Canal cleaning
A review of the role of irrigation in contemporary root canal treatment
Apical periodontitis has been established to be a microbial-induced disease 1–3. The aim of root canal treatment is the prevention or treatment of apical periodontitis by the elimination of micro-organisms from the root canal system and the prevention of subsequent recontamination 4. To this end, our primary treatment modality is chemo-mechanical debridement of the root canal 5.
Mechanical cleaning of the root canal system with hand or rotary instruments has been shown to engage only a proportion of the root canal wall – 35 to 53 per cent of the canal wall surface may remain untouched following preparation 6. Fins, lateral anatomy and communicating canals render the goal of mechanical removal of all infected tissue impossible; therefore, after gross debridement of the vital and non-vital tissue from the canal, the main goal of mechanical preparation is to enable chemical disinfection of the root canal 7.
The functions of endodontic irrigation include:
Irrigant activation may be enabled either by manual or machine-assisted means
Adrian Stewart
- Disinfection
- Degradation of pulp tissue
- Disruption of the biofilm
- Removal of the smear layer
- Lubrication of endodontic instruments
- Flushing of debris from the canal.
In practice, no single irrigant achieves all of these aims and a combination regime is recommended. Saline and local anaesthetic have each been employed, but these provide only a flushing and lubricating function. Irrigation with such chemically inert media has been shown to be incapable of adequately reducing the viable microorganisms in infected root canal systems 5.
Irrigants in contemporary use can be classified as antimicrobial or decalcifying 4 (see table).
| Antimicrobial Irrigants |
|---|
| Sodium hypochlorite |
| Chlorhexidine |
| Electro-chemically activated water |
| Iodine-potassium-iodide |
| Hydrogen peroxide |
| Decalcifying irrigants |
|---|
| Ethylenediaminetetraacetic acid (EDTA) |
| Citric acid |
Mechanical instrumentation has been shown to result in the burnishing of organic material and dentine debris against the canal wall and into depressions and lateral anatomy 8. The role of decalcifying agents such as EDTA incudes chelation of the mineral content of this “smear layer” and the opening of access to the lateral anatomy 9.
Sodium hypochlorite
Sodium hypochlorite (NaOCl) is recommended as the main endodontic irrigant due its ability to dissolve organic tissue and its broad anti-microbial spectrum 9. Its action on organic tissue enables it to disrupt and kill biofilms adherent to the root canal walls.
Concentrations in use in endodontics range from 0.5 to 5.25 per cent.
Chlorhexidine
Chlorhexidine is a bisguanide, generally used in the form of chlorhexidine digluconate. As a root canal irrigant, it is generally presented in 2 per cent concentration. While several in-vitro studies have shown anti-microbial efficacy to be similar to sodium hypochlorite, some in-vivo studies have demonstrated chlorhexidine to be inferior, with more culture reversals from negative to positive between visits. This is likely to be due to its inability to dissolve pulpal remnants 10.
The major advantages chlorhexidine has over sodium hypochlorite are lower toxicity, less objectionable smell and taste and substantivity, meaning it persists on the walls of the canals. Like sodium hypochlorite, chlorhexidine lacks the ability to dissolve the smear layer 4.
Chlorhexidine should not be used in conjunction with sodium hypochlorite due to the formation of a precipitate or flocculate. This flocculate contains para-chloroaniline (PCA), which is known to be carcinogenic, although the level of exposure in such cases is likely to be low. The presence of the flocculate may lead to blockage of narrow anatomy and subsequently hinder adequate penetration of hypochlorite.
Alternative concepts for antimicrobial irrigation include electrochemically-activated water (eg. Sterilox), laser photo activated disinfection and ozone gas filtration of the root canal system. Studies comparing the antimicrobial efficacy these approaches to irrigation, with a 3 per cent sodium hypochlorite solution found all to be inferior to varying degrees 11–13.
Decalcifying agents
Although sodium hypochlorite has the ability to dissolve organic tissue, it cannot dissolve the inorganic component of dentine. Decalcifying agents such as EDTA and citric acid are recommended for dissolution of dentinal debris and removal of the smear layer from canal walls. In addition, inorganic obstructions to negotiation of the root canal during preparation may be overcome with the aid ofchelation agents 9.
It is not recommended that EDTA be used as an alternating rinse with sodium hypochlorite due to the deactivation of sodium hypochlorite by EDTA 14. It is recommended that EDTA be used as a penultimate rinse. The canal is dried of sodium hypochlorite and the EDTA is introduced and left in the canal for one minute. This is then rinsed out and the canal dried again before the final rinse with sodium hypochlorite. In this way, the smear layer is removed, opening the dentinal tubules and any lateral canals to penetration with hypochlorite.
There is clinical folklore that mixing sodium hypochlorite in the canal with EDTA and creating an acid-base reaction, the so-called “Champagne Effect”, aids with coronal transportation of debris. No evidence exists to support this claim 9.
Factors that influence the effectiveness of irrigation:
- Concentration of the irrigant
- Temperature of the irrigant
- Level of corono-apical penetration of the irrigant
- Volume of irrigant exchange.
Concentration
The antimicrobial and tissue dissolution capacity of sodium hypochlorite are both a function of its concentration, but so is its toxicity. Spangberg found that a 0.5 per cent solution of sodium hypochlorite was sufficient to kill most micro-organisms, with the exception of Staphylococcus aureus, and retained the ability to dissolve necrotic tissue, though not vital tissue. One per cent solution killed Staphylococcus aureus 15 and 5.25 per cent sodium hypochlorite has been found to reduce the elastic modulus and flexural strength of human dentine, while 0.5 per cent solution does not 16.
The risk of apical extrusion of sodium hypochlorite also militates against the use of unnecessarily high concentrations, although a concentration of 0.01 per cent has been demonstrated to be lethal to fibroblasts and a case of skin injury with exposure to 2.5 per cent following rubber dam leakage is recorded 17.
Rapid dissolution of vital and necrotic tissue remnants within the pulp canal is an essential facet of the use of sodium hypochlorite irrigant. No other irrigant has been shown to dissolve pulpal remnants in the same manner. It is, therefore, necessary to balance the needs for a higher concentration of hypochlorite with the caveat that higher concentrations are more likely to result in tissue damage if accidentally extruded through the apex or exposed to the mucosa. A concentration of 2.5 per cent is commonly used. An alternative to increased concentration has been experimented with ex-vivo as described below.
Temperature
Heating the hypochlorite solution has been shown to increase both its bactericidal and tissue dissolving effects. The capacity of a 1 per cent solution of sodium hypochlorite at 45ºC to dissolve human pulp tissue was found to be equal to that of a solution of 5.25 per cent at 20ºC 18. No clinical studies have been carried out to determine the applicability of this technique in-vivo, however; the benefit of using heated, weaker solutions of hypochlorite is that a temperature equilibrium is quickly reached within the root and extrusion or mucosal exposure is less likely to cause serious injury.
Corono-apical penetration
Root canal irrigants are conventionally delivered using a side-vented needle, fitting loosely in the canal. Side venting and loose fit are important to reduce the risk of apical extrusion of irrigant and to increase the flushing effect on debris. Vapour lock (a body of gas trapped in the apical portion of the root canal) means that penetration of the irrigant under such passive irrigation circumstances has been shown to be no more than 1mm beyond the tip of the needle 19. In order to increase the efficacy of the irrigation, it is vital to:
- Maximise the extent to which the needle can penetrate
- Activate the irrigant in order to increase the penetration of the root canal.
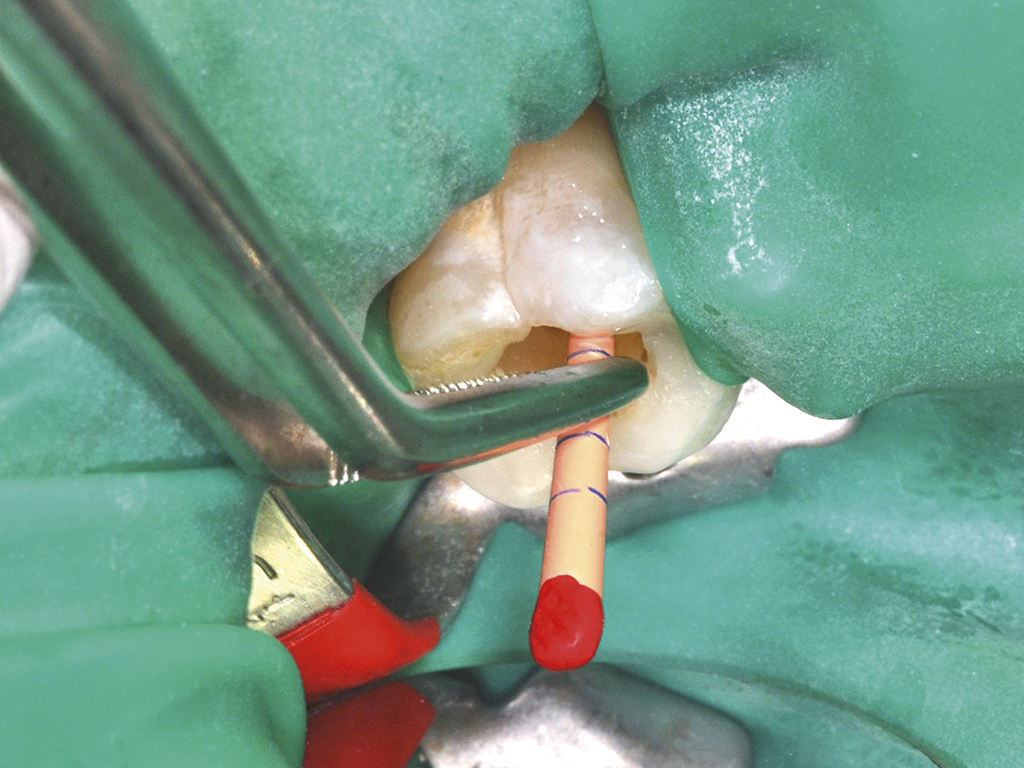
The needle penetration is a function of both the size of the needle and the size of the apical preparation of the canal. Apical preparations in the order of ISO size 25-30 and the use of currently available 27-30 gauge needles will enable penetration to approximately 1mm from Working Length (Figure 1). This has been found by at least one study to be the most dominant factor in irrigant penetration 20.
The preparation taper has also been found to affect irrigant exchange, with apical preparations of greater taper producing greater flow of irrigant than narrow tapers 21.
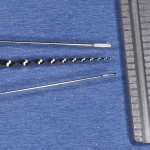
Irrigant activation may be enabled either by manual or machine-assisted means. Manual techniques include agitation with the delivery needle, use of endodontic brushes or by manual dynamic irrigation. In this technique, a well-fitting gutta percha cone is placed into the irrigated canal and moved rapidly in and out with a 2-3mm stroke. This action is thought to create a hydrodynamic effect increasing the penetration and exchange of the reagent 20. A drawback of manual pumping is that it is laborious (Figure 2).
Machine-assisted agitation systems have come about to facilitate better penetration. Rotary brushes, such as Canalbrush, can be used in a handpiece but, again, only where the brush can penetrate.
Quantec-E provides continuous irrigation during rotary instrumentation. This concept should provide for greater irrigant exchange than needle irrigation alone and this has been shown to be true in the coronal third of canals; however, this has not resulted in cleaner canal walls in the middle and apical thirds of canals studied 22.
Sonic agitation devices, such as the Endoactivator from Dentsply, work at lower frequencies than ultrasonic devices and demonstrate higher amplitudes of displacement. Endoactivator utilises a smooth-sided polymer tip that has been demonstrated to be resistant to fracture and passive towards the dentinal walls of the canal (Figure 3).
Passive ultrasonic irrigation (PUI) has been demonstrated to be highly effective in increasing both the penetration and cleaning efficiency of irrigant solutions. Although PUI can be used with intermittent irrigation, it has been demonstrated to be most effective when applied to the completed canal preparation 9. The prepared canal is flooded with irrigant such as sodium hypochlorite. A file is then introduced to the maximum length at which it does not bind with the canal walls and activated with an ultrasonic unit. With the file tip free, a node of vibration is established, generating a wave of energy that streams irrigant coronally. Endosonore files are highly effective for this technique (Figure 4).
While passive irrigation with sodium hypochlorite does not remove the smear layer, when a 3 per cent solution of sodium hypochlorite is used with PUI, several studies have found complete removal of the smear layer 23–24. These findings were not reproduced when the irrigant was replaced with saline.
The precise mode of action of PUI is unclear, but acoustic streaming is thought to be the primary factor in debris removal. Cavitation has also been postulated as an effect. Cavitation occurs with the generation and collapse of microbubbles within the irrigant solution as the pressure drops momentarily below the liquid’s vapour point. This has been shown to generate high temperatures in the micro-environment and may explain the synergistic effect of PUI and sodium hypochlorite 25.
Pressure alternating devices
Devices have been introduced that create alternating negative pressure and positive irrigation within the canal. Examples include EndoVac and RinsEndo. A study of one of these systems (RinsEndo) found that it outperformed passive irrigation in the removal of a layer of stained
collagen from the canal walls but was inferior to manual dynamic irrigation 26.
Summary
Despite attempts to create alternative solutions and methods, the evidence supports a regime that involves:
- A solution of sodium hypochlorite with a concentration in the range 1 per cent to 3 per cent
- The use of a decalcifying agent to remove the smear layer
- Ultrasonic activation of the irrigant
- Adequate apical preparation and taper of the canal to permit placement of the irrigant within 1mm of the apex and enable sufficient irrigant flow.
Figure 5 shows two completed cases demonstrating accessory anatomy that is not accessible to files, but which has been cleaned by irrigant penetration.
- Figure 1 – Top: A 27G cutaway irrigation needle. Bottom: A 30G side-ported needle. Middle: A Protaper F2 rotary file for comparison
- Figure 2 – A well-fitting GP cone can be used in a rapid pumping motion for manual dynamic irrigation
- Figure 3 – The Endo Activator from Dentsply
- Figure 4 – An endosonic file in its adaptor
- Figure 5 – Two teeth with accessory anatomy that has been cleaned by the reagent regime, not filing
About the author
Adrian Stewart BDS, PG Dip Endo (UCL), MSc, graduated from Queen’s University, Belfast in 1992. He holds an MSc in Clinical Dentistry (restorative dentistry) from Leeds University and the Post Graduate Diploma in Endodontic Practice from the Eastman Institute, UCL. Adrian works in practice limited to endodontics, taking referrals for non-surgical and surgical endodontics at 1 Manor Place, Edinburgh.
References
- Kakehashi S, Stanley HR, Fitzgerald RJ. The Effects of Surgical Exposures of Dental Pulps in Germ-Free and Conventional Laboratory Rats. Oral Surg Oral Med Oral Pathol. 1965 Sep;20:340-9.#
- Moller AJ, Fabricius L, Dahlen G, Ohman AE, Heyden G. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res. [Research Support, Non-U.S. Gov’t]. 1981 Dec;89(6):475-84.
- Nair PN. Apical periodontitis: a dynamic encounter between root canal infection and host response. Periodontol 2000. [Review]. 1997 Feb;13:121-48.
- Excellence Cf. Root canal irrigants and disinfectants. Endodontics [serial on the Internet]. 2011; Winter.
- Bystrom A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res. 1981 Aug;89(4):321-8.
- Gulabivala KP, B.; Evans, G.; Ng, Y-L. Effects of mechanical and chemical procedures on root canal surfaces. Endodontic Topics. 2005;10:103-22.
- Hulsman MP, O.A.; Dummer, P.M.H. Mechanical preparation of root canals: shaping goals, techniques and means. Endodontic Topics. 2005;10:30-76.
- Hulsmann M, Rummelin C, Schafers F. Root canal cleanliness after preparation with different endodontic handpieces and hand instruments: a comparative SEM investigation. J Endod. [Comparative Study]. 1997 May;23(5):301-6.
- Zehnder M. Root canal irrigants. J Endod. [Review]. 2006 May;32(5):389-98.
- Ringel AM, Patterson SS, Newton CW, Miller CH, Mulhern JM. In vivo evaluation of chlorhexidine gluconate solution and sodium hypochlorite solution as root canal irrigants. J Endod. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S.]. 1982 May;8(5):200-4.
- Seal GJ, Ng YL, Spratt D, Bhatti M, Gulabivala K. An in-vitro comparison of the bactericidal efficacy of lethal photosensitization or sodium hyphochlorite irrigation on Streptococcus intermedius biofilms in root canals. Int Endod J. [Comparative Study]. 2002 Mar;35(3):268-74.
- Gulabivala K, Stock CJ, Lewsey JD, Ghori S, Ng YL, Spratt DA. Effectiveness of electrochemically activated water as an irrigant in an infected tooth model. Int Endod J. [Comparative Study]. 2004 Sep;37(9):624-31.
- Hems RS, Gulabivala K, Ng YL, Ready D, Spratt DA. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. [Comparative Study Evaluation Studies Research Support, Non-U.S. Gov’t]. 2005 Jan;38(1):22-9.
- Rossi-Fedele G, Dogramaci EJ, Guastalli AR, Steier L, de Figueiredo JA. Antagonistic interactions between sodium hypochlorite, chlorhexidine, EDTA, and citric acid. J Endod. 2012 Apr;38(4):426-31.
- Spangberg L, Engstrom B, Langeland K. Biologic effects of dental materials. 3. Toxicity and antimicrobial effect of endodontic antiseptics in vitro. Oral Surg Oral Med Oral Pathol. [Comparative Study In Vitro]. 1973 Dec;36(6):856-71.
- Sim TP, Knowles JC, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. [Clinical Trial Comparative Study Randomized Controlled Trial]. 2001 Mar;34(2):120-32.
- Serper A, Ozbek M, Calt S. Accidental sodium hypochlorite-induced skin injury during endodontic treatment. J Endod. [Case Reports]. 2004 Mar;30(3):180-1.
- Sirtes G, Waltimo T, Schaetzle M, Zehnder M. The effects of temperature on sodium hypochlorite short-term stability, pulp dissolution capacity, and antimicrobial efficacy. J Endod. [Evaluation Studies]. 2005 Sep;31(9):669-71.
- Ram Z. Effectiveness of root canal irrigation. Oral Surg Oral Med Oral Pathol. 1977 Aug;44(2):306-12.
- Bronnec F, Bouillaguet S, Machtou P. Ex vivo assessment of irrigant penetration and renewal during the final irrigation regimen. Int Endod J. 2010 Aug;43(8):663-72.
- Boutsioukis C, Gogos C, Verhaagen B, Versluis M, Kastrinakis E, Van der Sluis LW. The effect of root canal taper on the irrigant flow: evaluation using an unsteady Computational Fluid Dynamics model. Int Endod J. [Comparative Study Research Support, Non-U.S. Gov’t]. 2010 Oct;43(10):909-16.
- Setlock J, Fayad MI, BeGole E, Bruzick M. Evaluation of canal cleanliness and smear layer removal after the use of the Quantec-E irrigation system and syringe: a comparative scanning electron microscope study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. [Clinical Trial Comparative Study Randomized Controlled Trial]. 2003 Nov;96(5):614-7.
- Cameron JA. The use of ultrasound for the removal of the smear layer. The effect of sodium hypochlorite concentration; SEM study. Aust Dent J. [Research Support, Non-U.S. Gov’t]. 1988 Jun;33(3):193-200.
- Alacam T. Scanning electron microscope study comparing the efficacy of endodontic irrigating systems. Int Endod J. [Comparative Study]. 1987 Nov;20(6):287-94.
- van der Sluis LW, Versluis M, Wu MK, Wesselink PR. Passive ultrasonic irrigation of the root canal: a review of the literature. Int Endod J. [Review]. 2007 Jun;40(6):415-26.
- McGill S, Gulabivala K, Mordan N, Ng YL. The efficacy of dynamic irrigation using a commercially available system (RinsEndo) determined by removal of a collagen ‘bio-molecular film’ from an ex vivo model. Int Endod J. 2008 Jul;41(7):602-8.




Comments are closed here.