Management of traumatic injuries
Dr Robert Philpott argues that a strict adherence to biological principles and a common sense approach is key when dealing with trauma patients
Literature on the management of dental trauma in general practice suggests that difficulties may be encountered due to gaps in knowledge and a lack of training on the subject.
Barriers to providing this care include lack of time, lack of confidence in diagnosis and inadequate remuneration (Hamilton et al 1997, Stewart and Mackie 2004, Jackson et al. 2005, Hu et al. 2006). Coupled with this is the fact that these patients may present relatively rarely in practice, adding to the stresses associated with management.
The keys to managing traumatic injuries involve correct technical management underpinned by a sound knowledge of the biological processes at play. This incorporates detailed history-taking, prompt emergency management and structured long-term follow-up to deal with the delayed complications often encountered.
Often, our dilemma as clinicians is between allowing an injured pulp every chance to exhibit signs of recovery while not delaying our treatment for too long
Dr Robert Philpott
How, what, when, where?
Initial interview of the patient must focus on any potential head injury, with emphasis on whether there has been a loss of consciousness. Often, many patients may have attended a local emergency department for immediate management prior to presentation at a dental practice.
One of the primary goals of immediate patient management is reassurance. History taking should begin with questioning of the patient in relation to how the injury occurred. The patient should be allowed to give their version of events with minimal interruption from the clinician. This component of the history may be especially important if there are any criminal or civil proceedings which may follow.
Interview in relation to the type of injury the patient has suffered may begin to shed light on the severity of the injury and the tissues involved. It is important to ask the patient what they feel has happened to their teeth i.e. whether the teeth are broken or not and whether there have been any alterations to the occlusion. History-taking should encourage the patient to use their own words to describe the injuries. Examination of previous photographs may shed light on the pre-operative situation. Interestingly, Dental Trauma UK, a new charity recently founded in the UK, has recommended that clinicians encourage the general public to join the “selfie” craze, taking a photograph of their smile, thereby providing invaluable information for the clinician managing a dental trauma.
The time elapsed since the injury may have an effect on pulpal and periodontal ligament survival and influence our decision-making in relation to the treatment we choose. Re-implantation of an avulsed tooth may not be possible if an extended time has passed since the injury due to clot formation and remodelling of the socket.
The site of the injury may influence our decision on whether the patient will need tetanus prophylaxis although, as aforementioned, this may often have been dealt with in a hospital setting. The site of the injury may also need to be searched for any missing tooth fragments, while cleaning of avulsed teeth contaminated with any gross debris will need to be completed before an attempt at re-implantation.
Immediate management
A traumatic injury to the dentoalveolar complex is an upsetting and worrying injury to any patient. It can also be a stressful occurrence for the dentist which, thankfully, may present relatively rarely in general practice.
Patients often present with multiple soft and hard tissue injuries and, in the first instance, it can be difficult to identify and diagnose the injuries. A calm approach is essential at this early stage, both to reassure the patient and to avoid missing any important detail during this initial examination (Fig 1).
The emergency management should commence with cleaning of the injured site. This can readily be accomplished using some sterile gauze soaked in chlorhexidine. It is wise to avoid using compressed air and water from the “3 in 1” syringe in the first instance to avoid startling an already nervous patient and to avoid disruption of the injured soft tissues. Although rare, this may lead to introduction of air into the soft tissues leading to a surgical emphysema.
Initial assessment of the injured site should be done by visual inspection, noting any malposed and fractured teeth, with attention paid to any previous treatment which may have been carried out. This should be followed by careful digital palpation of the site, taking care to identify any step deformities or mobility of the alveolar bone. This may be indicative of luxated teeth or fracture of the alveolar bone. Priority should always be given to treatment to encourage bony union during healing as the consequences of poor healing can be catastrophic.
Imaging
Radiographs are an essential tool in the diagnosis of dental trauma and a decision on which types and angles must be taken at the initial assessment appointment. As a rule of thumb, periapical radiographs of the maxillary anterior teeth (3-3) should be taken following a moderate injury to the maxillary anterior teeth. A decision on whether to take radiographs of the corresponding mandibular teeth can be taken depending on the results of the clinical examination and the perceived severity of the injury. Location of tooth fragments within the soft tissues is best done using a combination of digital palpation along with reduced exposure of a large periapical film. More recently, cone beam CT has been used in the diagnosis of traumatic injuries, offering the advantage of three dimensional assessment of displaced and injured teeth (Patel et al. 2007). This can offer great benefit in the case of dentoalveolar fractures and luxated teeth, often difficult to identify on standard periapical radiographs.
Classification of injuries
Classification of dental trauma is often complicated by the concomitant injury of multiple tissues. A thorough understanding of the tissues at risk of injury is critical to facilitate correct diagnosis and management of these injuries. As aforementioned, priority should be given to the treatment of any bony injury in order to minimise the risk of more severe complications later. A proposed classification of traumatic injuries in increasing order of severity is shown in Table 1.
Table 1
A proposed classification of traumatic injuries in increasing order of severity| INJURY | DESCRIPTION | PRESENTATION | TREATMENT |
|---|---|---|---|
| Enamel +/- dentine fracture | Fracture of enamel and/or dentine | Fractured tooth | Protect pulp and restore |
| Concussion | No movement of tooth | Tooth TTP | Monitor |
| Subluxation | Movement of tooth without displacement | Tooth TTP and possible bleeding from sulcus | Monitor |
| Lateral luxation | Tooth displaced | Incorrect position of tooth/occlusal discrepancy | Reposition, splint and review |
| Intrusion | Tooth forced into socket | Infra-occluded or "disappeared" tooth | Depends on severity/stage of development |
| Extrusion | Tooth forced outwards from socket | Tooth appears longer than adjacent teeth | Reposition, splint and review |
| Avulsion | Tooth completely removed from socket | Tooth no longer in place/in storage medium/missing | If available, clean, re-implant and splint |
| Dentoalveolar fracture | Fracture of bony housing | Mobility of whole bony segment if severe | Splint and review |
Repositioning and splinting
Adequate anaesthesia must always be achieved prior to any clinical intervention post trauma. This is essential to allow for adequate manipulation of injured tissues and to avoid adding to the patient’s stress. Repositioning of luxated teeth should begin with an understanding of how the injury has occurred and how this may have altered the position of the root within the alveolar housing. Frequently, the apices of luxated teeth may be “locked” into the alveolar bone.
Re-positioning, therefore, requires a firm but controlled force on the alveolar bone in order to manipulate the tooth into position. A clicking sound is often heard when this is done correctly. Palpation of the overlying soft tissues afterwards to assess labial contour helps to confirm this.
It is imperative in the case of avulsed teeth that they are first gently cleaned under running water while holding the tooth by the clinical crown. This ensures removal of any gross debris prior to an attempt at re-implantation. Storage medium and extra-oral dry time are two critical prognostic factors in the outcome following avulsion injuries, with literature suggesting the risk of replacement resorption being much higher in those teeth with a dry time of greater than 60 minutes (Andreasen 1981, Andersson et al. 1989). Patients should also be advised to store avulsed teeth in either milk or saliva (possibly even intra-orally) as opposed to in water. Ideally, an attempt at re-implantation should be made immediately although this may prove difficult in terms of positioning and angulation for those not familiar with the situation. Other storage media (Khademi et al. 2008) have also been proposed. However, they may not be readily available at the time of injury (Figs 2 and 3).
A variety of splinting protocols have been proposed for the stabilisation of injured tissues (Table 2).
Basic biological principles should be adhered to when fabricating a chairside splint. Wire-composite splinting is most commonly used and adheres to these principles if placed correctly. Guidelines previously recommended utilisation of rigid and non-rigid splints for different injuries but this has now been replaced by a protocol of non-rigid splinting for all injuries, of varying duration. This usually takes the form of an 0.16 Ni-Ti orthodontic archwire, although newer products on the market may supersede this (Fig 4).
Care should be taken initially to pre-bend the wire where possible to adapt it well to the labial surfaces of the injured and supporting teeth. This avoids application of an orthodontic force to the region. Teeth should be spot etched at the mid-labial aspect and a small amount of bonding agent added with the tip of a probe. Over zealous application of bonding agent results in difficulties in the removal of excess composite at the splint debond appointment. This may have obvious implications for direct physical trauma and potential heat transfer to an already injured pulp.
Composite should be placed at the mid-labial aspect of the teeth, well clear of the gingival margin and should be polished to avoid any overhangs, which may act as a plaque trap and a source of irritation to the patient. Splinting of teeth by direct composite union should be avoided due to its rigid nature, difficulties in maintaining oral hygiene and in removal.
Table 2
A variety of splinting protocols have been proposed for the stabilisation of injured tissues| INJURY | TIME (weeks) | TYPE |
|---|---|---|
| Subluxation | 2 | Flexible |
| Lateral luxation | 4 | Flexible |
| Intrusion | 4 | Flexible |
| Extrusion | 2 | Flexible |
| Avulsion | 2 | Flexible |
| Root # | 4 weeks - 4 months | Flexible |
| Dentoalveolar # | 4 | Flexible |
Review protocol
A robust review protocol is essential in the management of these cases. Various timings have been suggested and a common sense approach should prevail. The necessity for regular review is dependent on the severity of the initial injury and the likelihood of healing complications later. In general, review should be arranged one week, two weeks, four weeks, three months and six months following the date of the injury although slight variations have been proposed to this.
The key to review of traumatic injuries lies in establishment of baseline readings at the initial appointment and subsequent repetition of the examination and recording of results. This can be aided by the development of a custom trauma screen for in-office dental software or a simple stamp for written records. This ensures that nothing is missed at review.
Care must be taken in the interpretation of the results of sensibility tests in the aftermath of these injuries. Literature has suggested that teeth presenting giving positive responses at the initial appointment have a better pulpal prognosis but a period of monitoring is essential before committing any tooth to root canal treatment. The only exception to this appears to be avulsed permanent teeth, in which treatment can be initiated immediately.
A common sense approach should be adopted towards repeat radiographic examination. Over-exposure of the patient by taking excessive numbers of radiographs is ill-advised both in terms of the ALARA (as low as reasonably achievable) principle and also in terms of diagnostic yield.
Splint removal based on the timings outlined above is best carried out by removing the composite from the injured tooth/teeth first. This allows for their assessment in terms of mobility prior to deciding on whether to debond the whole splint or not. This saves time and avoids subsequent manipulation of injured teeth (Fig 5).
Definitive endodontic treatment
A decision on the necessity and timing of endodontic treatment on traumatised teeth must be taken following comparison between the clinical and radiographic findings at the initial appointment and subsequent review.
Various literature proposes the strategy of waiting for a period of three months, during which pulp sensibility tests give negative responses prior to initiating root canal treatment on injured teeth. The obvious exception to this is in the case of an avulsed tooth with a closed apex. Root canal treatment is advised immediately in this situation although practically, clinicians may often delay this by one week. This allows the focus of the initial appointment to be on patient reassurance and emergency management. Additionally, healing of soft tissue injuries will have progressed well during that initial period.
Caution must be exercised in interpreting the results of pulp sensibility tests following a traumatic injury. The injured pulp may be in a state of ‘shock’ and may not respond positively to the stimulus applied. Equally, it is well documented that immature teeth may give erroneous results due to the lack of development of the pulpal neural network. A prolonged delay leading to necrosis of the pulp, however, may affect the outcome of root canal treatment and put the tooth at risk of catastrophic resorption.
Where possible, endodontic treatment should be commenced with the splint in place as this confers extra stability on the injured teeth during the procedure. This is usually limited to teeth which have suffered an avulsion injury due to the recommended splinting times (Table 2) and the timing of definitive treatment. It may also lead to difficulties in rubber dam placement, with the split dam technique in the isolation of multiple teeth being necessary.
Timely management of complicated enamel dentine fractures is essential to optimise the outcome. Depending on the duration of pulpal exposure, the goal must be maintenance of pulpal vitality in these cases. Any direct exposures should be capped using a slurry of non-setting calcium hydroxide and restored with a glass ionomer cement base followed by a composite restoration. While mineral trioxide aggregate (MTA) remains the gold standard material for pulp capping of posterior teeth, caution must be exercised in the use of both grey and white MTA in these cases as subsequent discolouration of the tooth may provide an aesthetic challenge in the future. Biodentine may provide a suitable alternative in non-load-bearing areas.
Endodontic access to injured teeth is often straightforward due to their anterior location and lack of complex anatomy. Care must be taken to design and position the access cavity correctly, ensuring that the pulp horns are included to allow for removal of necrotic debris and access for irrigant. This prevents subsequent discolouration of these teeth post-treatment. Access may prove much more difficult in the case of traumatised incisors which have undergone pulp canal obliteration (PCO). Several groups have reported that 4-24 per cent of teeth undergo these changes in response to traumatic injuries, while McCabe and Dummer (2012) highlighted a useful series of steps to follow clinically in the management of this clinical scenario.
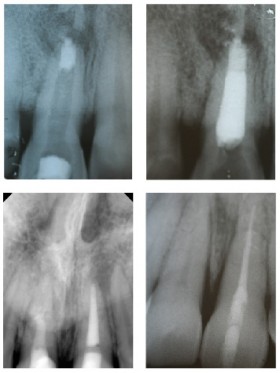
Instrumentation and irrigation of the root canal system should be carried out adhering to the biological principles of endodontic treatment. Difficulty may be encountered in determination of working length (WL) in teeth with open apices or in those with crowns and should be confirmed radiographically where doubt exists over the accuracy of the electronic apex locator (EAL) reading. Teeth suffering from horizontal root fractures should only be instrumented to the level of the fracture line and not beyond (Fig 6). The apical fragment of these teeth is almost always vital and unnecessarily instrumenting and obturating it poses difficulties for the clinician. Care must also be taken in the placement of the irrigation needle in close proximity to an open apex or root fractured tooth to avoid extrusion of sodium hypochlorite, the gold standard irrigant in such cases where dissolution of pulpal tissue is essential.
Various inter-appointment medicaments have been proposed for traumatised teeth with Ledermix showing promising results in the case of avulsed teeth (Bryson et al. 2002). This may not now be readily available in the UK and Odontopaste is proving to be a reliable alternative. In the case of other traumatic injuries, non-setting calcium hydroxide is advised.
Prior to the advent of MTA for the apexification (physical apical barrier formation) of immature teeth, long term dressing with calcium hydroxide was common. This proved to be a time consuming and unreliable method of barrier formation and potentially pre-disposed teeth to cervical fracture (Andreasen et al. 2002). MTA placement in these cases is best achieved using an apical placement system such as a Dovgan carrier or the Micro Apical Placement System by Dentsply.
Such devices simplify the technique and ensure placement of an adequate thickness of the material, while avoiding extrusion (Fig 6). The remaining canal is often best obturated using a thermoplasticised technique thereby minimising voids in the root filling.
More recently, case reports have emerged of revascularisation of teeth with open apices using combinations of antibiotics (Banchs and Trope 2004), combinations of irrigants (Shin et al. 2009) or simply sodium hypochlorite and EDTA, along with MTA. Results of these are promising, although doubts remain regarding the structure and origin of such regenerated tissue as it appears to be more similar to bone than pulpal tissue.
Discolouration of traumatised teeth may also pose problems in management. As aforementioned, care must be exercised to remove remnants of pulpal tissue from the pulp horns in access cavity design and the root filling material should always be compacted to a level 1mm below the cervical level of the tooth. This avoids subsequent discolouration from residues of root canal sealer and allows for correct placement of composite. The current protocol for non-vital bleaching of root-filled teeth dictates that bleaching agents containing a maximum of 6 per cent hydrogen peroxide are allowed. The “walking bleach” technique often results in acceptable aesthetic results for patients and clinicians alike.
- Multiple concomitant injuries to the dento-alveolar complex following a traumatic injury
- Photograph showing extent of displacement of coronal fragment following horizontal root fracture
- Same patient from Fig 2 following re-positioning and splinting.
- Titanium trauma splinting wire. Note spaces in wire which may facilitate placement of composite. (Image courtesy of Dr Chris Millen)
- Titanium trauma splinting wire. Note spaces in wire which may facilitate placement of composite. (Image courtesy of Dr Chris Millen)
- Patient from Fig 1 at one week review appointment. Note vast improvement in condition of soft tissues
- Series of radiographs showing definitive endodontic treatment of tooth 11 in patient following traumatic injury. Tooth 11 obturated using MTA plug apically and subsequent Obtura backfill. Final image shows tooth with horizontal root fracture filled through fracture line.
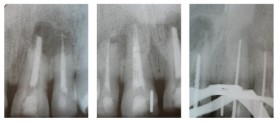
- Series of radiographs showing suboptimal root fillings in traumatised maxillary anterior teeth. Note signs of replacement and external inflammatory resorption.
Complications and prognosis
The biological complications following a traumatic injury to the dento-alveolar complex most frequently involve the pulp and the periodontal ligament (PDL). These healing complications are primarily a result of the extent of the injury (often the physical displacement of the tooth/teeth) and the efficiency with which we manage the injury.
Pulpal necrosis
While the severity of the initial injury is a prognostic factor for pulpal survival following trauma, the stage of development of the tooth is also important. Intuitively, we would assume that teeth with immature apices have a greater repair capability and this is borne out in the literature. Reports on pulpal revascularisation appeared in the literature as early as 1978 (Skoglund et al. 1978) and more recently, various protocols have been proposed in order to potentially regenerate injured and even partially necrotic pulps.
Literature suggests that the incidence of pulpal necrosis in permanent incisors is high in teeth suffering severe lateral luxation, intrusive and obviously avulsion injuries. In the case of horizontal root fractures, the degree of separation between the coronal and apical fragments often dictates whether the coronal pulp survives. In the case of an avulsed tooth,necrosis is almost certainly inevitable and endodontic treatment should be initiated within 10 days to limit the potential for associated complications.
Resorption
Dental resorption involves the removal of mineralised dental tissues and, according to Fuss et al. (2003), involves two distinct phases, injury and stimulation. In dental trauma cases, there are a number of categories of resorption which concern us and these are specifically related to certain injury types. In essence, resorption involves the loss of hard tissue while the unmineralised predentine and precementum remain protected. This protection of the predentine layer has been attributed to an unknown “protection factor” (Wedenberg 1987). While a detailed description of resorption is beyond the remit of this article, an outline of the types is given below.
Internal inflammatory resorption (IIR) may arise following a traumatic injury in the presence of a partially necrotic pulp. Bacterial contamination in the root canal system may act to stimulate an inflammatory response in the remaining pulpal tissues, with the subsequent loss of dental hard tissues. This presents as a ballooning radiolucency of the anatomy from the internal aspect of the root canal.
Infection may also act as a stimulus for external inflammatory resorption (EIR), with the dentinal tubules acting as a pathway for exit of bacteria and their associated by-products to the periodontium. These lesions present as radiolucencies at the lateral aspects of the root or in the apical region (Fig 7). Radiographically, the radiolucency is often superimposed over the root canal, with the lines of the root canal anatomy visible.
As the aetiology suggests, our management of these cases should focus on the removal of the infective stimulus which will halt the resorptive process. It is critical that we do not misdiagnose such cases or delay commencement of root canal treatment in traumatised teeth for too long, as the effects of the process can lead to devastating loss of hard tissues.
Often, our dilemma as clinicians is between allowing an injured pulp every chance to exhibit signs of recovery, while not delaying our treatment for too long. Importantly, not all types of resorption are as damaging and this often depends on the extent of the initial injury. In some trauma cases, we may see subtle signs of an EIR process which seems to self limit and cease over time.
Replacement resorption arises due to damage to the external surface of the root and is common after avulsion injuries, especially those teeth with a long extra-alveolar dry time or those that are mishandled (both in terms of manual handling and storage medium). This process essentially involves loss of dental hard tissue and subsequent replacement with bone. With injured teeth losing their aforementioned protective layer, bone resorbing osteoclasts begin this process of replacement resorption. Unfortunately, our knowledge of this disease process is limited and it may continue gradually until an entire root has been resorbed.
Various figures have been proposed to define the extent of replacement resorption needed to cause ankylosis of an injured tooth, with 20 per cent being suggested. Such teeth will, of course, lose their physiological mobility and have a high or metallic percussive tone. It is best to continue to monitor these cases and inform the patient of the likely complications which may arise in the future.
Conclusion
Management of injuries to the dentoalveolar complex involves strict adherence to biological principles and a common sense approach to the technical aspects of the treatment. Our approach at all times should be targeted at facilitating efficient healing of the tissues and allowing adequate time for this to occur. A regular and structured review protocol should be implemented with strict attention being paid to the possible healing complications, their appearance and the effect on prognosis.
About the author
Dr Robert Philpott, BDS MFDS MClinDent MRD (RCSEd), qualified from Cork Dental School in 2003 and completed his endodontic training at the Eastman in London in 2009. He has worked as a specialist in endodontics in Ireland, London and Australia. He currently divides his time working as a consultant in endodontics at Edinburgh Dental Institute and in private practice at Edinburgh Dental Specialists.
Further reading
Readers are directed to the following websites:
www.dentaltraumaguide.org
www.dentaltrauma.co.uk
References
- Andersson L, Bodin I, and Sorensen S. ‘Progression Of Root Resorption Following Replantation Of Human Teeth After Extended Extraoral Storage’. Dental Traumatology 5.1 (1989): 38-47. Web.
- Andreasen JO ‘Effect Of Extra-Alveolar Period And Storage Media Upon Periodontal And Pulpal Healing After Replantation Of Mature Permanent Incisors In Monkeys’. International Journal of Oral Surgery 10.1 (1981): 43-53. Web.
- Andreasen JO, Farik B, and Munksgaard EC. ‘Long-Term Calcium Hydroxide As A Root Canal Dressing May Increase Risk Of Root Fracture’. Dental Traumatology 18.3 (2002): 134-137. Web.
- Banchs F, and Trope M.‘Revascularisation Of Immature Permanent Teeth With Apical Periodontitis: New Treatment Protocol?’. Journal of Endodontics 30.4 (2004): 196-200. Web.
- Bryson EC, et al. ‘Effect Of Immediate Intracanal Placement Of Ledermix Paste On Healing Of Replanted Dog Teeth After Extended Dry Times’. Dental Traumatology 18.6 (2002): 316-321. Web.
- Fuss Z, Tsesis I, and Lin S. ‘Root Resorption – Diagnosis, Classification And Treatment Choices Based On Stimulation Factors’. Dental Traumatology 19.4 (2003): 175-182. Web.
- Hamilton FA, Hill FJ, and Holloway PJ. ‘An Investigation Of Dento-Alveolar Trauma And Its Treatment In An Adolescent Population. Part 2: Dentists’ Knowledge Of Management Methods And Their Perceptions Of Barriers To Providing Care’. Br Dent J 182.4 (1997): 129-133. Web.
- Hu LW, Prisco CRD, and Bombana AC. ‘Knowledge Of Brazilian General Dentists And Endodontists About The Emergency Management Of Dento-Alveolar Trauma’. Dental Traumatology 22.3 (2006): 113-117. Web.
- Jackson NG, Waterhouse PJ, and Maguire A. ‘Management Of Dental Trauma In Primary Care: A Postal Survey Of General Dental Practitioners’. Br Dent J 198.5 (2005): 293-297. Web.
- Jafarzadeh H and Abbott PV. ‘Review Of Pulp Sensibility Tests. Part I: General Information And Thermal Tests’. International Endodontic Journal 43.9 (2010): 738-762. Web.
- McCabe PS and Dummer PMH. ‘Pulp Canal Obliteration: An Endodontic Diagnosis And Treatment Challenge’. International Endodontic Journal 45.2 (2011): 177-197. Web.
- Mousav B et al. ‘Standard Oral Rehydration Solution As A New Storage Medium For Avulsed Teeth’. International Dental Journal 60.6 (2010): 379-382. Web.
- Patel S, et al. ‘The Potential Applications Of Cone Beam Computed Tomography In The Management Of Endodontic Problems’. International Endodontic Journal 40.10 (2007): 818-830. Web.
- Shin SY, Albert JS, and Mortman RE. ‘One Step Pulp Revascularisation Treatment Of An Immature Permanent Tooth With Chronic Apical Abscess: A Case Report’. International Endodontic Journal 42.12 (2009): 1118-1126. Web.
- Skoglund A, Tronstad L, and Wallenius K. ‘A Microangiographic Study Of Vascular Changes In Replanted And Autotransplanted Teeth Of Young Dogs’. Oral Surgery, Oral Medicine, Oral Pathology 45.1 (1978): 17-28. Web.
- Stewart SM, and Mackie IC. ‘Establishment And Evaluation Of A Trauma Clinic Based In A Primary Care Setting’. International Journal of Paediatric Dentistry 14.6 (2004): 409-416. Web.





2 Comments
Dear Sir or Madam,
I completed and submitted my answers to the CPD questions
in the March issue of Scottish Dental Magazine a number of weeks ago,but still haven’t received certification/notification of my results (successful or otherwise !) Have the results been checked/certificates been issued yet,as perhaps I have missed an email in amongst my other mail and it may be an oversight on my part ! Thank you for your
anticipated response to this query.
Norman Shiels
Hi Norman, thanks for getting in touch, the team are currently working on sorting all the CPD data to create the certificates for those who answered the quiz correctly, and will be in contact soon with your results.
SD