lateral incisors and mandibular incisors1. The availability of interdental space less than 6mm and/or residual bone width less than 5mm are also indicative for the use of narrow diameter implant (NDIs)1.
NDIs have significantly reduced the need for bone grafting among completely edentulous patients2. This would permit the avoidance of complications associated with alveolar bone augmentation such as prolonged healing time, additional costs and increased surgical morbidity2, 4. In a recent study, Pommer et al. conclude that, while little evidence on patients’ preferences towards minimally invasive treatment alternatives as opposed to bone augmentation surgery could be identified from within-study comparison, patient satisfaction with graftless solutions for implant rehabilitation of completely edentulous jaws is generally high5.
Long-term survival of the narrow implants in posterior areas of the maxilla and mandible is not well documented. A recent study with this type of implants in areas with combination of split crest technique seems to indicate a successful implant survival rate (97 per cent)6.
Ortega-Oller et al. in a meta-analysis have shown that narrower implants (<3.3mm) have significantly higher failure rates than wider implants (≥ 3.3mm)7. This could be influenced by other variables such as type of prosthesis, implant surface, and timing of prosthetic loading7. Klein et al. in a recent systematic review reported that the survival rate of implants with a diameter < 3mm were higher than 90 per cent with a follow-up time of between one and three years8. For implants with a diameter between 3.0 and 3.25mm the survival rate was higher than 93.8 per cent (follow-up of one to five years). Those implants with a diameter ≥ 3.3mm had a survival rate of 88.9 per cent to
100 per cent with a follow-up time of one to 12 years. The most common causes of implant failure have been lack/loss of osseointegration and infection1, 9, 10.
From the above, NDIs have a comparable success rate as wider implants not only in the anterior region but also in the posterior regions.
For that, this study was conducted to analyse the long-term outcomes of using 2.5mm NDIs as definitive implant for rehabilitation of missing teeth in posterior areas.
Material and methods
This article was written following the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines11 and included patients treated at a single dental clinic in Vitoria, Spain. Patients included in the study fulfilled the following criteria:
- Both genders and over 18 years old
- Patients with totally or partially edentulous jaws who were treated by one or more 2.5mm narrow-diameter implants due to insufficient bone ridge thickness (< 5mm) and/or reduced mesio-distal space (< 6mm)
- Implants inserted before July 2005
- Implants inserted in posterior areas (premolar
and molar) - A retrospective cohort study design was used.
Data collection
Patient records were analysed to derive demographic data (gender, age), social habits (smoking, alcohol intake), relevant medical conditions, and history of periodontal disease. Then a database was conformed with implants data (length, diameter, and insertion torque) and localisation.
For implant survival assessment, implant failure was considered any implant lost due to biological (failure to achieve osseointegration or loss of acquired osseointegration) or biomechanical causes.
For Marginal Bone Loss (MBL) quantifications, marginal bone levels were measured on the periapical radiograph made just after the surgery and the last available periapical radiograph. The radiographs were obtained using paralleling technique with a film holder (Superbite, KerrHawe, Barcelona, Spain).
Measurements of MBL on the periapical radiographs were performed by computer software (Digora, Soredex, USA), a calibration of the periapical radiograph by a known length (implant length) was performed. Once the radiograph was calibrated to a 1:1 measure, eliminating the possible presence of magnification, measurements were made mesially and distally to the implants, calculating the distance between the uppermost point of the implant platform and the most coronal contact between the bone and the implant. The bone level recorded just after the surgical insertion of the implant was the basal value to compare with subsequent measurements over time.
For prostheses survival assessment, prostheses failure was considered as any complication that led to prosthesis removal (screw loosening/ fracture abutment/ implant fracture/ceramic chipping and prosthesis fracture).
Surgical procedures
All surgeries were made by two experienced surgeons. Before surgery, patients underwent a routine dental scaling to start the implant treatment with an adequate periodontal health. Radiographic evaluation was also performed to establish the treatment plan.
Patients received 2g of amoxicillin (600mg of clindamycin for allergic patients) 60 minutes before surgery and 1g of acetaminophen, 30 minutes preoperatively. Local anesthesia was achieved by the administration of articaine hydrochloride with epinephrine (1:100,000).
Implant sites were prepared using a low-speed drilling procedure (125 rpm) without irrigation12,13. Before installation, implants were carefully embedded in liquid Plasma Rich in Growth Factors prepared from patient’s blood according to a protocol developed by the manufacturer (PRGF-Endoret, Biotechnology Institute BTI, Vitoria, Spain) to bioactivate the implant surface.
Rehabilitations were made by the restorative dentist. In general, healing was allowed for a minimum of three months, after which the healing abutments were fixed. Shortly thereafter, the suprastructure was placed. Immediate loading protocol was applied in four patients (eight NDIs). Implants were loaded immediately only if they achieved an insertion torque of at least 45Ncm.
Post-surgical clinical assessments
Once the surgical phase was conducted, patients were scheduled for a series of periodic evaluations, consisting normally of: one evaluation five to 10 days after intervention, at one month, at three months, at six months, and from this moment ahead, once a year. The post-implant assessment included, at each follow-up visit, different clinical assessments to verify the status of the implant (gingival health, prosthesis mobility, pain, infection, alveolar ridge resorption and any complications).
Moreover, periodic panoramic and periapical radiographs were carried out to verify the implant clinical status in the follow-up period.
Statistical analysis
Data collection and analysis was performed by two independent examiners (other than restorative dentist and surgeon). The patient was the statistical unit for the statistical description of demographic data, social habits, medical history and history of periodontal disease. Mean values, standard deviations, and ranges were calculated for age, while relative frequency was calculated for the remaining patient-related variables.
The implant served as the statistical unit for the descriptions of implant length, diameter, location, insertion torque, marginal bone loss, survival an prosthetic parameters. Absolute and relative frequency distributions were calculated for qualitative variables and mean values and standard deviations for quantitative variables. The survival of implants and prostheses were evaluated with Kaplan-Meier method. SPSS v15.0 for Windows statistical software package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
In this study, a total of 25, 2.5mm narrow-diameter implants placed in 15 patients were included and evaluated. Eighty per cent of the patients were female and the mean age at surgery was 53 ± 9.2 years. Four patients were smokers (20 per cent). The length of the implants ranged between 11.5mm and 15mm. The implants mean follow-up time since insertion was 6.5 ± 3.9 years (range 0 to 9.5 years).
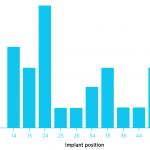
The mean follow-up time of the prostheses was 5.67 years (SD = 36.06). Figure 1 shows the anatomical locations of implants. Fifteen implants (60 per cent) were placed in the maxilla, whereas 10 were placed in the mandible (40 per cent).
Delayed implant loading was performed for 17 implants (68 per cent). The implant loading was performed after eight ± four months since insertion (range: five to 21 months). Five implants (32 per cent) were submitted to immediate loading protocol.
Regarding the type of the prosthesis, 12 implants (48 per cent) were involved in a fixed partial bridges, whereas 12 implants were involved in four screwed complete prostheses (48 per cent), and the one remaining implant was restored with a cemented single crown (4 per cent).
For the assessment of long-term MBL, only those cases where the last available periapical radiograph was performed after at least seven years of insertion were taken into account. Twenty one implants (mean follow-up time of 8.9 ± 0.5 years) that satisfied this requirement were analysed. The mean MBL was 0.64mm at the mesial side (SD = 0.64, range between 0 and 1.95mm), and 0.66mm (SD = 0.62, range between 0.00 and 2.19mm) at the distal side.
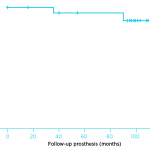
The survival rate was 100 per cent for implants. Two prostheses failed during the observation period. The prosthetic complications were porcelain fracture in another patient and connector fracture in other patient. This resulted in prostheses survival rate of 92.0 per cent (Figure 2).
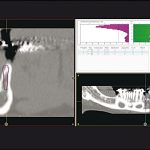
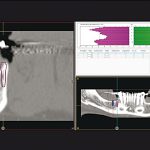
Figure 3 illustrates the clinical situation of a patient involved in the study before and after 10 years of treatment with narrow diameter implants.
- Figure 1. Anatomical location of the narrow diameter implants included in this study
- Figure 2. Cumulative survival rate of the prostheses
- Fig 3a. Post-operative X-ray at the moment of the insertion of the implants
- Fig 3b. Planning in the diagnostic software of the implant insertion
- Fig 3c. Planning in the diagnostic software of the implant insertion
- Fig 3d. X-ray with the final prosthesis at two years
Discussion
Eighty seven per cent of the implants were followed for more than three years and 60 per cent for more than seven years. During the follow-up period, no implants have failed resulting in a survival rate of 100 per cent. In a review, Renouard and Nisand reported an implant survival rate higher than 90 per cent for 3mm and 3.3mm implants14. Sohrabi et al. have similarly concluded that the survival rate of NDIs is generally higher than 90 per cent and that the failure rate appeared to be higher in small-diameter implants less than 13mm in length15. Klein et al. have reported that available studies on dental implants <2.5mm in diameter reported a survival rates between 90 and 100 per cent8.
In a recent meta-analysis by Ortega-Oller et al. the majority of the analysed studies (implants less than 3.3mm in diameter) have also reported a survival/success rate higher than 90 per cent7. However, the results of the meta-analysis have shown higher failure rates for implants with a diameter <3.3mm when compared to implants with a diameter ≥3.3mm. The authors have related this outcome with the fact that NDIs are usually placed in complicated clinical scenario and they have higher possibility of fracture7. Interestingly, according to that review, the failure rate will be more probable if the implants are loaded in a period less than three months since insertion and/or have a smooth implant surface7.
In the present study, the survival rate of NDIs was comparable to standard implants. The high survival rate of the NDIs could be related to the fact that the implants placed in this study had a roughened surface. Furthermore, 26 implants were loaded after eight months (± four months) since implant insertion and no one of these had failed.
Abutment screw loosening is one of the most common prosthetic complications that was being reported by clinical studies on NDIs8. This complication could be the result of different factors such as component misfit, inadequate tightening, settling of the screw, inadequate screw design and excessive loading16. The absence of screw loosening in this long-term follow-up could related to the fact that all implants (except one) were splinted by a fixed prostheses.
Splinting multiple implants has been reported to minimise the lateral force on the prosthesis, to enhance force distribution, and to reduce the stress on the implants17,18. Thus, splinting of 2.5-diameter implants would protect the implants from excessive loading and prevent implant/abutment screw fracture.
In this study, all the implants were inserted in posterior areas. In this type of rehabilitation, the risk of ‘fatigue’ fractures of the implants exists19,20. Freitas-Junior et al. have concluded in a biomechanical study that a single NDI is less reliable than a standard implant or two NDIs to support single crown in the molar region21. In our study, the survival of implants were 100 per cent and there were no biomechanical complications with the implants.
The measurement of marginal bone loss around the NDIs had a mean value below 1mm for the implants with follow-up time more than seven years since insertion. This would indicate the absence of excessive mechanical loading on the 2.5mm diameter implants. Similar results have been reported by Wang et al.22.
This study suffers from the limitation of a retrospective study design and the small sample size. The retrospective study provides evidence of lesser strength than the evidence derived from prospective or randomised clinical trial. There is also a dependency on the availability and accuracy of medical/dental records.
Conclusions
The use of narrow diameter implants in narrow alveolar ridges in posterior areas could constitute a minimally invasive alternative to bone augmentation surgery. NDIs of 2.5mm have resulted in a high survival rate in a long-term follow-up. This outcome could be related to the fact that these implants have all been splinted to other implants by a fixed prosthesis. This prosthetic configuration may have minimised the probability of implant and prosthesis failure.
References
1. Andersen E, Saxegaard E, Knutsen BM, Haanaes HR. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int J Oral Maxillofac Implants 2001; 16: 217-224.
2. Papadimitriou DE, Friedland B, Gannam C, Salari S, Gallucci GO. Narrow-Diameter versus Standard-Diameter Implants and their Effect on the Need for Guided Bone Regeneration: A Virtual Three-Dimensional Study. Clin Implant Dent Relat Res.
3. Anitua E, Alkhraisat MH, Orive G. Novel technique for the treatment of the severely atrophied posterior mandible. Int J Oral Maxillofac Implants 2013; 28: 1338-1346.
4. Esposito M, Cannizzaro G, Soardi E, Pellegrino G, Pistilli R, Felice P. A 3-year post-loading report of a randomised controlled trial on the rehabilitation of posterior atrophic mandibles: short implants or longer implants in vertically augmented bone? Eur J Oral Implantol 2011; 4: 301-311.
5. Pommer B, Mailath-Pokorny G, Haas R, Busenlechner D, Furhauser R, Watzek G. Patients’ preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. Eur J Oral Implantol 2014; 7 Suppl 2: S91-109.
6. Garcez-Filho J, Tolentino L, Sukekava F, Seabra M, Cesar-Neto JB, Araújo MG. Long-term outcomes from implants installed by using split-crest technique in posterior maxillae: 10 years of follow-up. Clin Oral Implants Res. 2015 Mar;26(3):326-31.
7. Ortega-Oller I, Suarez F, Galindo-Moreno P, Torrecillas-Martinez L, Monje A, Catena A, Wang HL. The influence of implant diameter on its survival: a meta-analysis based on prospective clinical trials. J Periodontol 2014; 85: 569-580.
8. Klein MO, Schiegnitz E, Al-Nawas B. Systematic review on success of narrow-diameter dental implants. Int J Oral Maxillofac Implants 2014; 29 Suppl: 43-54.
9. Polizzi G, Fabbro S, Furri M, Herrmann I, Squarzoni S. Clinical application of narrow Branemark System implants for single-tooth restorations. Int J Oral Maxillofac Implants 1999; 14: 496-503.
10. Zinsli B, Sagesser T, Mericske E, Mericske-Stern R. Clinical evaluation of small-diameter ITI implants: a prospective study. Int J Oral Maxillofac Implants 2004; 19: 92-99.
11. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453-1457.
12. Anitua E, Alkhraisat MH, Pinas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat.
13. Anitua E, Carda C, Andia I. A novel drilling procedure and subsequent bone autograft preparation: a technical note. Int J Oral Maxillofac Implants 2007; 22: 138-145.
14. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res 2006; 17 Suppl 2: 35-51.
15. Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res 2012; 23: 515-525.
16. Patil PG. A technique for repairing a loosening abutment screw for a cement-retained implant prosthesis. J Prosthodont 2011; 20: 652-655.
17. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent 2010; 30: 89-95.
18. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res 2003; 5: 254-262.
19. Chiapasco M, Casentini P, Zaniboni M, Corsi E, Anello T. Titanium-zirconium alloy narrow-diameter implants (Straumann Roxolid) for the rehabilitation of horizontally deficient edentulous ridges: prospective study on 18 consecutive patients. Clin Oral Implants Res 2012; 23: 1136-1141.
20. Davarpanah M, Martinez H, Tecucianu JF, Celletti R, Lazzara R. Small-diameter implants: indications and contraindications. J Esthet Dent 2000; 12: 186-194.
21. Freitas-Junior AC, Bonfante EA, Martins LM, Silva NR, Marotta L, Coelho PG. Effect of implant diameter on reliability and failure modes of molar crowns. Int J Prosthodont 2011; 24: 557-561.
22. Wang HL, Okayasu K, Fu JH, Hamerink HA, Layher MG, Rudek IE. The success rate of narrow body implants used for supporting immediate provisional restorations: a pilot feasibility study. Implant Dent 2012; 21: 467-473.
About the author
Eduardo Anitua DDS, MD, PhD graduated with a degree in medicine and surgery from the University of Salamanca and gained his PhD in medicine from the University of Valencia.
He holds a specialism in stomatology from the University of the Basque Country (UPV/EHU) and a diploma in prostheses and occlusion from the Pankey Institute (Florida, USA).
He is a visiting professor at more than 20 universities in the USA (Harvard, Boston, Tufts, Pennsylvania, New Orleans), Germany (Berlin), England (Bristol), Italy (Milan, Turin), India, Mexico, Brazil, Portugal, Argentina, Colombia, Venezuela, Uruguay and Spain (Seville, Madrid, Barcelona, Murcia).
Dr Anitua has published more than 200 papers in national and international journals, is the author of eight books and co-author of seven books and chapters translated into various languages. He has 37 international patents developed in regenerative therapy and oral implantology.
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings




Comments are closed here.